Temporomandibular joint dysfunction is a pathological process that is caused by changes in the jaws, articular surfaces and muscle tissue. In this case, uncoordinated movement of both jaws in relation to each other is diagnosed with clear signs of a violation of static and dynamic occlusion. The pathology occurs quite often, accounting for about 75% of all patients in dental offices. Many oral diseases are a consequence of TMJ dysfunction. Also, nearby organs and tissues are involved in the destructive process, which complicates its clinical signs with additional symptoms.
Specialists usually diagnose a chronic form of pathology in the temporomandibular joint, which in some cases accompanies a person for many years and is compensated by other components of the maxillofacial apparatus. Without therapeutic measures, complete or partial ankylosis may occur; therefore, a timely visit to the dentist will prevent impaired chewing function, visual unattractiveness and many other problems, the development of which can be caused by TMJ dysfunction.
Definition of temporomandibular joint
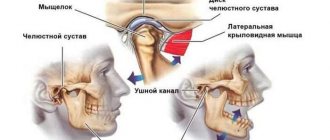
The temporomandibular joint is a fairly mobile joint that connects the lower jaw and the temporal bone, located on either side of the skull, in front of the ears.
This hinge joint provides the following functions:
- sedate jaw movements characteristic of conversation;
- maximum opening of the mouth, for example, when yawning;
- movement of the jaw during chewing.
The main assistants to the joints of the maxillofacial apparatus are the masticatory muscles, which help keep the lower jaw in the correct anatomical position, while easing the load on it.
Diagnosis and treatment methods
Modern methods used to identify the primary source that caused the development of pathology involve a set of procedures, which include radiography, CT and CBCT, PCR and DFA diagnostics. The key feature that distinguishes arthritis from other diseases is changes in the structure of the joint space (widening in the acute form and narrowing in the chronic form), as well as the formation of marginal lesions.
The treatment cycle involves immobilization of the joint for several days - a state of rest, combined with the use of compresses and painkillers, allows to reduce the load and relieve pain. Further recovery includes physical therapy using myogymnastics and electrophoresis, sanitation and local prosthetics. For the purulent form, a prerequisite is opening and cleaning the joint cavity.
Causes of dysfunction of the temporomandibular joint
Modern dentistry has facts that have not been fully studied about the causes of pathologies of the temporomandibular joint. However, based on the available data, experts suggest that the main problem lies in the destructive processes of the muscles and altered components of the joint itself.
Orthodontists identify the following pathologies and situations as the main causes and provoking factors for impaired mobility of the joint connecting the lower jaw (mandible) and the temporal bone:
- trauma to the lower jaw, which can provoke a violation of static and dynamic occlusion;
- damage to the facial muscles, which is accompanied by an increase in the load on the joint;
- pinching of the facial nerve causes excessive muscle tension, which, in turn, disrupts the functioning of the joint and mandible as a whole;
- involuntary contraction of the chewing muscles, which is usually accompanied by damage to the dentition, periodontal disease and inflammation of the TMJ;
- damage to the temporomandibular joint due to the progression of osteoarthritis or rheumatoid arthritis;
- inadequate prosthetics;
- congenital anomalies of the structure of the lower jaw;
- malocclusion, which in 95% is caused by destructive manifestations;
- pathologically low alveolar processes;
- inflammatory processes of the articular surface of infectious etiology;
- incorrect position of the disc at the junction of the head of the joint and the corresponding notch;
- prolonged tension of the facial muscles, clenching of teeth due to strong emotional stress.
The information provided about the probable causes of TMJ dysfunction is confirmed by clinical studies and the results of collected anamnesis about the disease.
Causes and prevention of arthrosis of the facial jaw
Based on the reasons for their occurrence, it is customary to distinguish between primary and secondary arthrosis of the jaw. The first are typical for older people (50-60 years and older) and are not associated with pathologies of the joints or dentofacial apparatus. The latter occur against the background of other disorders - for example, injury, infection, metabolic disease.
Let us consider the causes of arthrosis of the jaw joint in more detail:
- infectious disease (acute or chronic, for example, tonsillitis);
- sports or household injury (dislocation or subluxation of the jaw joint, bruise, jaw fracture);
- systematic overload (for example, when crunching nuts or intense exercise in the gym);
- dental diseases (absence of a tooth or part of it, “gentle” chewing on one side due to a dental problem);
- bruxism (unconscious grinding of teeth, usually during sleep), stress, high mental stress, mental disorders and nervous tics;
- diseases of the cardiovascular system;
- endocrine and metabolic diseases (gout, diabetes, hormonal imbalance);
- congenital anomalies of the dentofacial apparatus (including malocclusion), in which the load is distributed incorrectly;
- genetic diseases of muscle and cartilage tissue (scapulohumeral-facial muscular dystrophy, collagenopathies, as well as systemic lupus erythematosus and other autoimmune diseases);
- age-related changes (both senile and hormonal - for example, with menopause).
Often, arthrosis of the facial jaw (or temporomandibular joint - TMJ) begins due to a violation of occlusion - i.e., contact of teeth and functions of the masticatory muscles (with loss of a tooth, tumor or inflammation of the muscle muscles, lesions of the facial and trigeminal nerves). Therefore, in order to prevent arthrosis of the jaw joint, it is important to promptly replace chewing teeth with prosthetics, eliminate inflammation of the gums and dental pulp, and also treat under-erupted wisdom teeth. Do not ignore innervation disorders and muscle injuries due to stroke, surgery or incorrectly selected dentures.
Regardless of the causes, arthrosis of the jaw joint remains a chronic disease that requires lifelong monitoring and inevitably progresses.
Characteristic symptoms
Symptoms characteristic of the manifestation of a destructive process in the joint, which ensures the mobility of the lower jaw, can be pronounced or blurred, which is typical for a protracted chronic process. Periods of remission followed by exacerbations are also likely, that is, symptoms can suddenly appear against the background of imaginary well-being.
Specialists in the treatment of TMJ destruction identify the following characteristic symptoms of this pathology:
- severe soreness of the muscles of the face, neck, shoulder girdle and parotid region with irradiation into the ear cavity;
- toothache;
- pain tends to intensify during speech, eating or yawning, that is, when the amplitude of movement of the lower jaw increases;
- there is pronounced stiffness and limitation in the movement of the jaws;
- partial ankylosis (immobility) may occur as a result of jamming or blocking of the joint;
- there is a pronounced sound when opening the mouth, for example, clattering, clicking or creaking, which, in most cases, is accompanied by sharp pain;
- tension and fatigue of the facial muscles;
- sometimes swelling of the affected joint increases;
- difficulty chewing, accompanied by a feeling that the jaws are not touching each other.
The patient's general condition also shows deterioration, characterized by headache, dizziness, noise and aching pain in the ears, and decreased performance. Acute pathological processes in the temporomandibular joint sharply reduce a person’s quality of life with debilitating manifestations, disrupting many vital functions.
Who treats TMJ dysfunction?
Degenerative processes in the lower jaw joint are a disease that is treated by dentists and specialists in treating problems of the maxillofacial apparatus, for example, orthodontists and orthopedists. However, the etiological factor may necessitate intervention in the treatment process by specialists from other areas of clinical medicine. Thus, to ensure maximum effectiveness of therapeutic measures, the direct participation of such doctors may be necessary:
- a traumatologist is needed when the temporomandibular joint is displaced due to injury;
- consultations with a neurologist will be needed, first of all, if the facial nerve is pinched, as well as when exposed to many other factors, since the disease often involves nerve endings in nearby tissues and organs;
- a psychologist will be needed to stabilize the patient’s psycho-emotional state if destruction in the lower jaw joint has occurred due to prolonged tension in the facial muscles caused by psychological trauma or stress.
Of course, dental specialists play a leading role in the treatment of temporomandibular joint dysfunction, and representatives of related areas act as consultants.
If you have pathological symptoms, you should immediately contact any specialist, for example, even a therapist. The doctor will definitely conduct an examination and coordinate the patient’s further actions if he detects signs of dental pathology. The variety of manifestations of the disease of the maxillofacial apparatus, in most cases, causes difficulties in diagnosis even for an experienced specialist. An accurate diagnosis is established after additional examinations.
Which doctor should I contact?
The first signs of the disease are often discovered by a dentist when visiting a patient for dental treatment or complaining of pain in the jaw. When palpating the jaw muscle, its compaction is noted, and the mobility of the joint is limited. To clarify the clinical picture, the doctor may prescribe conventional or contrast radiography, as well as a computed tomography examination. Depending on the results, treatment may require the participation of several specialists.
Treatment of arthrosis that has developed against the background of anatomical pathologies of the joint (bad bite, abrasion of teeth, absence of several adjacent lateral teeth) is carried out by dental doctors. A dental therapist, an orthodontist and a prosthetist can take part in the treatment.
If there is a history of diseases that provoke the development of arthrosis of the TMJ, the dentist may refer the patient to specialists of a different profile:
- If the cause is a disease associated with metabolic disorders, an endocrinologist is involved in the treatment.
- If nerve conduction disorders are detected, the help of a neurologist will be required.
- An infectious lesion of the maxillofacial joint or the presence of an inflammatory process localized in other joints (arthritis, rheumatism) is a reason to consult a rheumatologist.
- In some cases, with arthrosis of the TMJ, partial hearing loss is observed, then an otolaryngologist joins the complex treatment.
Differentiation of diagnosis
The symptoms of pathological processes in the joint, which provides movement of the lower jaw, are similar to the manifestations of other diseases. Doctors, using special examinations, must accurately differentiate the diagnosis so as not to miss the development of the following serious pathologies:
- myocardial infarction, which is also characterized by pain radiating to the neck, lower jaw and shoulders;
- otitis media of unknown etiology can be suspected when there is severe pain and hearing loss;
- cerebrovascular accident may occur with dizziness, flashing of flies and nausea;
- cervical and thoracic osteochondrosis are similar in localization of pain;
- pinching of the facial nerve is also caused by unilateral tension of the facial muscles and swelling;
- complicated diseases of the gums and teeth, which are accompanied by inflammation and immobility of the lower jaw.
To avoid making an incorrect diagnosis, the doctor carefully studies the patient’s life history and illness, conducts a visual and palpation examination, and also prescribes the necessary tests.
[slide-anything id=”3470"]
Features of diagnostic measures for TMJ dysfunction
For the most accurate diagnosis of damage to the articular surface of the lower jaw at the junction with the temporal bone of the skull, specialists use the following methods and the following examination plan:
- clarification of the patient’s vital functions (work specifics, presence of chronic diseases, psycho-emotional background);
- questioning the patient about the probable cause of pathological changes in the jaw (trauma, inflammatory processes in the oral cavity, past dental history, the presence of neurological pathologies);
- visual inspection of the outer surface of the projection of the joint and the oral cavity, if possible;
- palpation examination of the joints of the mandible, which helps to identify muscle tension, swelling and displacement;
- listening to sounds when opening the mouth, which can be in the form of clicks or crackling sounds;
- determination of the amplitude of jaw mobility;
- identifying the scope of possible movements;
- assessment of the functionality of the masticatory muscles;
- determining the correct bite;
- X-ray examination of the dentofacial apparatus, which will be the most informative for excluding other pathologies of teeth and gums;
- the magnetic resonance imaging method allows you to examine the soft structures of the jaw, for example, intra-articular cartilage and its physiological position, the correctness of which determines the condition of the TMJ;
- CT scan results will provide a layer-by-layer image of the bone structure of the jaws.
The results of these examinations may require consultation and treatment with a dental surgeon, traumatologist or orthodontist.
Splint therapy with an occlusal splint for the treatment of TMJ dysfunction
This type of dental treatment is a preparation for further correction of the bite with a brace system.
At this stage, a splint splint or a so-called occlusal splint is placed in the patient’s oral cavity, which is fitted by a specialist. It is made individually for each person. The plastic splint is designed to reprogram the muscles, after which the resulting position of the jaws is stabilized by a brace system.
Features of splint treatment:
- along with the gradual correction of the position of the jaws, the splint splint gradually wears off;
- recommended for constant wear (both day and night);
- It’s comfortable to talk to her, you just need to get used to her;
- as the splint corrects the position of the joint itself and the work of the masticatory muscles, the person does not experience pain or discomfort;
- caring for the splint during treatment is extremely simple - it is removed only when brushing your teeth, washed with warm water and toothpaste or soap;
- Putting on the splint is very simple and quick.
In some cases, wearing a so-called TMJ mouth guard is prescribed.
Quite often, TMJ dysfunction is treated through systematic orthodontic expansion of the upper jaw. As a result of this treatment, the width of the upper row of teeth is normalized, not only articular pathology goes away, but also the face becomes symmetrical and more harmonious.
The result of treatment with a splint or other orthodontic systems should be an ideal position (occlusion) of the jaws with correct fissure contacts. After wearing splints, prosthetics or artistic restoration are usually recommended as the final aesthetic stage of treatment.
Therapeutic measures for diseases of the temporomandibular joint
When an accurate diagnosis of TMJ dysfunction is established, the doctor prescribes a course of therapeutic measures, the features of which are determined by the degree of the pathological process and the etiological factor. The disease requires complex treatment. The most lasting effect in restoring the functions of the maxillofacial apparatus is provided by the following recommendations, methods and means:
- complete exclusion of solid food, which will make it possible to maintain conditional rest for the mandible joint;
- maximum restriction of mobility (no yawning, no talking);
- alternating warm and cold compresses in combination with certain exercises to warm up the joints, which is performed under the supervision of a physiotherapist;
- for pain relief, the doctor prescribes non-steroidal anti-inflammatory drugs in a certain dose and at the recommended dosage interval;
- in case of extremely severe pain, it is possible to take narcotic analgesics;
- muscle relaxants are used to eliminate tension in the muscles of the face, neck and shoulder girdle, if any;
- to restore harmony in the patient’s psycho-emotional background, it is possible to take antidepressants in small dosages;
- physiotherapeutic procedures (laser, electrophoresis with novocaine, ultrasound, radio wave therapy, neurostimulation);
- installation of a special design on the teeth (mouthguard, orthopedic splint), which allows you to prevent the closure of the dentition as much as possible, correct the bite and restore the movement of the TMJ joint in the physiologically correct position;
- orthopedic treatment involves the installation of crowns and bridges to align the dentition and ensure comfortable static and dynamic occlusion;
- avoidance of foods that irritate tooth enamel to prevent relapse of exacerbation;
- a slightly open position of the mouth, which is carried out using the tongue located between the front teeth, will ensure relaxation of the masticatory muscles and jaws;
- in some cases, doctors use the injection of analgesic drugs into the muscle tissue of the projection of the pathological joint.
Complex treatment using the listed methods and means, in most cases, gives a positive effect and long-term remission.
How can you tell if a person is suffering from TMJ dysfunction?
The listed symptoms are a clear sign that something is wrong with the joint and require mandatory comprehensive treatment. Even in the early stages of the development of the disease, a person does not feel any deviation from the norm, his jaw begins to behave differently, and the pain in the mouth intensifies over time.
To confirm the diagnosis, the dentist must:
- carry out a visual examination of the teeth and oral cavity as a whole;
- collect anamnesis and study the patient’s complaints;
- perform an ocludogram to study the position of the jaws in relation to each other;
- refer the person for orthopantomography, x-ray and computed tomography of the TMJ. An MRI may be needed to monitor and correct treatment.
In some cases, additional consultation with related specialists is required: neurologist, rheumatologist, ENT specialist, etc.
Based on the diagnostic procedures performed, the patient is diagnosed and step-by-step treatment is prescribed.
It is important! To effectively treat the disease, you need to contact an experienced dentist, who will not only diagnose the condition of the oral cavity, but will be able to distinguish a violation of the structure and functions of the TMJ from other pathologies. For example, from jaw dislocation, articular arthrosis, complex diseases, arthritis, synovitis, etc.