Limited mouth opening, inability to chew food, missing teeth
Before
Stages
After
Specialists:
Nazaryan David Nazaretovich
Description:
The patient came to the clinic with complaints of pain in the TMJ area, more pronounced on the left side, limited mouth opening, inability to chew food, missing teeth in the lower jaw, and destruction of some teeth. During the diagnosis, an input MRI of the TMJ revealed displacement of the articular discs of the temporomandibular joint without the possibility of reduction. Due to the absence of chewing teeth on the lower jaw on the left side, a decrease in the height of the crowns of the chewing teeth on the right side, and TMJ disease, the head of the joint fell deeper into the articular fossa. Due to the displaced articular disc, the head of the lower jaw began to contact areas not intended for load (hence the pain syndrome) and change its shape in response to contact with the bone tissue of the temporal bone fossa. The displaced disc blocked the opening of the mouth and the ability to move the jaw forward and to the sides.
The first stage of treatment was the production of a therapeutic and diagnostic distraction mouthguard - Splint, which made it possible to move the head of the lower jaw away from the articular fossa. The second stage involved surgical correction of the position of the displaced discs. You can notice changes in the height of the bite in the lateral sections with the correct position of the discs on the heads of the joint. The third stage involved orthodontic correction to ensure support for the TMJ structures using the patient’s own teeth. At this stage, implantation of missing teeth and temporary prosthetics were performed. While wearing the braces system, we were able to regain the lost bite height. After removing the brace system, local prosthetics will need to be performed for long-term stability of the result.
general information
Everything in the human body is interconnected. Changes in one organ area will cause a cascade of reactions throughout the body, including the musculoskeletal one.
Most medical practitioners do not look at the TMJ joint, but rather pay attention to the pain that occurs in different areas of the body due to TMJ dysfunction. Ascending postural causes of temporomandibular joint dysfunction are often associated with pelvic instability or instability of the sacroiliac joint. system - posture. Thus, postural instability of the body spreads upward, causing changes in the functioning of the temporomandibular joint. In addition, interactions at the dental level also affect the functioning of the TMJ.
When treating a patient's body for TMJ dysfunction and malocclusion, it is important to look at the entire system.
The pelvis is important for a balanced, stable position of the spine.
Inside the spinal column there is the dura mater, which also lines the cranial cavity from the inside, and is a single, inextensible, high-density structure. It is extremely important for the formation of the relationship between the skull and the spine. The dura mater has features in the places of attachment to bone structures, but we are especially interested in the sacrum and occipital bone, in the area of which the main fusion occurs. Thus, it is possible to trace the close relationship of the occipital bone and the sacrum, which normally should have synchronous movement. A dura mater stretched unnaturally as a result of scoliosis or pelvic pathology will directly lead to disruption of the functioning of both the occipital bone and the sacrum. Dysfunction in the pelvis quickly moves upward, causing pain in the neck, thoracic region, lower back, and finally affecting the function of the TMJ.
There is also an ascending type of dysfunction, in which problems in the lower levels of the body cause dysfunction in the upper parts. Now imagine that there is a leg injury or a spasm in the sacroiliac joint on one side. What will the body do? It will shift the main load to the healthy side (leg, or the side without pain and spasms).
The spine and the entire postural system of the body will adapt to the new center of gravity through body distortion. The distortion of the body will occur with the help of muscles that will contract or relax in a “chessboard” pattern, under the command of the central nervous system. Her commands will be aimed at maintaining body balance, because otherwise the person will simply fall on his side. This mechanism will also be reflected on the head, which will tilt in the opposite direction in order to maintain balance. Now let's look at the skull.
Intracranial pressure will automatically increase on the low side of the tilt and with a prolonged position of the head, the skull will tend to equalize this pressure. The central nervous system will once again give a command to the muscles of the anterolateral surface of the neck, the masticatory group. They will contract in such a way that the middle and anterior zones of the skull turn in the opposite direction, thereby balancing the intracranial pressure. Also, with the help of muscles, other mechanisms are implemented that maintain balance and postural balance of the body.
There are 3 powerful zones responsible for body balance:
1 - Eyes
2 - Vestibular apparatus
3 - Feet
If any of these systems fails, the load will be distributed among the others. Now imagine that when you tilt your head, caused by spasmed muscles of the back group (to maintain balance), information from the horizontal planes of the vestibular apparatus and eyes will become incorrect. In an attempt to align the signals, the brain will also give a command, and the neck muscles will contract, trying to rotate the middle and anterior zones of the skull closer to the horizon, i.e. align your eyes.
Complaints of headaches, pain in the TMJ area, clicking when moving the lower jaw
Before
After
Specialists:
Nazaryan David Nazaretovich
Description:
The patient came to the clinic with complaints of headaches, pain in the TMJ area, clicking when moving the lower jaw, and lack of stable position of the lower jaw.
From the anamnesis: about 6 years ago, prosthetics were performed in the lateral sections of the upper and lower jaw in another medical facility. Tooth 4.6 was removed for therapeutic reasons (exacerbation of chronic periodontitis).
At the time of examination, the patient had no lateral bite support on the right side and the 8th teeth on the lower jaw stood above the occlusal plane and created traumatic nodes during chewing. This could provoke a forced displacement of the lower jaw.
According to the conclusion of MRI of the TMJ, displacement of the articular discs with reposition was noted. (with restoration of position when opening the mouth)
At the rehabilitation stage, teeth 3.8, 4.8 were removed, the bridge structure on the upper jaw was removed and single composite crowns were made, implantation was performed in the area of the missing tooth 4.6, and a therapeutic and diagnostic mouth guard (Splint) was performed with preliminary diagnosis of the dental system and electrical myostimulation of the masticatory muscle group for fixation true position of the lower jaw.
During the active wearing of Splint and its corrections, the patient’s complaints resolved and subsequently required orthodontic treatment to ensure correct bite and support of the TMJ.
Structure of the temporomandibular joint
Author: Bravetti P
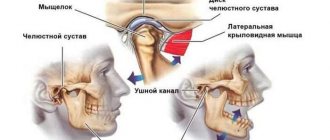
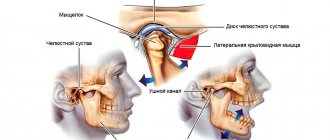
The temporomandibular joint (TMJ) is a synovial joint and is the only true joint in the maxillofacial region. It is also known as the mandibular joint or the craniomandibular joint. The temporomandibular joint is unique due to its rotational (ginglymoid joint) and translational (arthroid joint) movements during mandibular function, including opening and closing the mouth, chewing, and speaking. The right and left joints cannot move independently of each other as they are connected through the mandible to form the bicondylar articulation (Alomar et al. 2007). Moreover, the teeth serve as a guide and limit certain movements of the lower jaw. As the name suggests, the formation of the temporomandibular joint involves two bones, that is, the temporal bone and the mandible (Figure 1, 2, 3, and 4).
Figure 1 Temporomandibular joint in the skull (white dotted circle), right lateral view. SM condyle of the mandible, CP coronoid process. 1 Squamosal part of the temporal bone 2 mastoid process of the temporal bone 3 tympanic part of the temporal bone with the external auditory canal 4 zygomatic process of the temporal bone
Figure 2 Right lateral view of a cross-section of a cadaver's head, showing the temporomandibular joint region (black dotted circle). SM condyle of the mandible, CP coronoid process, TBz zygomatic process of the temporal bone
Figure 3 3D rendering of cone beam computed tomography images of the left temporomandibular joint in a 62-year-old man. AT Articular tubercle, SM mandibular condyle, CP coronoid process, EAC external auditory canal, MR mastoid process, StP styloid process, TBz zygomatic process of the temporal bone
Figure 4 Sagittal section of cone beam computed tomography of the temporomandibular joint in a 22-year-old woman. AT Articular tubercle, SM condyle of the mandible, CP coronoid process, EAC external auditory canal, MF foramen of the mandible
The glenoid fossa of the temporomandibular joint is formed by the mandibular fossa, a mediolaterally elongated cavity located in the inferior part of the temporal bone just anterior to the external auditory meatus (Figures 5 and 6). The articular fossa is limited in front by a bony protrusion - the articular tubercle. The head of the temporomandibular joint is the upper part of the condylar process, which is the posterior part of the ramus of the mandible and is located opposite its anterior part - the coronoid process.
Constant clicking in the TMJ area when chewing
Before
Frontal photograph of the bite. There is an inclination of the occlusal plane of the upper jaw to the right side
Lateral photograph of the bite (right). Incorrect inclination of the maxillary incisors is noted. (Lower jaw lock). Stamped crown on tooth 4.6
Lateral photograph of the bite (left). Missing tooth 2.6
Photograph of the teeth of the upper jaw. Crowded position of the anterior group of teeth. Rotations of the molar and premolar groups. Erupted teeth 1.8, 2.8 (as one of the causes of traumatic nodes in occlusion). Asymmetrical dentition
Photograph of the teeth of the lower jaw. Secondary caries under old restorations on the molar group of teeth. lack of correct anatomy of the stamped crown of tooth 4.6. erupted teeth 3.8, 4.8
MRI slice of the left TMJ in the mouth opening position of 54 mm. The head of the joint extends beyond the articular tubercle, but to a lesser extent on the right side. (joint hypermobility)
MRI slice of the left TMJ in the open mouth position 43mm. Reposition of the disc is noted (the disc is in the correct position)
MRI slice of the Left TMJ in the closed mouth position. Anterior displacement of the articular disc is noted
MRI slice of the right TMJ in the open mouth position 54 mm. The head of the joint extends beyond the articular tubercle (hypermobility of the joint)
MRI slice of the right TMJ in the open mouth position at 43mm. The normal position of the articular disc is noted
MRI slice of the right TMJ in the closed mouth position. The normal position of the articular disc is noted
Stages
Frontal photograph of the bite. Beginning of correction of the inclination of the occlusal plane of the upper jaw
Lateral photograph of the bite (right). There is a rise in the bite due to orthodontic onlays
Lateral photograph of the bite (left). There is a rise in the bite due to orthodontic onlays
Photograph of the teeth of the upper jaw
Photograph of lower jaw teeth
After
Frontal photograph of the bite. There is no inclination of the occlusal planes of the upper and lower jaw
Lateral bite photograph (right)
Lateral photograph of the bite (left). The contact density in the molar area will be restored by replacing the temporary crown on the 2.6 implant
Photograph of the teeth of the upper jaw
Photograph of the teeth of the lower jaw. The temporary crown of tooth 4.6 needs to be replaced
Specialists:
Nazaryan David Nazaretovich
Description:
The patient complained of constant ringing clicks in the TMJ area when chewing, opening the mouth and moving the lower jaw. Entry MRI revealed joint hypermobility and disc dislocation with recovery.
After wearing Splint, positive dynamics, and analysis of the results of the control MRI, no indications for joint surgery were identified. The task was to rebuild the patient's bite to support the joint. Treatment with braces lasted 17 months. At this stage, implantation was carried out in the area of 2.6 teeth, removal of all 8 teeth, temporary prosthetics on an implant, as well as restoration of the erased cutting edges of the central incisors. After removing the braces, local orthopedic work will be performed to stabilize the bite.
Anatomy of the TMJ
Home / Articles / Anatomy of the TMJ
The functioning of the TMJ (temporomandibular joint) determines the condition and health of the dental system, as well as the body as a whole. Due to its proper operation, the normal implementation of processes such as chewing, speaking, and movement of the lower jaw is ensured. Every day the TMJ performs thousands of movements, but the work of the joint is invisible, since it is hidden in the cheek and temple area. The balance of the TMJ normally allows a person to freely move the lower jaw, open and close the mouth, the imbalance does not appear immediately, but is also noticeable by the characteristic features that the orthodontist Farida Yusifovna Gasimova tells us about.
— Farida Yusifovna, how does the temporomandibular joint work?
— The structure of the joint is very complex, unlike other components of the internal structure of the body, its work does not in any way affect the functioning of the blood vessels, ear, nerves, although the joint is located directly next to it. This, one might say, is a perfect device that clearly and fully fulfills its role in the functioning of the body. Thanks to the paired design, uniform movement of both sides of the jaw is ensured simultaneously and equally. The anatomical structure of the TMJ includes the heads, fossae, capsules, ligaments of the articular tubercle, stylomandibular ligament and retroarticular disc. The active movement of the lower jaw relative to the upper is ensured by the structure of the head of the lower jaw, which has the shape of an ellipse, so the lower jaw easily moves forward and backward, right and left, up and down. The movable support is provided by the condylar processes at the end of which the head of the lower jaw is located. In children and adults, there are slight differences in the composition of the bone of the head, since with age new movements and functions are acquired, and the bone is overgrown with cartilage. Also, the size and shape of the head of the lower jaw is individual for each person since it is formed depending on the development and various factors of a person’s life; with age, changes occur in its structure. Next to the temporal bone and the zygomatic process and tubercle there is a mandibular fossa, which is separated from the auditory canal by a bone plate, and from the tympanic cavity by the posterior fornix. This structure allows you to avoid the development of pathological processes. The fossa is fenced off by the tympanic fissure, the zygomatic process, the sphenoid bone and the tubercle. The mandibular fossa is divided into extracapsular and intracapsular, and changes shape over the course of a person’s life. The articular tubercle becomes smaller in old age, this is associated with jaw deformation and loss of teeth; in newborn children it is absent altogether and is completely formed by the age of 7-8 years. Depending on the condition of the dentofacial system and teeth, the articular tubercle develops individually. The articular disc dentistry Millennium Anapa Mayakovsky is nourished through the fluid of the periarticular tissues and lymph; nerve endings do not approach it. The articular disc is located in the area of the tubercle and head. Depending on the type of jaw, the individual thickness and shape of the articular disc is formed. Movement of the disc and head is provided by ligaments woven into a dense capsule consisting of endothelial and fibrous connective tissue. Thanks to the work of the ligaments, the lower jaw moves up, down, sideways, forward and backward. Also, the ligaments restrain the stretching inside the TMJ and fix the joint.
— Farida Yusifovna, what specific function does the temporomandibular joint perform?
— The temporomandibular joint has many functions, the main one of which is to ensure the process of chewing, speech, pronunciation of sounds and movement of the lower jaw. Also, the temporomandibular joint is a unique human organ, consisting of two connected parts - right and left, which move equally and in parallel, have the same structure and structure. Together they are combined into a single complex system, with synchronous balanced movement. When synchrony is disrupted, TMJ dysfunction is diagnosed. The temporomandibular joint transmits impulses to the central nervous system, thereby ensuring chewing processes. The trigeminal nerve functionally connects the dentition on the lower and upper jaws and muscles; together this represents a complex biological system. The reflex activity of the TMJ ensures synchrony and parallelism of movements and the touching of teeth. If an imbalance occurs, it is necessary to carry out timely treatment, otherwise the person’s bite will be deformed and the teeth will be worn out.
— What does the term TMJ dysfunction mean?
— Disorders of the temporomandibular joint appear due to problems in the movement of the temporomandibular joint, which occurs simultaneously on both sides of the head. A violation is called uneven movement on the left and right sides when there is asymmetry. TMJ diseases can be very different, the most common are arthritis and arthrosis, ankylosis, synovitis, tendonitis, joint dislocation. Disturbances in the functioning of the TMJ cause pain and discomfort in the facial area; the causes may be mechanical injuries, malocclusion, damage to the jaw, poor-quality surgical intervention or dental treatment, infection, stress, genetic predisposition, anatomical abnormalities of the structure, excessive loads, pathologies of tooth abrasion. Dysfunction manifests itself initially weakly, many patients do not notice the symptoms until their brightness acquires colors in the form of closing of the jaw, crunching and clicking when moving the jaw, pain and itching, displacement of the jaw when opening the mouth, pain radiating to the ear, temple, swelling of the face, dizziness, tinnitus and other characteristic signs of TMJ dysfunction. The appearance of such symptoms should be a reason to contact Millennium Anapa Mayakovsky Dentistry.
Comprehensive hygiene for 2500 rubles! Air Flow 1000p for patients with braces!
A unique promotion for our regular patients! A set of hygienic procedures (removal of tartar and plaque using Air Flow and ultrasound , scaling, polishing, fluoridation) for regular patients once every 6 months for RUB 3,000!
Air Flow and polishing for only RUR 1,500 for patients with braces!
Dissatisfaction with facial aesthetics, limitations in mouth opening
Before
Frontal photograph of the bite. Cross occlusion is noted on the right side. Absence of contacts of the premolar group on the left side. Tilt of the occlusal plane of the lower jaw to the left
Lateral photograph of the bite (right). Incorrect inclination of the frontal group of teeth in the upper jaw is noted. The lower jaw occupies a posterior (retracted) position
Lateral photograph of the bite (left). The incorrect inclination of the anterior group of teeth in the lower jaw is clearly expressed. Lack of closure of teeth in the lateral region
MRI slice of the right TMJ in the closed mouth position. The normal position of the articular disc is noted. Articular head of regular shape
MRI slice of the Left TMJ in the closed mouth position. There is a pronounced structural deformation of the articular head
MRI slice of the right TMJ in the open mouth position at 34mm. The normal position of the articular disc is noted
MRI slice of the left TMJ in the open mouth position 34mm. There is a limitation in the movement of this deformed joint. The articular disc is not in the correct position
After
Frontal photograph of the bite. Patient with a splint in the postoperative period
Lateral photograph of the bite (right). Ensures uniform contacts in the lateral sections
Lateral photograph of the bite (left). Ensures uniform contacts in the lateral sections
Specialists:
Nazaryan David Nazaretovich
Description:
The main complaints of the patient in this clinical case were dissatisfaction with facial aesthetics (the lower jaw is shifted to the right side) and limitations in mouth opening with pain in the area of the left TMJ. The entry MRI of the TMJ shows a pronounced deformation of the head of the left condyle with unreducible displacement of the articular disc.
The patient was recommended to undergo surgical treatment of the TMJ with preliminary production of Splint in preparation for the operation and subsequent use of this mouth guard in the postoperative period to support the joint structures during the healing period. The second stage of treatment for this patient will be orthodontic treatment in preparation for orthognathic surgery aimed at changing the position of the jaw bones and eliminating asymmetry.
The temporomandibular joint (TMJ) (articulatio temporomandibularis) , formed by the head of the mandible and the mandibular fossa of the temporal bone (Fig. 1-24).
Rice. 1-24. Temporomandibular joint (TMJ) . A: 1 - zygomatic arch; 2 - zygomatic bone; 3 - coronoid process of the lower jaw; 4 - maxillary bone; 5 - second molar; 6 - lower jaw; 7 - third molar; 8 - masticatory tuberosity; 9 - branch of the lower jaw; 10 - stylomandibular ligament; 11 - condylar process of the lower jaw; 12 - anterior (outer) part of the lateral ligament of the temporomandibular joint; 13 - posterior (internal) part of the lateral ligament of the temporomandibular joint; 14 - mastoid process of the temporal bone; 15 - external auditory canal.
B: 1 - sphenoid sinus; 2 - lateral plate of the pterygoid process of the sphenoid bone; 3 - pterygospinous ligament; 4 - spine of the sphenoid bone; 5 - neck of the lower jaw; 6 - sphenomandibular ligament; 7 - styloid process of the temporal bone; 8 - condylar process of the lower jaw; 9 - stylomandibular ligament; 10 - opening of the lower jaw; 11 - wing-shaped hook; 12 - pterygoid tuberosity; 13 - angle of the lower jaw; 14 - mylohyoid line; 15 - molars; 16 - premolars; 17 — fangs; 18 - hard palate; 19 - medial plate of the pterygoid process; 20 - inferior nasal concha; 21 - sphenopalatine foramen; 22 - middle turbinate; 23 - superior nasal concha; 24 - frontal sinus
The head of the lower jaw is a roller-shaped thickening of an ellipsoidal shape, elongated in the transverse direction. The axes, extended along the length of the head, converge at the anterior edge of the foramen magnum, forming an obtuse angle. In front of the head, in the pterygoid fossa, the lateral pterygoid muscle is attached. The posterior surface of the head is slightly convex, triangular in shape, with the base facing upward. The articular surface of the mandibular fossa is 2-3 times larger than the head of the mandible. It has an elliptical shape. The fossa is divided into two parts: anterior - intracapsular and posterior - extracapsular. The incongruity between the head and fossa is leveled by the articular disc and the attachment of the joint capsule on the temporal bone. The intracapsular part of the articular fossa is limited in front by the slope of the articular tubercle, and in the back by the petrotympanic fissure. From the outside, the fossa is limited by the root of the zygomatic process, from the inside by the angular spine of the sphenoid bone. The shape of the mandibular fossa is different and depends on individual development factors, as well as the nature of dental occlusion. There are two extreme forms - deep and flat.
One of the characteristic features of TMJ is the presence of an articular tubercle, which is unique to humans. The articular tubercle, limiting the fossa in front, is a bony prominence of the zygomatic process. There are two extreme forms of the tubercle: a low and wide tubercle corresponds to a flat mandibular fossa, a high and narrow one corresponds to a deep fossa (Fig. 1-25).
Rice. 1-25. Shape of the articular tubercle : a - flat; b - medium-convex; v - cool
The articular disc (discus articularis) consists of fibrous cartilage tissue. It divides the joint cavity into two isolated slits - upper and lower. The disc has the shape of a biconcave lens, in which anterior and posterior sections are distinguished. Between the latter there is a thinner and narrower middle part of the disk. The anterior part of the disc is thicker than the posterior part. Its thickness depends on the shape of the articular fossa: the deeper and narrower the fossa, the thicker the disc, and, conversely, the flatter and wider the fossa, the thinner the disc (Fig. 1-26).
Rice. 1-26. Differences in the structure of the articular surfaces of the TMJ : a - ovoid shape of the condylar process and deep mandibular fossa; b — flat shape of the condylar process and the mandibular fossa: 1 — mandibular fossa, 2 — articular disc, 3 — condylar process; 4 — mandibular fossa (bottom view), 5 — isolated condylar process
Therefore, two extreme forms of the articular disc are distinguished: with one of them, the articular disc is flat and thin, with the other, narrow and thick. The purpose of the disc is to equalize the discrepancy between the articular fossa and the head and, due to its elasticity, to soften chewing impacts. The superior joint space is located between the glenoid fossa and the articular tubercle and the superior surface of the articular disc. The lower articular space is limited at the top by the concave surface of the disc, and at the bottom by the articular head of the mandible. The articulated surfaces in the lower joint gap fit one another more tightly, so it is narrower here than the upper one. The tendon fibers of the lateral pterygoid muscle are woven into the anteromedial edge of the articular disc, thanks to which it can move down the slope of the articular tubercle down and forward.
The articular capsule of the TMJ is extensive and flexible, allowing significant movements of the lower jaw. At the top, the capsule is attached anteriorly along the edge of the zygomatic arch, posteriorly along the fissura petrotympanica, medially along the spina angularis and sutura petrotympanica, then it turns outward and captures the articular tubercle in front. On the lower jaw, the capsule runs along the neck of the articular process, leaving the fovea pterygoidea outside the capsule. At the back, the capsule is thickened, and the extracapsular part of the mandibular fossa is filled with loose connective tissue, forming a maxillary cushion. The TMJ ligaments are divided into intracapsular and extracapsular . The intracapsular ligaments include the anterior and posterior discotemporal ligaments, running from the upper edge of the disc upward and forward and backward towards the root of the zygomatic arch; lateral and medial disconomandibular, located from the lower edge of the disc down to the attachment of the capsule at the neck of the lower jaw. Three ligaments are extracapsular. 1. The lateral ligament (ligamentum laterale) starts from the base of the zygomatic process and the zygomatic arch, goes down to the neck of the articular process. The ligament has the shape of a triangle, with the base facing the zygomatic arch, and consists of two parts: the posterior one, in which the fiber bundles go from above and forward, and the anterior one - the fiber bundles go from top to bottom and back. This ligament inhibits the lateral inward movements of the lower jaw. 2. The sphenomandibular ligament (ligamentum sphenomandibulare) originates from the angular spine of the sphenoid bone, extends downward, attaching to the lingula of the lower jaw. The ligament delays the lateral and vertical movements of the lower jaw.
3. The stylomandibular ligament (ligamentum stylomandibular) runs from the styloid process of the temporal bone down to the posterior edge of the ramus of the mandible. This ligament inhibits the forward movement of the lower jaw. The TMJ is a combined joint. Its articular surfaces are covered with fibrous cartilage. According to the nature of the movements, the joint is classified as block-shaped. The lowering and raising of the lower jaw is possible in the joint. With a slight lowering of the lower jaw, movement occurs around the frontal axis in the lower joint gap, while the head of the lower jaw produces rotational movements along the lower surface of the disc. The forward movement of the lower jaw occurs in the upper gap of the joint. In this case, the head together with the disc is one piece and slides forward and down the slope of the articular tubercle. Simultaneously with this movement, the head of the jaw makes rotational movements in the lower gap of the joint. Lateral movements of the lower jaw occur due to unilateral contraction of the lateral pterygoid muscle and the anterior bundles of the temporal muscle of the opposite side. The angle of deviation towards the lower jaw is 15-17°. The head of the jaw on the side of the contracting muscles makes its way down and forward onto the articular tubercle along with the disc, while turning inward. The movement occurs in the upper gap between the upper surface of the articular disc and the slope of the articular tubercle. In the joint of the opposite side, where the lower jaw has advanced, the head remains in the articular fossa, performing rotational movements around the vertical axis. In addition, the head shifts backward and inward. Movement occurs in the lower chamber of the joint between the lower surface of the disc and the articular head (Fig. 1-27).
Rice. 1-27. Sagittal section of the temporomandibular joint (TMJ)
In the joint cavity there is a biconcave Z-shaped curved cartilage disc. Since the lower jaw anatomically has two joints, it is classified as combined, complex, or biaxial. The movements in it are complex. The structure of the joint allows the lower jaw to perform rotational movements around the frontal axis - lower the jaw (open the mouth) to a distance of up to 5 cm between the front teeth in an adult. Further lowering leads to dislocation. If the mouth opens excessively, the condyle of the lower jaw can slip forward through the tubercle and be fixed in this position by muscle contraction. All this causes dislocation of the lower jaw, which can be on one or both sides. In this position, movements of the lower jaw are impossible, there is no speech, only inarticulate sounds are made. The dislocation must be reduced, and as quickly as possible, otherwise the stretched capsule creates conditions for repeated phenomena. But this must be done by a doctor, since inept reduction can be complicated by a fracture of the neck of the condylar process of the mandible. Since the joints are separated from each other, movements in them can be separate. This is facilitated by the wide capsule and ellipsoidal shape of the condyle of the jaw, i.e. presence of a vertical axis. More precisely, it is possible to move the jaw forward in one joint, but not to do this in the second joint, thus, in a non-adjustable joint, the condyle rotates around a vertical axis. The chin part of the jaw moves in a circle around the center. This displacement is limited by the joint of the opposite side and, above all, by the depth of its fossa of the temporal bone, the severity (height) of the articular tubercle and the strength of the articular ligaments. From the average position, the chin can move to the sides by no more than 15-17°, i.e. by 4.5% of the circumference. In addition to these movements, the jaw can move forward and backward simultaneously in both joints: this movement is called translational. Thus, the TMJ is the only joint that allows translational movements. Combinations of the described movements create the ability to chew, not only squeezing, but also crushing food by the shear type (move the jaw forward, sideways). The relief of the teeth also serves this purpose.
Materials used : Anatomy, physiology and biomechanics of the dentofacial system: Ed. L.L. Kolesnikova, S.D. Arutyunova, I.Yu. Lebedenko, V.P. Degtyareva. — M.: GEOTAR-Media, 2009
You might be interested in:
- Incisors (dentes incisivi). There are 8 incisors located in the middle of the dental arches, they are called the front teeth. There are upper and lower incisors, as well as medial...
">Structure of incisors
- Human teeth are an integral part of the masticatory-speech apparatus, which is a complex of interacting and interconnected organs...
">General structure of teeth
We recommend reading:
- General information about the structure of the human skull. The skeleton of the head is made up of paired and unpaired bones, which together are called the skull, cranium. ...
">Structure of the human skull
- Lower jaw The lower jaw (mandibula) is unpaired, horseshoe-shaped, the only movable bone of the skull. It consists of two symmetrical...
">Structure of the lower jaw
- Upper jaw The upper jaw, maxilla, paired, is located in the center of the face and connects with all its bones, as well as the ethmoid, frontal and…
">Structure of the upper jaw
Pain syndrome and restrictions in movements of the lower jaw
Before
Frontal photograph of the bite
Lateral photograph of the bite (right). Absence of tooth 4.5, absence of tooth 1.4 are noted with replacement of the defect with a removable partial apparatus
Lateral bite photograph (left)
MRI slice of the left TMJ. There is a structural change in the shape of the joint head. Anterior disc dislocation without reduction (without restoration)
After
Frontal photograph of occlusion after joint surgery
Lateral bite photograph (right)
Lateral photograph of the bite (left). There is a rise in the height of the bite on the operated side
MRI section of the left TMJ after surgical reduction of the articular disc. The correct position of the disc is noted
Frontal photograph of the bite in the mouthguard (Splint)
Lateral photograph of the bite in the mouth guard (Splint) (right view)
Lateral photograph of the bite in the mouthguard (Splint) (left view)
Specialists:
Nazaryan David Nazaretovich
Description:
A typical complaint for patients with TMJ problems is pain and restrictions in the movements of the lower jaw. Such complaints were also present in this clinical case. The entry MRI of the TMJ shows a pronounced structural change in the shape of the head of the left joint and an articular disc displaced forward without the ability to restore its position.
We carried out preliminary Splint therapy in preparation for joint surgery (we made a transparent rigid mouthguard for the lower dentition) and assessed the result over time with a series of control MRIs of the TMJ. Using the example of a section from one of these studies, one can clearly compare the picture before and after surgery. The patient also noted positive dynamics regarding pain symptoms already at the stage of wearing a mouth guard. In the postoperative period, pain was no longer observed. The range of movements of the lower jaw was restored. Of course, the closure of the teeth changed after placing the disc in the correct position. We will require orthodontic and orthopedic treatment to support the stability of the TMJ.