Sinusitis is an insidious disease in that the first symptoms and signs of sinusitis are very similar to a common cold and therefore often remain without proper attention. When obvious distinctive symptoms of the disease appear, time may be lost and the disease turns out to be in full swing - in an acute form.
Sinusitis is a disease that requires immediate treatment, since the disease is dangerous because inflammation occurs near the eyes and brain, and if effective treatment is not started in a timely manner, the disease can lead to very serious complications, including death. It should be noted that sinusitis is one of the most common diseases of the ENT organs.
In the article below, you will find information about what sinusitis is and its symptoms, photos and schematic images, where the source of inflammation is located, how the chronic and acute forms differ, the ICD-10 code, what this disease leads to if it do not treat.
The success of treatment largely depends on the degree of trust between the patient and the doctor, therefore, if your relationship with the doctor does not work out, you can always turn to another specialist. This article is intended to help you. With its help, you can familiarize yourself with the disease, receive additional information and more complete answers to questions if any arise after visiting your doctor. The article is for informational purposes only and is not an instruction for self-medication.
Author of the article: doctor Patrusheva E.V.
What is sinusitis?
Sinusitis is more common in adults than in children. According to the latest medical statistics, 10-15% of the population in all developed countries falls ill with sinusitis every year, and this number increases annually by 2-3%. The statistics are somewhat scary.
What kind of disease is this?
Sinusitis is an inflammation of the maxillary sinuses. Very often they are called maxillary or maxillary, since the sinuses are located in the thickness of the upper jaw. Consequently, sinusitis and maxillitis are two different names for the same disease.
Moreover, in ICD-10 (“International Classification of Diseases”) the disease is designated as maxillary sinusitis J01.0.
It is important to know that the symptoms of sinusitis in the initial stages are non-specific and similar to a common cold. Moreover, chronic and persistent nasal diseases can mask the disease, making it difficult to make a correct diagnosis. That is why, if any changes in your health status occur, you should consult a doctor.
You can learn about what sinusitis is and how to treat it by watching this video with Elena Malysheva and Doctor of Medical Sciences, Professor G.Z. Piskunov.
Sinusitis and sinusitis - what's the difference?
Very often in the diagnosis we read the name “sinusitis”, but the doctor said that it was sinusitis. How do they differ from each other, which diagnosis is correct? Or maybe it's one and the same?
If we open the document that doctors use when making any diagnosis - the International Classification of Diseases (ICD-10) - and read it, we will not find in the document a disease called “sinusitis”; its place is taken by “sinusitis”.
In fact, “sinusitis” is a general name for inflammatory diseases of all sinuses. There are 4 paired sinuses - the frontal, ethmoid, sphenoid and the familiar maxillary sinuses. The inflammation of each of these sinuses has its own name:
- Inflammation of the frontal sinuses - frontal sinusitis or frontal sinusitis.
- Inflammation of the ethmoid sinuses – ethmoiditis or ethmoidal sinusitis.
- Inflammation of the sphenoid sinuses – sphenoiditis or sphenoidal sinusitis.
- Inflammation of the maxillary sinuses – sinusitis, maxillitis or maxillary sinusitis.
That is why in ICD-10 there is only sinusitis, as a general name for all inflammatory diseases of the paranasal sinuses, and it is designated J01. That is, sinusitis and sinusitis are the same name for the same disease - inflammation of the maxillary sinus. And the correct diagnosis may sound: “sinusitis of the maxillary sinuses”, “maxillary sinusitis” or “sinusitis” - the difference is only in the words.
Since sinusitis most often occurs as a complication of a runny nose (rhinitis), it is also called rhinosinusitis.
How dangerous is sinusitis and can you die from it?
Regardless of the name, “sinusitis,” “maxillitis,” or “sinusitis,” this is a dangerous disease. In the absence of qualified and timely medical care, serious complications can occur, for example, the disease can develop into meningitis. If the disease is not treated or self-medicated, death may occur from its complications.
To better understand what sinusitis is and why it is dangerous, what it can lead to, it is necessary to consider the anatomical features of the structure and location of the human nasal sinuses.
Exceptions to the rules - pathologies
There are cases of improper development and formation of additional partitions or the absence of some cavities. Excessive pneumatization and pathologies of bone walls are diagnosed. Congenital pathologies do not manifest themselves, but cause complications.
Nasal problems occur after injury directly to the nasal sinus or after a closed intracranial one. The sign is always eye pain, and sometimes the person suffers traumatic shock or loses consciousness. Bone fragments can shift, causing bleeding, and if the ethmoidal labyrinth is affected, liquorrhea occurs. On examination, an uneven fracture line and displacement of the shadows of the lines of the sinus walls are observed.
The structure of the human nasopharynx
The structure of the nasopharynx is quite simple. We can say that this is a cavity located in the human skull that connects the oral and nasal cavities. The nasopharynx also communicates with the sphenoid, occipital bone, with the cervical vertebrae and neck, with the tympanic cavities, with the lateral auditory openings and the eustachian tubes.
If you look at the structure of the human nasopharynx in the diagram, you can see that the nasopharynx connects all the cavities in the human skull.
All nasal cavities are interconnected with each other and with the nasopharynx. This structure contributes to the rapid spread of infection during sinusitis, and if left untreated, severe complications and even death can easily occur.
The structure and location of the paranasal (maxillary) sinuses
As stated above, there are 4 paired paranasal sinuses. The diagram shows their location, it is clear where they are located (with the exception of the sphenoid sinus).
- The frontal sinuses of the nose are located above the superciliary arches and through the frontal canal they communicate with the anterior part of the middle nasal meatus.
- The ethmoid sinuses look like cells that communicate with each other and with the nasal cavity.
- The sphenoid sinuses are located in the body of the sphenoid bone.
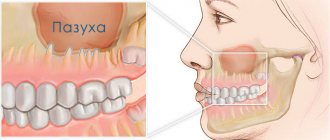
- The maxillary sinuses are paired. These nasal sinuses are located in the thickness of the upper jaw, symmetrically on both sides of the back of the nose. The photo below schematically shows the inflammatory process in the maxillary sinus.
The sinus is covered from the inside with mucous membrane. It secretes mucus, which contains substances that neutralize microbes. The formed mucus flows into the nasal cavity through a special anastomosis.
Special cilia (ciliated epithelium) help mucus move directionally from the sinus into the nasal cavity. They are in constant motion and, moving, create a kind of current that moves mucus to the anastomosis.
If the size of the anastomosis is normal, the contents of the sinus flow freely through it even during ARVI. If the size of the anastomosis is changed (for example, due to swelling), mucus may stagnate in the sinus. Changing the size of the maxillary sinus anastomosis can lead to various complications, including sinusitis.
All sinuses communicate with the nasal passages and with each other, so the inflammatory process of one sinus can spread to the others. According to medical statistics, in more than 70% of cases, sinusitis develops in two or more sinuses; in 1.5-2% of patients, sinusitis spreads to all sinuses. This very serious disease is called "pansinusitis" or "hemisinusitis" if all sinuses are affected, but only on one side.
In addition, the process can extend beyond the sinuses. Intraorbital inflammatory processes may occur. If an infection enters the orbit, thrombosis of the orbital veins may occur. With further infection in the brain, sinusitis can develop into meningitis and a brain abscess can develop, which can be fatal.
When to go to the hospital
If the main sinus is pneumatized and there is pneumatization in other sinuses, then this often manifests itself with certain symptoms. If signs of illness appear, you should see a doctor as soon as possible. The danger of inflammation of the nasal appendages is that they are in close proximity to other important organs. With sinusitis, inflammation of the brain can develop, which often leads to serious complications . The following symptoms should alert you:
- pain in the face, which intensifies when the head is tilted forward;
- feeling of fullness around the nose;
- prolonged nasal congestion and any amount of purulent discharge;
- heat;
- lacrimation;
- abnormal weakness and apathy;
- foul odor from the nose.
All these symptoms mean the onset of an inflammatory process in the sinuses. Only a specialist can make a correct diagnosis; you should not self-medicate, as you can waste precious time .
All pathologies that cause disturbances in the pneumatization of the nasal sinuses are highly treatable. But you need to understand that the earlier the correct diagnosis is made and treatment started, the more favorable the prognosis.
- X-ray of the sinuses for sinusitis - signs for identifying the disease
Pneumatization of the paranasal sinuses - what is it?
As shown in the image above, the sinuses are normally filled with air. In medical language this is called “pneumatized sinuses.” Pneumatized sinuses are responsible for the resonance and timbre of the voice, and also reduce the mass of the skull bones.
Thus, the meaning of such phrases as: “the frontal sinuses are pneumatized,” “the paranasal sinuses are pneumatized,” “the paranasal sinuses are pneumatized,” “the main sinus is pneumatized” means the normal healthy state of the paranasal sinuses. There's nothing to worry about.
Possible results of the conducted research
In the event of various inflammatory processes, if there is a suspicion of their presence, the attending physician writes a referral for an examination. This diagnosis consists of fluoroscopic examination.
Pneumatization of the paranasal sinuses can be diagnosed by several indicators.
Reduced. A decrease in pneumatization makes it possible to determine the presence of a pathological, inflammatory process. This phenomenon often happens when inflammation of the maxillary sinus occurs. In addition, the result of a decrease may be:
- the presence of caries or other infectious diseases of the teeth and oral cavity;
- the appearance of a cyst or other neoplasm;
- accumulations of exudate (presence of purulent or other fluid);
- congenital underdevelopment of the internal spaces of the nose.
Saved. This conclusion indicates the normal functioning of the organ. It is also the result of diagnosis when inflammatory processes of the maxillary sinuses were not detected.
- X-ray of the sinuses: features of the study
Promoted. An increase in standard indicators indicates possible disruptions in the functioning of the endocrine system (gigantism and acromegaly develop especially often).
What causes sinusitis?
Having understood the anatomy and various names of the disease, it is necessary to understand what causes sinusitis.
The main condition for the development of inflammation in the sinus is difficulty in the outflow of mucus. Normally, a small amount of mucous fluid is constantly formed in the maxillary sinus, which washes the inner walls of the sinus, removes microbes and flows through the anastomosis of the maxillary sinus with the help of the directed movement of special cilia of the ciliated epithelium.
If the outflow is disrupted, mucus stagnates in the sinus. Subsequently, microbes multiply in the stagnant mucus inside the sinuses. Pus forms and symptoms of sinusitis appear.
The outflow of mucus may be impaired as a result of edema - allergic or infectious, as well as against the background of various inflammations of the nose as a result of trauma to the nose or congenital anomalies in the structure of the nasopharynx (deviated nasal septum, abnormal development of the nasal turbinates, etc.).
One of the most common causes of sinus blockage is nasal congestion, as the anastomosis (entrance to the sinus) is blocked. Nasal congestion develops as a result of swelling (increase in the size of the mucous membrane) and accumulation of mucus. This leads to blocking the access of oxygen through the nose, including into the sinuses.
Infection in the maxillary sinuses can enter in several ways:
- Hematogenous. Microbes enter the sinuses from foci of infection in other organs through the bloodstream.
- Nasal. The infection enters from the nasal cavity through the sinus anastomosis.
- Odontogenic. The infection enters the sinuses from the inflamed roots of the upper 4 molars, which are in close contact with the walls of the sinuses. In addition, infection can enter through the canals of the teeth during various dental procedures.
- Traumatic. The infection occurs through various injuries to the nose, upper jaw and other bones of the facial skull.
The main reasons for the development of sinusitis:
- ARVI (acute respiratory viral infection);
- prolonged runny nose (more than 2 weeks);
- sore throat (tonsillitis);
- ear inflammation, otitis (otogenic sinusitis);
- caries of the upper 4 molars (odontogenic form).
Predisposition to the disease may be due to:
- low immunity;
- curvature of the nasal septum, adenoids, etc.;
- the presence of pathogenic bacteria in the nasopharynx, for example, Staphylococcus aureus, the rapid development of which occurs due to weakened immunity.
It should be remembered that untreated sinusitis can cause relapses (new cases) of the disease. This is due to the fact that after treatment with antibiotics, many dead cells remain in the sinuses. They “clog” the sinuses and become a favorable environment for the development of new inflammation.
Do not stop treatment just because you feel better. It is necessary to completely clear the maxillary sinuses. This can be done in several ways:
- by the body's own forces through the release of mucus through the nasal canals and with the help of lymphatic drainage through lymphatic capillaries and vessels.
- rinsing the sinuses with antiseptics;
- surgical operation (puncture or puncture).
To help your sinuses clear faster, you can help your immune system. You can stimulate the immune system and speed up the removal of toxins and dead cells using a special medical device called Vitafon. More information about the method of treating sinusitis in remission (weakening or disappearance of symptoms) using this device can be found here. Before use, carefully read the instructions and consult your doctor. This simple method will help avoid complications and serious surgical interventions in the future.
Psychosomatics: Louise Hay and Liz Burbo
Psychologists say that not a single emotion passes without a trace for us. Any negative experience affects our health, both psychological and physical. “Psychosomatics” studies the psychological causes of various diseases. Like many other diseases, sinusitis (sinusitis) can have psychosomatic (psychological) causes.
The most famous foreign scientists in this field are Louise Hay (USA) and Lise Burbo (Canada). According to Louise Hay, sinusitis is suppressed self-pity, unshed tears. A prolonged situation of “everyone is against me” and an inability to cope with it.
For a more accurate understanding of the psychosomatics of sinusitis, we can give an example:
A person has constant stress, he is always worried about himself and his loved ones, suppresses feelings of fear and self-pity. At the same time, he believes that the whole world is against him, and no one will help him. Over time, this becomes the norm. A constant feeling of fear leads to breathing problems, which becomes the root cause of a runny nose and sinusitis.
To change this situation, you need to reconsider your attitude towards life, do what you can do, and not be afraid to ask for help from the people around you. You don't have to be perfect, you just need to love yourself as you are.
It is worth understanding that psychosomatics is good in its time and place. If you have symptoms of sinusitis, you should consult a qualified doctor. Psychosomatics can be considered for the prevention of the disease or its repeated relapses (new cases of exacerbation of the disease).
What is sinusitis?
There are several types of this disease depending on the location, cause, features of development and complications of the disease.
| Type of sinusitis | Characteristic |
| Spicy | The duration of the disease is 2-3 weeks. The disease manifests itself once or occurs no more than once a year. The first symptoms are similar to ARVI and other colds. |
| Recurrent | The disease in its acute form recurs 2 to 4 times a year. The symptoms are similar to those of acute sinusitis. This type of disease develops due to insufficient cleaning of the contents and tissues of the maxillary sinuses after an illness, as well as against the background of weak immunity. |
| Chronic | The disease recurs more than 4 times a year or the disease lasts for 2 or more months. The symptoms either subside or reappear. This type of sinusitis can appear in the absence of proper treatment in the acute form of the disease. |
Depending on the cause of the disease (according to the etiological factor), sinusitis can be:
| Type of sinusitis | Characteristic |
| Viral | Triggered by a viral infection. According to the famous doctor E.O. Komarovsky viral sinusitis occurs with any acute respiratory viral infection (ARVI) and goes away with it, unless complications occur in the form of a bacterial infection. |
| Bacterial (aerobic and anaerobic) | It is caused by a bacterial infection and in most cases is a complication after ARVI. |
| Fungal | Develops as a result of decreased immunity and fungal infection. |
| Traumatic | As a result of injury. In case of violation of the integrity of the sinus, the type of disease will be determined as perforated. |
| Allergic | It manifests itself as an allergic reaction to allergens entering the body. |
| Iatrogenic | Occurs as a result of medical interventions. Most often found in dentistry. |
| Perforated | Violation of the integrity of the sinus as a result of trauma, complications of odontogenic or iatrogenic sinusitis. |
| Endogenous | It occurs as a result of internal processes occurring in the body. For example, as a result of otitis (otogenic sinusitis), due to pathological processes occurring in the apices of the roots of the upper teeth (odontogenic sinusitis) or vasomotor - due to vegetative-vascular dystonia, vasomotor rhinitis (runny nose) or long-term use of vasoconstrictor drugs (medicinal sinusitis ). |
| Mixed | When combining several causes (infections). |
According to the form of the disease.
Exudative (catarrhal). The disease is accompanied by the release of inflammatory fluid. Depending on its nature, there are:
- serous (discharge resembles watery fluid).
- mucous (discharge resembles mucus).
- purulent (discharge similar to pus).
Productive . These forms are accompanied by proliferation of the mucous lining of the sinuses. Depending on the nature of growth, they are divided into:
- parietal-hyperplastic (parietal sinusitis): characterized by thickening and swelling of the mucous membrane of the maxillary sinus, as well as the absence of purulent contents;
- polypous: growths in the nose and sinuses in the form of a polyp (thickening on a stalk).
If there are complications during the development of the disease, for example, the spread of the process to the orbit of the eyes, venous vessels and brain, this type of sinusitis is called complicated.
Depending on the prevalence of the process, unilateral sinusitis is distinguished, that is, the disease can be on one side (left-sided or right-sided sinusitis) and bilateral sinusitis. Regardless of the location of the disease, the inflammatory process can be acute, purulent, or any other of the above types.
Knowing the type of disease determines how to treat it!
Ultrasound in gray scale mode: diagnosis and evaluation of the effectiveness of treatment of maxillary sinusitis
Ultrasound machine RS85
Revolutionary changes in expert diagnostics.
Impeccable image quality, lightning-fast operating speed, a new generation of visualization technologies and quantitative analysis of ultrasound scanning data.
Introduction
The incidence of acute bacterial rhinosinusitis in our country tends to increase. Thus, according to the Moscow Department of Health, in the period 2012–2017. the number of patients has increased 1.9 times compared to the previous 15 years, while the number of patients with severe forms of this suffering has increased [1]. Acute rhinosinusitis is one of the most common diseases encountered in outpatient practice. In different countries, its incidence ranges from 15 to 40 episodes per 1000 patients per year, women suffer approximately twice as often as men, and the highest incidence occurs in working age from 25 to 44 years [2].
The presence of facial pain, difficulty in nasal breathing, purulent nasal discharge, impaired sense of smell, and unpleasant odor in the nose are the most common symptoms of sinusitis. The close proximity of the optic, trochlear, oculomotor and abducens nerves can lead to flashing spots before the eyes, impaired convergence, decreased vision, dizziness, nausea and even vomiting. Inadequate or insufficient and untimely therapy often contributes to the transition of acute sinusitis to a chronic form; it becomes recurrent and leads to the development of chronic bronchitis, pneumonia or bronchial asthma. The changing range of pathogens and the development of their resistance to previously used drugs complicate the choice of antibiotic therapy. It is believed that if there is no effect of initial therapy on the 7th day, a repeat diagnostic search should be performed [3].
The existing range of techniques most commonly used for this purpose includes anterior rhinoscopy, endoscopy, ultrasound scanning in A- and B-mode, diagnostic puncture, plain radiography and computed tomography of the paranasal sinuses (SNS). Anterior rhinoscopy, when mucopurulent secretion is detected in the middle nasal meatus, indicates the presence of sinusitis, but the absence of discharge does not exclude a pathological process in the sinuses.
Endoscopy of the nasal cavity allows you to visualize the discharge in the area of the anastomosis of the paranasal sinuses, however, a full endoscopic examination of the nasal cavity can be difficult if there is gross deformation of the nasal septum. Ultrasound scanning in A-mode, due to the difficulty of interpreting the data obtained, often does not allow differentiating a cyst or polyp from mucosal edema and a liquid component.
A diagnostic puncture does not give an idea of the condition of the walls and mucous membrane, the presence of polyps and other formations, although it allows one to obtain the contents of the sinus or prove its absence.
Plain radiography is the main method for diagnosing the paranasal sinuses. The agreement rate between radiography and computed tomography for maxillary sinusitis is 77% [4].
Computed tomography of PPN is the “gold standard” in the diagnosis of sinusitis; it serves as a reliable basis for planning surgical treatment. However, its use for monitoring during conservative treatment is limited due to high cost and radiation exposure.
Ultrasound scanning of the maxillary sinuses in gray scale mode (B-mode) has been used for more than 15 years and not only in cases where it is necessary to exclude exudative sinusitis in a group of people who have contraindications to x-ray examination, but also for monitoring during treatment [5] , however, the frequency of its use is small and does not exceed 4%, while the frequency of use of radiation methods is 87% [2].
To illustrate the capabilities of ultrasound examination of the maxillary sinuses in gray scale mode, we present the following clinical observations in which the study was performed on a modern expert-class ultrasound device. Ultrasound was performed with the patient sitting and facing the examiner using a linear sensor with a frequency of 7.5 MHz in sagittal and horizontal sections; the lower wall of the orbit, which is the upper wall of the maxillary sinus, served as a guide for finding the maxillary (maxillary) sinus.
Clinical observation 1
Patient N., 25 years old, consulted an otolaryngologist with complaints of congestion in the left half of the nose. Ultrasound of the left paranasal sinus in A-mode reveals an expansion of the initial complex (Fig. 1a), in B-mode the posterior wall is not visualized, since the pneumatization of the sinus is preserved, thickening of the mucous membrane up to 15 mm is noted - a picture of left-sided maxillary catarrhal sinusitis (Fig. 1b).
Rice. 1.
Catarrhal maxillary sinusitis.
A)
Echogram of the left maxillary sinus in A-mode.
b)
Echogram of the left maxillary sinus in B-mode.
As is known, catarrhal sinusitis is characterized by swelling of the mucous membrane, cellular infiltration of all its layers with leukocytes, due to which in B-mode a weakly echogenic zone with a clear distal contour appears directly behind the bone base of the anterior wall of the sinus, which, when examined in A-mode, corresponds to an expansion of the initial complex. In this observation, there are no reflections from the posterior wall either during ultrasound in gray scale mode or in A-mode, that is, pneumatization of the sinuses is preserved.
Visualization of the posterior wall is possible only if pneumatization is impaired and depends on the amount of secretion or other contents: the more secretion, the more complete the view of the walls will be. The line of separation of media, which would correspond to the X-ray concept of “liquid level,” is not visible with ultrasound, since the ultrasound beam passes parallel to this line [6]. Consequently, the amount of exudate must be judged by the extent of visualization of the posterior wall in the sagittal section.
Clinical observation 2
Patient V., 40 years old, complained of nasal congestion and pain in the projection of the left maxillary sinus. Ultrasound of the paranasal sinuses on the right shows uniform thickening of the mucous membrane (Fig. 2a), on the left - a violation of pneumatization: the posterior wall is visible to the level of the infraorbital foramen (Fig. 2b). An additional hyperechoic arc is the cyst wall. An X-ray taken on the same day shows a total darkening of the left maxillary sinus; MSCT on the left confirmed the presence of a cyst.
Rice. 2.
Right-sided exudative maxillary sinusitis. Cyst of the right maxillary sinus.
A)
Echogram of the right maxillary sinus in B-mode. Thickened mucous membrane is marked with calipers.
b)
Echogram of the left maxillary sinus in B-mode. Arrows mark the wall of the cyst.
Clinical observation 3
Patient E., 49 years old, complained of nasal congestion, mucous discharge, and discomfort in the zygomatic region. Ultrasound in A-mode in both maxillary sinuses shows a significant expansion of the initial complex and on the right - an additional peak from the posterior wall (Fig. 3a), on the radiograph on the right - subtotal darkening, on the left - parietal thickening of the mucosa (Fig. 3b). Ultrasound in B-mode shows exudate on the right, filling almost the entire volume of the sinus (Fig. 3c), and on the left – parietal thickening of the mucous membrane up to 14 mm (Fig. 3d). There is complete agreement between the results of ultrasound and radiography. After 7 days of conservative treatment, complete restoration of pneumatization on the right was noted (Fig. 3e) and a significant decrease in the thickness of the mucosa on the left (Fig. 3f).
Rice. 3.
Right-sided exudative maxillary sinusitis dynamics before and after treatment.
A)
A-mode echogram of the maxillary sinuses before treatment.
b)
X-ray of the paranasal sinuses before treatment.
V)
Echogram of the right maxillary sinus in B-mode before treatment.
G)
Echogram of the left maxillary sinus in B-mode before treatment.
d)
Echogram of the right maxillary sinus in B-mode after treatment.
e)
Echogram of the left maxillary sinus in B-mode after treatment.
Clinical observation 4
Patient Yu., 36 years old, complained of a feeling of pressure in the area of the right maxillary sinus. Ultrasound (Fig. 4a) shows pneumatization of the right maxillary sinus is preserved, the posterior wall is not visualized, the mucosa is thickened, and the thickening is heterogeneous, with point hyperechoic inclusions. MSCT (Fig. 4b, c) also reveals uneven thickening of the mucosa, with an area of heterogeneous compaction – a fungal body (mycetoma). Dense inclusions represent deposits of phosphate and calcium sulfate in areas of necrosis of mycetoma - a picture of non-invasive fungal sinusitis. The patient was operated on and the diagnosis was confirmed.
Rice. 4.
Non-invasive fungal maxillary sinusitis.
A)
Echogram of the right maxillary sinus in B-mode.
b)
MSCT of the paranasal sinuses. Axial projection.
V)
MSCT of the paranasal sinuses. Frontal projection.
Clinical observation 5
Patient N., 43 years old, complained of difficulty in nasal breathing, mucus running down the back of the throat, discomfort in the left zygomatic region, and headaches. On ultrasound, pneumatization of the right maxillary sinus is preserved; a cyst measuring 11 x 9 mm is visualized in the lower part near the anterior wall (Fig. 5a), the left maxillary sinus is airless (Fig. 5b), the picture resembles exudative sinusitis, but the posterior wall has a double contour, and this sign indicates that this is not a free exudate, but a large cyst, which is confirmed by the results of MSCT (Fig. 5c, d).
Rice. 5.
Maxillary sinus cysts.
A)
Echogram of the right maxillary sinus in B-mode. Arrows mark the wall of the cyst.
b)
Echogram of the left maxillary sinus in B-mode. Arrows mark the wall of the cyst.
V)
MSCT of the paranasal sinuses. Frontal projection.
G)
MSCT of the paranasal sinuses. Axial projection.
Clinical observation 6
Patient K., 38 years old, complained of difficulty in nasal breathing, mucopurulent discharge from the nasal cavity, headache, and low-grade fever. On ultrasound, the pneumatization of the right maxillary sinus is disrupted, the posterior wall is visible, which has a single contour in contrast to the previous observation, and near the anterior wall there is an additional arch, which is the wall of the cyst (Fig. 6a). The presence of exudative sinusitis was confirmed x-ray: the right maxillary sinus is completely darkened (Fig. 6b). Despite the treatment, after 4 days, no dynamics were noted on ultrasound, which served as the basis for a puncture, during which purulent discharge was obtained, the sinus was washed with a dioxidine solution. As a result, during control ultrasound 2 days later, pneumatization of the sinus was restored, the posterior wall was not visible, and a small cyst remained near the anterior wall (Fig. 6c).
Rice. 6.
Right-sided exudative maxillary sinusitis. Treatment control.
A)
Echogram of the right maxillary sinus in B-mode before treatment. Sagittal projection.
b)
X-ray of the paranasal sinuses before treatment.
V)
Echogram of the right maxillary sinus in B-mode after treatment. Axial projection.
Clinical observation 7
Patient B., 28 years old, complained of difficulty in nasal breathing, mucopurulent discharge from the nose, headache, and was treated with vasoconstrictor drugs for a week and a half. It is known that he suffers from chronic sinusitis with exacerbations 1-2 times a year. On the radiograph (Fig. 7a) in the right maxillary sinus there is a pronounced thickening of the mucosa, in the left - against the background of parietal thickening of the mucosa, the level of fluid is determined up to 1/3 of the volume of the sinus; the same words can be used to describe the ultrasound picture (Fig. 7b, c). Antibiotics and topical corticosteroids were prescribed. After 4 days, the ultrasound picture was without the slightest dynamics (Fig. 7d), and therefore the sinus was punctured, washed and filled with dioxidine (Fig. 7d): it is transparent to ultrasound and makes it possible to examine in detail the thickened mucosa - uniform along the anterior wall and in the form several polyps along the posterior wall.
Rice. 7.
Polypous polysinusitis. Treatment control.
A)
X-ray of the paranasal sinuses before treatment.
b)
Echogram of the left maxillary sinus in B-mode before treatment. Sagittal projection.
V)
Echogram of the left maxillary sinus in B-mode before treatment. Axial projection.
G)
B-mode echogram of the left maxillary sinus 4 days after the start of treatment. Axial projection.
d)
Echogram of the left maxillary sinus filled with dioxidine solution in B-mode 4 days from the start of treatment. Sagittal projection.
e)
B-mode echogram of the left maxillary sinus 8 days after the start of treatment. Sagittal projection.
and)
Echogram of the left maxillary sinus in B-mode 15 days from the start of treatment. Sagittal projection.
h)
B-mode echogram of the left maxillary sinus 36 days after the start of treatment. Sagittal projection.
And)
MSCT of the paranasal sinuses. Axial projection.
To)
Echogram of the right maxillary sinus in B-mode after 2 years. Sagittal projection.
l)
B-mode echogram of the left maxillary sinus after 2 years. Sagittal projection.
After another 4 days (8th day from the start of treatment), against the background of ongoing therapy, the ultrasound picture is completely restored: the sinus is again filled with heterogeneous contents (Fig. 7f), and only after another week the amount of content decreases, pneumatization is partially restored (Fig. 7g) . However, after 3 weeks the original picture completely returned (Fig. 7h), MSCT confirmed the presence of polyposis polysinusitis (Fig. 7i), the patient underwent surgical treatment and has been feeling well for two years. After 2 years, during pregnancy, nasal congestion reappeared; an ultrasound scan on the 2nd day of illness revealed bilateral exudative maxillary sinusitis (Fig. 7j, l); the sinuses were washed through the anastomosis formed during surgical treatment; a large amount of thick viscous mucus was obtained; treatment: Aqua-Maris, Nasonex, irrigation therapy, intranasal glucocorticosteroids (mometazole). Thanks to timely actions, stable remission was quickly achieved.
Conclusion
The sensitivity of ultrasound for impaired pneumatization is 100%. In determining its cause, be it swelling of the mucous membrane, the presence of exudate, cysts or polyps, ultrasound naturally cannot compete with computed tomography. For swelling of the mucous membrane, the sensitivity of ultrasound is 82.3%, the specificity is 66.7%, for cysts - 66.7 and 33.0%, for polyps - 90.9 and 62.5%, respectively [7]. But a comparative analysis of the information content of plain radiography and ultrasound diagnostics showed the absence of statistically significant differences between them [8], that is, the otolaryngologist has the right to expect from ultrasound the same information as from plain radiography, with the only difference being that ultrasound also provides multiple, quick, harmless, visual and objective assessment of the effectiveness of treatment. The desire to comply with the principles of evidence-based medicine dictates the need for more widespread use of ultrasound of the paranasal sinuses in outpatient practice.
Literature
- Kozlov V.S., Gorbunov S.A., Kudryashov S.E. Analysis of experience in the use of nasal catheters in acute bacterial rhinosinusitis // Bulletin of Otorhinolaryngology. 2020; 85 (6): 46–51.
- Savlevich E.L., Kozlov V.S., Farikov S.E. Analysis of modern schemes for the diagnosis and treatment of acute rhinosinusitis according to the outpatient service of polyclinics of the Administration of the President of the Russian Federation // Bulletin of Otorhinolaryngology. 2020; 85 (4): 51–57.
- Gurov A.V., Zakarieva A.N. Possibilities of modern macrolides in the treatment of acute purulent sinusitis // Consilium medicum. 2010: 12 (3): 31–35.
- Ryazantsev S.V., Karneeva O.V., Garashchenko T.I., Gurov A.V., Svistushkin V.M., Sapova K.I., Kazanova A.V., Maksimova E.A. Acute sinusitis. Clinical guidelines of the National Medical Association of Otolaryngologists. M., 2016. 30 p.
- Shilenkova V.V., Kozlov V.S., Byrikhina V.V. Two-dimensional ultrasound diagnostics of the paranasal sinuses: A manual. Yaroslavl, 2006. 54 p.
- Vasilchenko S.A., Sergeeva T.A., Valitova L.N., Khabarova E.G., Burkov S.G. Ultrasound visualization of the maxillary sinuses: experience of use for sinusitis in an outpatient setting // Kremlin Medicine. 2012; 1:65–68.
- Byrikhina V.V. Two-dimensional ultrasound diagnosis of diseases of the paranasal sinuses: Abstract of thesis. dis. ...cand. honey. Sci. M., 2007.
- Shilenkova V.V., Byrikhina V.V., Karpov V.A., Shargin V.V., Korsun A.A. Comparative analysis of the information content of two-dimensional ultrasonography in the diagnosis of paranasal sinuses in adults and children // Russian Otorhinolaryngology. 2005; 1 (14): 129–132.
Ultrasound machine RS85
Revolutionary changes in expert diagnostics.
Impeccable image quality, lightning-fast operating speed, a new generation of visualization technologies and quantitative analysis of ultrasound scanning data.
Diagnosis of sinusitis
Based on the patient's complaints, the doctor can make a preliminary diagnosis. But it is possible to say for sure whether there is sinusitis or not only after additional examination methods and the necessary tests.
Additional research methods for sinusitis
- X-ray examination of the paranasal sinuses (x-ray/x-ray). This is the most common, accessible and inexpensive method. During this study, the body experiences severe radiation exposure. This study is not suitable for pregnant women; in addition, an x-ray cannot determine the cause and nature of inflammation (mucous or purulent) of the disease. There are other methods for this.
- Computed tomography (CT) is a very informative, but expensive method. In addition, not all medical institutions have the necessary equipment. Therefore, it is not used often, only in difficult cases to clarify the diagnosis. In addition, this method is contraindicated during pregnancy.
- Magnetic resonance imaging (MRI) is also used only in complex cases to clarify the diagnosis. Not all medical institutions have the necessary equipment.
- Ultrasound of the maxillary sinuses. The method is very informative for sinusitis and has virtually no contraindications. It is rarely used, as it requires special equipment and trained personnel. On the other hand, this method is suitable for pregnant women.
- Therapeutic and diagnostic puncture (puncture). It is considered the “gold standard for diagnosis” in the absence of other methods. It is an invasive (requiring a puncture of the skin or mucous membrane) procedure during which the contents of the sinus cavity are obtained.
- Laboratory research methods. A general blood test for sinusitis will show signs of an inflammatory process: increased ESR - above 12 mm/h, increased number of leukocytes, detection of the presence of bacterial inflammation (which makes it possible to distinguish a bacterial type of disease from a viral one). The method is auxiliary to confirm the presence of the disease; it alone is not enough.
Sinusitis is a serious disease, so only the attending physician can accurately diagnose the disease and determine what tests are needed. After the doctor has made a diagnosis, the patient must strictly but consciously follow his recommendations in order to avoid complications and ultimately get rid of this disease.
MRI of the sinuses, how a scan is done
The patient is placed on a table that moves inside the tomograph. There is no radiation exposure during this examination. MRI shows sections in different planes, without the need to change the position of the body. The procedure takes about 20 minutes and is very comfortable. There is good air ventilation inside the scanner and soft lighting.
In cases where the use of intravenous contrast is recommended, the study will take a little longer (about 15 minutes additional). After completing the tomography, you can immediately return to your normal lifestyle.
What does sinusitis look like on an x-ray?
It is difficult for an ordinary person to identify sinusitis in an image; future doctors are taught this at the institute. We will help our readers learn to identify the disease in photographs.
The image shows the paranasal sinuses. Normally, they appear dark on both sides of the nose. The color of the sinuses in the photo should match the color of the eye sockets.
In the picture (see photo) we see a discoloration on the right side in the sinus area (right-sided sinusitis)
If a discoloration is visible in the area of the paranasal sinuses on both sides, then this is bilateral sinusitis.
Note: An x-ray is a negative, just like regular photographic film. Dense structures (bones, edema, inflammatory fluid) are light in color in the image. Less dense structures and air are darker. Therefore, when the sinuses acquire a lighter color in the picture, they speak of darkening, total or subtotal (complete or incomplete) - accordingly, these are signs of sinusitis.
In this photo you can see an x-ray before and after treatment of sinusitis.
Questions that often arise:
Where to take an x-ray of the maxillary sinuses?
X-rays of the paranasal sinuses can be done in a clinic or hospital as prescribed by the attending physician if they have an X-ray machine appropriate for the task.
How often can an x-ray be taken?
There is no definite answer, there are only contraindications. At least one x-ray is necessary to diagnose the disease and it is advisable to undergo an examination after treatment to ensure that the sinuses are clean. However, in some cases additional images may be required. Your doctor will determine the required number of images.
The first signs and symptoms of sinusitis
Symptoms of sinusitis are very similar to those of ARVI and influenza: fever, runny nose, decreased sense of smell, general malaise. Subsequently, these symptoms intensify and signs characteristic of bacterial sinusitis join:
- pain in the sinuses;
- headache;
- dizziness;
- unpleasant odor from the nasopharynx.
Possible coughing, bleeding from the nose, nausea, toothache, swelling and pain in the eyes.
How to identify and recognize sinusitis?
In the initial stages of sinusitis, signs and symptoms may not be expressed; sometimes sinusitis occurs without fever, runny nose and nasal congestion, so you need to remember what symptoms of sinusitis will help you recognize it.
Temperature
The temperature during sinusitis can vary from very high (over 39 °C) to low-grade (within 37 °C) and normal. This depends on the age of the patient, the type of disease, the state of immunity, and the presence of concomitant diseases in the patient.
In some cases, the disease can be very insidious. It would seem that the runny nose has gone away, the temperature has returned to normal, and suddenly pain and heaviness appear in the sinuses. In this regard, it should be remembered that sinusitis can be without fever, runny nose and nasal congestion, so the main symptom is still pain in the area of the maxillary sinuses.
Inflammation of the sinuses - pain in the sinuses
In most cases, inflammation of the maxillary sinuses is accompanied by a symptom such as pressing pain in the sinuses. This is due to the fact that the inflammatory fluid presses on the walls of the sinus, as a result, the pressure in them increases and the pain nerve endings are irritated. Pain in the maxillary sinuses is most severe when bending or making sudden movements of the head. This symptom will help to recognize the disease, especially if sinusitis without a runny nose.
Headache
A headache with sinusitis can be felt in the forehead, nose, cheekbones, and sometimes radiates to the back of the head. With inflammation of the maxillary sinuses, the pain can be severe, pressing, bursting. The feeling of pressure in the forehead and bridge of the nose increases when the head is tilted.
Discharge and blood from the nose
Nasal discharge is mucous or mixed with pus, and sometimes with blood clots. The discharge (snot) may have an unpleasant odor. The color of nasal discharge may vary depending on the stage of the disease, from white, transparent to yellowish-green. Regardless of the type of snot associated with sinusitis, whether it exists or not, if the above symptoms occur (headache, fever and pain in the sinuses), you should immediately consult a doctor.
Nosebleeds, snot and runny nose with blood during sinusitis can be associated with frequent blowing of the nose and damage to small vessels.
But sometimes there may be no discharge. This condition is called "dry sinusitis."
Sinusitis without nasal discharge
Sinusitis can occur without nasal discharge. This is observed with very severe swelling, when mucus does not flow out of the sinus at all. Other symptoms of sinusitis come to the fore: sinus pain, headache, fever and nasal congestion.
Nasal congestion
Nasal congestion is associated with swelling of the mucous membrane of the nasal passages and maxillary sinuses, including without the formation of pus. Swelling may be accompanied by snot and an unpleasant smell in the nose when you have a runny nose.
Unpleasant odor from the nasopharynx
This sign appears at the height of the disease and indicates the addition of microbial putrefactive flora, which is the cause of the unpleasant odor of pus in the nose.
Cough
Inflammation of the sinuses may occur with a cough. This is due to the fact that mucus flows into the oropharynx. Cough with sinusitis worsens at night and when lying down.
Dizziness and nausea
Sometimes dizziness occurs with sinusitis. Nausea and dizziness can be associated with intoxication of the body, inflammation and increased pressure in the maxillary sinus. Dizziness, nausea, headache, temperature above 37 ° C, nasal discharge - these signs are characteristic of an acute process. In the chronic form of the disease, such symptoms may not be expressed clearly.
Toothache
Toothache with sinusitis is an uncommon symptom. It can appear with a long-term disease, the accumulation of a large amount of pus in the nasal sinuses and the spread of the process to the roots of the 4 upper teeth, which are closely adjacent to the lower wall of the maxillary sinus.
There may also be a reverse process, when first the teeth hurt, and then sinusitis develops. This is observed with advanced caries of molars. Pathological processes occurring in the apices of the roots of the upper teeth extend to the maxillary sinus. This type of disease is called odontogenic.
Pain in the eyes
Inflammation of the maxillary sinuses may cause swelling of the eyelids and pain in the eyes. This suggests that the purulent process has spread to the orbit (orbital region). This is an extremely dangerous symptom, since there is a danger of pus breaking through the thin wall of the orbit and through the vessels into the brain.
It should be remembered that sinusitis is not just nasal congestion and runny nose. This is a serious disease and, in the absence of timely and qualified treatment, can lead to serious complications. At the first signs of the disease, you should consult a doctor and not self-medicate.
Indications and contraindications for MRI of the sinuses
Magnetic resonance imaging is necessary in the following cases:
- prolonged headaches, especially pain in the face;
- repeated nosebleeds;
- treatment-resistant nasal congestion;
- impaired sense of smell;
- suspicion of a neoplasm;
- injuries to the facial area;
- congenital anomalies of the nasal cavity and sinuses;
- pathologies identified by X-ray or ultrasound results;
- postoperative observation.
All sinuses communicate with each other, so infectious processes (the most common pathology in this area) can pass from one sinus to another.
Acute sinusitis
Its main signs on MRI are a decrease or increase in signal intensity from the mucous membrane. Changes in the bone walls of the sinuses are possible in the form of thickening or destruction.
Signs of sinusitis and ethmoiditis on MRI
Chronic rhinosinusitis
MRI is of particular importance for inflammation of a fungal nature, which is difficult to diagnose by other methods. It is more common in young people with concomitant bronchial asthma, who are forced to constantly use inhaled corticosteroids, suppressing local immunity. Fungal sinusitis can also result from chronic infection in people with weakened immune systems. This case is characterized by severe difficulty in nasal breathing, thick, difficult to separate secretions in the nasal passages and sinuses, and rapid progression.
On MRI, the inflamed mucous membrane and the exudate contained in the sinus give an intense signal, in the center of which a low-intensity formation is determined, surrounded by a layer of fluid (the so-called “fungus ball”). With other research methods, it can be mistaken for air. MRI is the most informative method of differential diagnosis in this case.
Fungal sinusitis on MRI
Polypous rhinosinusitis
This is a disease of the mucous membrane, which is manifested by the progressive growth of polyps. The local process is often associated with chronic purulent inflammation. Diffuse polyposis, spreading to all paranasal sinuses, is most likely already caused by a decrease in the immunity of the whole organism.
MRI reveals formations of soft tissue density, heterogeneous in structure, sometimes with areas of cartilaginous density. Magnetic resonance imaging in this case helps to differentiate polyps from a tumor process.
Mucocele
This is a benign cyst-like formation of the sinuses. Most often it is a consequence of chronic inflammation and affects the frontal sinus.
On MRI, the sinus appears dilated, but with preserved airiness, and the image intensity is reduced. Magnetic resonance imaging makes it possible to distinguish it from cysts, sinusitis and polyposis. In the case where there is bone damage, it is differentiated from malignant formations. The prognosis is most favorable with early diagnosis and timely treatment.
Tumor diseases
Among benign neoplasms, the greatest clinical significance is:
- papillomas (from respiratory epithelium);
- adenomas (from glandular structures of the mucous membrane);
- vascular tumors;
- osteomas (from bone tissue);
- chondromas (made of cartilage tissue).
Manifestations of nasal and sinus tumors in the early stages are usually minimal and nonspecific. Some types may not produce clinical symptoms for years and are accidentally detected on MRI performed for other indications. Complaints may appear even when the tumor grows beyond the nasal sinuses. May appear:
- deformation of the nose or face;
- double vision;
- lacrimation (with compression of the nasolacrimal duct);
- decreased vision (with compression of the optic nerve);
- meningitis (if it spreads into the cranial cavity).
Often the only symptom may be a headache. This is due to the peculiarities of the innervation of this area. If a benign sinus disease has already been diagnosed, then the appearance of pain may indicate the addition of a secondary infection or malignant degeneration; a mandatory MRI is required.
Treatment of all tumors of the nasal sinuses is surgical and timely accurate diagnosis plays a great role in the prognosis of the disease.
Magnetic resonance imaging is the main diagnostic method for malignant processes in the sinuses and makes it possible to determine the nature, stage, boundaries, choose the right method of surgical treatment and carry out postoperative monitoring.
Hemangioma of the maxillary sinus on MRI (indicated by arrows)
MRI is contraindicated:
- pregnant women in the first trimester;
- if there are implants or foreign bodies containing metals with ferromagnetic properties in the patient’s body;
- if the patient has electronic devices installed (pacemaker, insulin pump, cochlear implant or others)
- if the patient suffers from claustrophobia or has an unstable mental state;
- in the presence of vascular clips on the arteries.
Children under 5 years of age and adults with a body weight of more than 130 kg or a waist circumference of more than 150 cm are not examined in our clinic.
Complications and consequences
Without adequate treatment, sinusitis can cause serious complications. Acute sinusitis can become chronic and then plague you with constant exacerbations. Well, that's not the worst part. The terrible consequences of sinusitis in adults and children are meningitis, brain abscess, thrombosis of the cavernous sinuses (blood vessels), and swelling of the optic nerves. These complications of the disease require serious treatment in a hospital setting.
If after the main treatment of sinusitis the temperature remains at 37 ° C, this means that the inflammatory process in the body continues or ends. If the temperature persists for a week, this means that the source of inflammation is not completely cured and you need to see a doctor again.
After sinusitis, residual effects in the form of nasal congestion may persist. This is due to hypertrophy (parietal thickening) of the mucous membrane of the maxillary (maxillary) sinuses and their incomplete cleansing of dead cells.
Vibroacoustic therapy using the Vitafon medical device allows you to eliminate these phenomena at home. More detailed information about the device and methods of treating sinusitis in remission can be found here.
Having analyzed the reviews about the Vitafon device, we can say that the device gives positive results only with correct and long-term use. To get a good result from Vitafon treatment, read the instructions and consult with your doctor.
FAQ:
How to understand that sinusitis is going away?
There are several signs (symptoms) of recovery: body temperature drops to normal or subfebrile 37–37.2 oC, purulent discharge stops, when the sinuses are washed there is no purulent discharge, the sense of smell returns, headaches and pain in the nose, sinuses and forehead disappear.
But remember that you cannot stop treatment on your own. Otherwise, you risk getting chronic sinusitis. Your attending physician can determine that sinusitis has been cured after the necessary examinations.
Is sinusitis contagious?
Sinusitis itself is not contagious to others, is not an infectious disease and is not transmitted by airborne droplets from person to person, but it must be remembered that it often occurs against the background of ARVI and other viral and bacterial diseases transmitted by airborne droplets, which are very contagious.
Is it possible to walk in winter?
You can’t walk if you have sinusitis in winter. Since cold air will increase blood supply and activate the glands of the sinuses. As a result, the amount of mucus in the sinuses will increase, and with complicated outflow, this will only worsen the situation. In addition, general hypothermia of the body and sinuses also negatively affects the healing process.
Is it possible to smoke?
Tobacco smoke greatly irritates the nasopharynx and, penetrating into the sinuses, increases their secretion. In addition, substances found in tobacco smoke impair the absorption of vitamin C, and the walls of blood vessels become fragile. The answer is obvious - smoking with sinusitis is contraindicated.
How long does the temperature last?
A high temperature indicates the severity of inflammation and the body’s resistance. In the acute form, a high temperature (above 38 ° C) usually lasts for 3-4 days in case of adequate treatment. If treatment is ineffective or delayed, the temperature may remain high for a longer time. A low temperature (up to 37.8 °C) may persist throughout the entire treatment until complete recovery. With chronic sinusitis, the temperature may be normal or not high throughout the entire process.
Is your nose breathing?
One of the signs of the disease is impaired nasal breathing and nasal congestion. In some cases, the nose does not breathe with sinusitis, but periodically the nose can breathe (first one or the other nostril).
How to distinguish sinusitis from a runny nose?
A normal runny nose lasts no more than 2 weeks. Also, with a normal runny nose, there is no unpleasant smell from the nose, soreness of the sinuses and severe headache. In any case, symptoms such as nasal congestion, runny nose and high fever, regardless of duration, require consultation with a doctor.
The following medical literature was used in preparing the article:
- "Bulletin of Otorhinolaryngology", No. 2, 2015.
- Clinical and morphological features of chronic inflammation of the maxillary sinus. Palchun V. T., Mikhaleva L. M., Gurov A. V., Muzhikova A. V. // Journal “Fundamental Research”. – 2010 – No. 7.
- Clinical otolaryngology. Textbook - Mishenkin N.V., Drachuk A.I., Ivanov L.I., Dashkevich Yu.M. Omsk, 1990
- Otorhinolaryngology. Textbook - Kiselev A., Usachev V.I., Soldatov I.B., St. Petersburg, 2000.
- Differential X-ray diagnosis of lesions of the paranasal sinuses, tumors of the skull and brain, cranial injuries, intracranial and extracranial foreign bodies: recommendations for practitioners. M. Kh. Faizullin. — Kazan, 1971
- "Listen to your body." Liz Burbo, 2008
Author of the article: doctor Patrusheva E.V.
You can ask questions (below) on the topic of the article. We will try to answer them competently.
Clinical picture
Mostly during an exacerbation, patients complain of difficulty breathing through the nose and discharge from the nasal cavity, which can be mucous, mucopurulent or purulent.
The purulent form of the disease is accompanied by complaints of discomfort in the area of the canine fossa and the root of the nose from the inflamed maxillary sinus. In some cases, pain may radiate to the superciliary or temporal region. Headache during an exacerbation is most often diffuse in nature, resembling trigeminal neuralgia. Hyposmia or anosmia (decreased or loss of sense of smell) is often observed. Quite rarely there are cases of closure of the nasolacrimal duct, and then lacrimation from the eye is observed.
Hyperplastic bilateral maxillary sinusitis occurs. During the period of exacerbation, along with all the signs of this disease, general weakness, malaise, and high (febrile) temperature (38-390C) are noted.
Friends! Timely and correct treatment will ensure you a speedy recovery!