Cheilitis is an inflammation of the red border, mucous membrane and skin of the lips. In common parlance, the disease is called jamming. The inflammatory process can be long-lasting and periodically worsen. In healthy young people it often goes away on its own, but in children, the elderly and people with chronic diseases it should be treated with medication. Elderly people have a high risk of leukoplakia and malignancy of the process.
Cheilitis is treated by a dentist, and if necessary, a therapist, pediatrician and other specialized specialists - an endocrinologist, an infectious disease specialist, etc. - are involved in drawing up a treatment plan.
Causes of cheilitis
Cheilitis can be an independent disease and a manifestation of other pathologies of the mucous membranes and internal organs. The most common causes of the disease include:
- Dermatoses. The mucous membranes and skin of the lips can be involved in the pathological process in lichen planus, psoriasis, erythematoses and other skin diseases.
- Unfavorable factors. Exposure to hot and cold air, wind, and excessive exposure to UV rays are especially common causes of cheilitis in people who work outdoors and under special weather conditions.
- Allergic reactions. Allergies can be triggered by chemical factors, ultraviolet rays, cosmetics, etc.;
- Other diseases. Secondary cheilitis often develops against the background of atopic dermatitis, eczema, neuritis of the facial nerve, etc.
Natural protective mechanisms are weakened by such factors as hypothermia, previous surgical interventions, long-term antibacterial therapy, hypovitaminosis, etc.
Ask a Question
Symptoms and types of disease
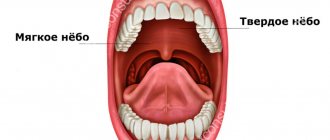
Cheilitis on the lips can manifest itself in different ways depending on the form of the disease. Thus, the exfoliative type of inflammation appears more often in women; its main symptom is peeling. The disease is based on neurological and endocrine disorders. Peeling occurs on the red border of the lips and does not affect the skin and mucous membranes. The disease rarely spreads to the entire red border, so part of it remains unchanged.
With severe dry skin, peeling is accompanied by symptoms such as:
- feeling of dry lips;
- burning;
- formation of easily detachable scales.
The disease is long-term and sluggish, with periods of exacerbation occurring from time to time. It rarely goes away on its own. With the exudative form, pain, swelling of the lips, and the formation of large crusts may occur.
Glandular cheilitis develops against the background of the proliferation of minor salivary glands and their subsequent infection. With congenital pathologies, signs of such inflammation of the lips are present in almost all cases. Acquired overgrowth may be associated with chronic diseases of the periodontal tissues, tartar, multiple caries - diseases leading to infection of the dilated ducts. Lesions of the lower lip with this form of cheilitis are more common. The disease develops with the appearance of dry lips, which is initially easy to correct with the help of cosmetics. Subsequently, cracks begin to form, deepen and begin to bleed. The condition is aggravated by the constant desire to lick dry lips - cracks and ulcers can become weeping and become permanent due to the inelasticity of the skin of the lips.
Contact allergic cheilitis develops after exposure to an allergen - an irritant. The most common of them are components of lipsticks and other care products. Allergies can also be associated with bad habits, for example, constantly keeping pencils, pens and other foreign objects in the mouth. Musicians may develop occupational cheilitis due to constant contact of the mouthpieces of wind instruments with their lips. The main symptoms of the disease include:
- severe itching;
- burning;
- swelling of the lips;
- redness of the skin and mucous membranes.
Manifestations intensify upon contact with the allergen. Bubbles of different sizes may form; their spontaneous or accidental opening leads to the formation of ulcers and cracks. Chronic forms of allergic disease are accompanied by peeling, slight itching and the absence of other signs of inflammation.
Actinic cheilitis belongs to the category of diseases that are based on increased sensitivity to weather and other external factors. Usually occurs in response to sun exposure. Exudative forms of this disease are accompanied by the formation of crusts. Sometimes small blisters form, the opening of which leads to painful erosions. In the absence of exudate, the main symptoms are pain, dryness, and burning of the lips. Actinic cheilitis often degenerates into precancerous diseases.
In atopic cheilitis, the main cause of the disease is dermatitis of the same name, or neurodermatitis. It appears in people with an allergic predisposition, and the triggering factor can be medications, cosmetics, food products, as well as microorganisms and their waste products. The disease is accompanied by redness of the lips, itching and peeling of the red border, and damage to the corners of the mouth. After acute symptoms subside, peeling and thickening of the skin may occur. Dryness stimulates the formation of cracks.
Macrocheilitis is part of the Rossolimo–Melkersson–Rosenthal syndrome. Appears against the background of neuritis of the facial nerve and the symptom of a folded tongue. Develops due to infectious-allergic effects against the background of genetic predisposition. Manifests itself with the following symptoms:
- lip enlargement;
- severe itching;
- swelling of other parts of the face;
- bluish-pink color of swollen areas of the lips.
One or both lips, cheeks, and upper parts of the face may be affected. Neuritis leads to facial asymmetry, and the nasolabial fold is smoothed out.
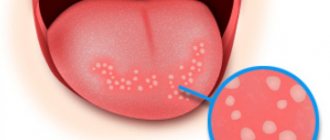
Hypovitaminous cheilitis of the lips develops against the background of a deficiency of B vitamins. Burning and dryness of the oral mucosa and lips appear. The mucous membranes become swollen and red, peeling occurs on the red border, and cracks appear. They are prone to bleeding, which is also associated with a lack of vitamins. The tongue may become enlarged and can easily become imprinted with teeth.
With candidal cheilitis, the inflammatory process is accompanied by the formation of white plaque on the mucous membranes. The cause of this disease is the proliferation of a fungus of the genus Candida; it often affects infants, people after radiation and chemotherapy, as well as patients with immunodeficiencies. Cheilitis develops with long-term use of antibiotics and immunosuppressants.
Vitamins
The appearance of a jam indicates not only the presence of some pathogen, but also the weakness of the skin, since any infection manifests itself in the weakest places.
This means there are problems with the skin and vitamins that are responsible for its condition help solve them. Namely: A, B2 and E. It is the presence of these vitamins that needs to be replenished in order to get rid of unpleasant and painful wounds. This can be done quickly with complex pharmaceutical preparations containing these vitamins.
Also, vitamin deficiency can be replenished from food, but this will last longer than with the use of the drug.
Diagnostic features
If inflammation appears on the lip, it is advisable to visit a therapist, for children a pediatrician, if indicated, an infectious disease specialist, a dentist, or other specialized specialists. Diagnosing cheilitis is usually not difficult - a specialist will conduct an examination, listen to complaints and prescribe a series of tests. If the allergic nature of the disease is suspected, allergy tests may be recommended, and if plaque appears, it is advisable to take a scraping. To detect endocrine and other disorders that may cause the disease, biochemical blood tests and other diagnostic methods are often prescribed. In rare cases, a biopsy is required to differentiate cheilitis from other pathologies. This will help to exclude the malignant or precancerous nature of inflammatory formations and prescribe the correct treatment.
Angulitis: clinical manifestations
The symptoms of angulitis are very similar to the manifestations of herpes, so it is extremely important to promptly contact a specialist who will make the correct diagnosis and tell you how to quickly cure angulitis.
Symptoms of seizure:
- redness in the corners of the mouth;
- cracks;
- multiple blisters with purulent contents;
- slight bleeding (not always);
- purulent crusts.
Treatment of lip jams in adults depends on the etiology and form (acute or chronic). It is very important to start treatment on time, because without it, the affected area can increase, causing significant discomfort to the patient.
Treatment methods
The treatment plan for cheilitis is developed individually, depending on the form of the disease, the severity of symptoms, and the characteristics of the health condition. Thus, in the treatment of the exfoliative form of the disease, the key element of effective treatment is the impact on the psycho-emotional sphere: you will need to contact a neurologist or psychoneurologist to prescribe sedatives and antidepressants according to indications. Consultation with an endocrinologist may be required.
Local treatment may involve the use of laser or ultrasound physiotherapy, local anti-inflammatory drugs, and less commonly, radiation therapy. Elimination of excessive dryness is possible with the help of hygienic lipsticks. To speed up recovery, the doctor may prescribe vitamin therapy, UVOC and other methods of maintaining the body's defenses.
Therapy for glandular cheilitis consists of using local anti-inflammatory agents. Antibacterial, antiviral, and hormonal ointments can be used. A radical method of therapy is electrocoagulation of the salivary glands or their surgical removal, as well as laser ablation. These methods are used when conservative methods are ineffective. After the main course, the doctor will prescribe medications to prevent relapses - they will eliminate dry or weeping skin. It is important to sanitize the oral cavity in a timely manner and undergo professional teeth cleaning.
Treatment of atopic cheilitis consists of eliminating irritating factors. Drugs with antipruritic and anti-inflammatory effects can be used locally, and therapy with antihistamines with a systemic effect is also carried out. The use of glucocorticosteroids allows you to get quick relief, but it is important to strictly adhere to medical prescriptions - they can only be used for a short time. It is important to follow a hypoallergenic diet and remove allergenic foods from the diet.
Therapy for meteorological cheilitis begins with limiting harmful effects, for example, insolation. Local treatment is usually carried out - the doctor prescribes hormonal agents and protective creams, including those with SPF. The course of treatment is supplemented with vitamins - vitamin-mineral complexes or individual preparations (B, PP, C, etc.).
In the treatment of macrocheilitis, immunocorrective and antiviral therapy is of particular importance. The doctor may prescribe:
- hormonal anti-inflammatory drugs of systemic action;
- novocaine blockades;
- antihistamines, etc.
Laser therapy can have a positive effect on the correction of the entire triad of symptoms. Other physical therapy methods have been successful in treating facial neuritis.
Seizures in the corners of the mouth: treatment with ointments
At home, when seizures occur, antiseptic, antibacterial, antifungal and combination ointments are used, depending on the pathogen. Antibacterial and antifungal agents are more effective than antiseptics, since they not only prevent the proliferation of microorganisms, but also contribute to their death. Good results can be achieved by combining solutions and ointments.
Below are the TOP 5 types of ointments for treating seizures at home:
| Name of ointment | Description |
Ointments with antiseptic effect:
Prescribed for the following cases: common and uncomplicated streptococcal and candidal infections. | Ointments can be applied to the corners of the lips and surrounding areas of the skin in a thin layer, but a better effect can be achieved with ointment compresses. To do this, the medicine is applied to a sterile napkin and fixed in the corners of the lips with an adhesive plaster overnight. Antibacterial ointments are ineffective against fungal infections; moreover, they can aggravate the course of candidiasis. Levomekol ointment is not suitable for treatment in the lip area. Oxolinic ointment and Acyclovir are ineffective against streptococcal and candidal infections. |
Antifungal agents (fungicides):
Prescribed for the following cases: candidal infections. | Antifungal ointments are used by applying them to the corners of the mouth in a thin layer or in the form of compresses 3-4 times a day. Fungicide solutions are used to treat not only the corners of the mouth, but also the entire oral cavity. This is necessary for the treatment or prevention of candidal stomatitis. Fungicides are ineffective against streptococcal infections. |
Antibacterial agents:
Prescribed in the following cases: streptococcal seizures | Ointments can be applied to the corners of the lips and surrounding areas of the skin in a thin layer, but a better effect can be achieved with ointment compresses. To do this, the medicine is applied to a sterile napkin and fixed in the corners of the lips with an adhesive plaster overnight. Antibacterial ointments are ineffective against fungal infections; moreover, they can aggravate the course of candidiasis. Levomekol ointment is not suitable for treatment in the lip area. Oxolinic ointment and Acyclovir are ineffective against streptococcal and candidal infections. |
Combined ointments:
Prescribed for the following cases: chronic seizures, seizures caused by a mixed infection, in the presence of concomitant atopic dermatitis in the area around the mouth. | Combined ointments contain an antibiotic, an antifungal component and a glucocorticosteroid hormone. These remedies can only be prescribed by a specialist when other treatment methods do not help. |
Remedies that promote rapid healing of a seizure:
Prescribed in such cases: all types of jam. | In order to quickly get rid of jams, in addition to antibacterial ointments and antiseptics, use ointments that promote wound healing. But you need to know that these ointments are not prescribed from the first day of therapy. They are connected to the main treatment when the first positive results appear: on the 2-4th day. Healing ointments are applied in a thin layer 3-4 times a day at least an hour after using antibacterial ointments. |
To read: Peritonitis
Usually, seizures do not require general treatment; they heal with the use of only local medications. But if the lesions have spread to large areas of the skin, do not heal for a long time and are associated with immunity problems, then the use of general remedies is necessary. They are prescribed only by a doctor.
Possible complications
Failure to see a doctor in a timely manner often causes serious complications. The disease itself often does not pose a serious health risk. But only an experienced specialist can tell you how to treat cheilitis. Self-medication can lead to unpleasant consequences and provoke the occurrence of a chronic form of the disease. In addition, cheilitis is dangerous because its symptoms can mask malignant tumor processes. It is important to remember that some forms are prone to malignancy - cheilitis may be followed by precancerous conditions.
Prognosis and prevention
With timely treatment and the absence of malignancy processes, the prognosis is almost always favorable. If the therapy has caused noticeable cosmetic defects, you can resort to methods for correcting the appearance of the lips.
To prevent complications, it is important to understand whether you are at risk. The presence of allergic diseases and dermatoses, chronic endocrine diseases, and wearing dentures increase the risk of developing pathology. To prevent the appearance of cheilitis, it is important to adhere to several rules:
- regularly visit the dentist, sanitize the oral cavity, remove tartar;
- promptly replace outdated fillings and orthopedic structures, contact after chipped teeth and injuries to prevent lip injury from the sharp edges of fillings and enamel;
- For the manufacture of prostheses, contact only professionals;
- eat properly and nutritiously to prevent hypovitaminosis;
- try to avoid prolonged exposure to the sun and use products with SPF, including for lips;
- be attentive to your health and promptly treat diseases of the gastrointestinal tract, endocrine, nervous system, and internal organs.
Types of angulite
Considering the etiology, seizures can be primary and secondary. In turn, the primary ones are divided into: streptococcal, viral and candidiasis.
Viral seizures. They are caused by a viral infection (herpes virus). In this case, a doctor will help you choose an ointment for sticking in the corners of an adult’s lips.
Streptococcal seizures are caused by streptococcal infection. A characteristic manifestation is the formation of a yellowish-red crust.
Candidiasis angulitis. The cause is a fungal infection. This type is characterized by a chronic course and the absence of a crust.