Errors and complications that arise when preparing and filling a carious cavity
Insufficient preparation (treatment) of the carious cavity
When preparing a carious cavity, it is necessary to carefully remove necrotic, pathologically altered dental tissues. Leaving areas of softened dentin subsequently leads to infection of the underlying areas and the development of secondary caries or inflammation of the pulp - pulpitis. Even if such unpleasant complications do not arise, the softened dentin absorbs pigments, its color changes, which leads to darkening of the tooth crown. When secondary caries occurs, the tooth tissue surrounding the filling is destroyed and it falls out. Incorrect formation of the cavity leads to fractures of the filling material or breaking off (of the enamel edge) of the walls of the carious cavity. Overhanging edges of the enamel create the preconditions for their breaking off and the occurrence of secondary caries.
Many errors can occur if the preparation regime is violated. These include: overheating and burns of hard tissues (especially dentin), overheating of the pulp (heating to 70° C causes its necrosis), etc.
Traumatic preparation leads to severe pain, and if anesthesia is used, to irritation and inflammation of the pulp. If there is strong pressure on the bur, in addition to damage to the hard tissues of the teeth, pulp or gums, even such a casuistic complication may occur as breakage of the bur and its jamming in the carious cavity being prepared. In general, careful adherence to the rules for preparing a carious cavity allows you to avoid a number of complications.
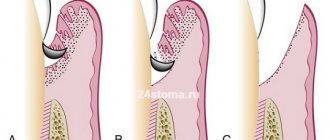
Perforation of the bottom of the carious cavity
Perforation of the bottom of a carious cavity occurs when careless or rough preparation of the bottom of a carious cavity with a bur or excavator. In the latter case, this often happens with acute deep caries, if when processing the bottom of the cavity they do not take into account that the distance between the tooth cavity (the pulp itself) and the carious cavity is very small (0.1-0.3 mm thickness of the septum). You need to be especially careful when preparing a carious cavity with a turbine drill. It is necessary to take into account the topography of the dental cavity and pulp horns, which are very easy to perforate when expanding and forming a carious cavity. When preparing its bottom, you should avoid using small-sized burs, especially fissure and reverse-cone ones. The prerequisite for perforations is an insufficiently opened carious cavity with overhanging edges, which make it difficult to examine, and the dentist does not see the position of the drill in the carious cavity.
When the bottom of a carious cavity is perforated, sharp pain occurs due to pulp trauma (when preparing a cavity under anesthesia, this symptom may not be expressed, which causes a certain feeling of carelessness in the doctor). A drop of blood or serous-bloody fluid appears at the site of perforation. Due to pulp perforation, acute traumatic pulpitis develops (accidental exposure or injury of the pulp). Pulp injury occurs when there is significant trauma to the coronal pulp with a drill or other instrument (excavator). Therefore, this complication is treated in the same way as acute traumatic pulpitis (antiseptic treatment of the carious cavity, use of pastes with calcium hydroxide, antibiotics, enzymes, etc.). Treatment tactics depend on the degree of damage to the pulp: in case of accidental exposure, conservative (biological method) treatment is carried out, and in case of accidental injury to the pulp - amputation or extirpation depending on the degree of injury, location of the tooth (incisor or molar), location of the carious cavity on the crown of the tooth, the patient's age and other factors. Recently, there have been reports of successful treatment of accidental pulp exposure by covering it with light-curing calcium hydroxide pastes, then treating the perforation with an adhesive system and covering it with a composite material (compomer).
Perforation of the wall of the carious cavity
Perforation of the wall of the carious cavity occurs due to traumatic preparation and incorrect assessment of the relationship between the carious cavity and the crown or the general axis of the tooth.
Most often this is observed near the neck of the tooth on the contact surfaces. In this case, the gums are usually injured, which is accompanied by pain and minor bleeding. It is necessary to carefully examine the perforation site to avoid mistakes. Sometimes pulp perforation is diagnosed and appropriate “treatment” is carried out, for example, a devitalizing paste is applied. Usually, when the wall is perforated, bleeding from the gum wound is stopped with cotton balls soaked in a solution of hydrogen peroxide or other hemostatic agents. The perforated hole is carefully prepared according to the rules for preparing a carious cavity and filled with filling material when filling a carious cavity. The use of glass ionomer cements and compomers in such cases is very effective.
Breaking off the wall of a carious cavity can occur due to rough lever-like movements of an excavator or drill, when excessive pressure occurs on one of its walls.
You need to be especially careful when preparing thin walls of a cavity with overhanging edges, which very easily break off even with slight pressure on them with the bur of a turbine drill. In these cases, one must remember about the very high speed of rotation of the turbine, when even a slight force of the operator’s hand (20-30 g) applied to the tip causes significant pressure of the bur on the wall of the carious cavity. In such cases, it is recommended to perform necrectomy of softened dentin very carefully, with relatively low bur rotations. To eliminate the defect formed after breaking off the wall of the carious cavity, the carious cavity is formed accordingly (usually with a ledge or an additional cavity or platform) and filled. Significant defects in the tooth crown are restored by restoring it with composite materials or artificial crowns.
Bur damage to adjacent teeth
Damage to neighboring teeth by the bur can occur when preparing carious cavities located on the contact surfaces of the teeth, in cases where the rules for removing the carious cavity to the chewing (palatal) surface are neglected. The degree of damage to the hard tissues of the adjacent (adjacent to the cavity) tooth can vary - from a slight defect in the surface layer of enamel to its complete absence. Minor enamel defects are treated with fluoride varnish or other fluoride-containing (remineralizing) preparations. A very good effect is achieved when covering such damage with light-curing adhesive systems of composite materials.
A special sealant is offered for this purpose - “Seal & Protect”. If there is an enamel defect with a violation of the enamel-dentin junction, it is closed with an appropriate filling material (with preparation of the defect or when using composites without significant preparation of the hard tissues of the affected adjacent tooth).
Damage to the gingival margin
Damage to the gingival margin occurs during the preparation of carious cavities located on the contact surfaces and in the cervical area of the teeth. In this case, pain in the gums and bleeding from it are noted. Bleeding is stopped with cotton balls soaked in a 3% solution of hydrogen peroxide or another hemostatic agent. After this, the treated carious cavity is thoroughly washed, dried and filled. To prevent this complication, you need to carefully prepare the carious cavity, avoiding injury to the gums. The gingival papilla, which grows into the carious cavity, must first be forced out of it or removed (surgically, with a diathermocoagulator or using cryodestruction).
A number of errors and complications occur during filling a carious cavity.
When filling, it is important to choose the right filling material and prepare it. The wrong choice of material leads to cosmetic defects, causes rapid destruction and loss of the filling due to the discrepancy between the strength of the material and the chewing pressure. When preparing filling material and filling a carious cavity with it, you must carefully follow the manufacturer's instructions. Neglect of these rules sharply reduces the physical and mechanical properties and strength of the filling, contributes to its rapid destruction, discoloration and the occurrence of other complications.
Incorrect application of the insulating gasket
Improper application of a sealing lining for moderate to deep caries can cause irritation or damage to the pulp by chemical, toxic or thermal irritants from permanent filling materials. The presence of a gasket on the side walls of the carious cavity (above the enamel-dentin junction) worsens the marginal fit and fixation of the permanent filling material, predisposing to the occurrence of secondary caries and loss of the filling. Placing a gasket on the vestibular wall of a carious cavity in the frontal teeth leads to a cosmetic defect. An opaque pad in the form of a yellow spot shines through the translucent enamel of the vestibular wall. The use of adhesive systems of the fourth and fifth generations greatly facilitates the work of the dentist, since it requires a minimum size of the isolating pad, however, in many cases it is necessary.
Overbite when filling a carious cavity
Overbite when filling a carious cavity causes pain or a feeling of awkwardness when chewing, and can limit the movements of the lower jaw. Constant overload of a filled tooth can lead to chronic periodontal injury - the development of acute or chronic periodontitis. In some cases, this may be preceded by inflammation of the pulp with severe pain. Such fillings sometimes break easily under the influence of pressure, which can lead to breaking off the walls of the carious cavity or splitting the tooth crown (especially in premolars). To prevent such complications, it is necessary to very carefully fit the filling in contact with the antagonist teeth.
No contact point
The absence of a contact point creates conditions for the accumulation of food debris between these teeth, which injure the interdental papilla, promote the development of caries on the contact surfaces of the teeth, as well as periodontal diseases (papillitis, gingivitis, periodontitis). Only in some cases, for example, when there are wide gaps between teeth, a contact point is not created during filling.
Application of a single filling in adjacent carious cavities
The application of a single filling in adjacent carious cavities disrupts the natural microexcursions of the teeth. This leads to loosening of the filling, its breaking and falling out. In addition, such a filling dramatically violates the conditions for self-cleaning of the interdental space, which can lead to secondary caries and periodontal diseases.
Overhanging edges of the filling
The overhanging edges of the filling, which protrude into the interdental space, injure the gums and create conditions for the accumulation of food debris between the teeth (Fig. 182). This leads to complications (secondary caries, inflammatory periodontal diseases). To prevent complications that may arise when filling a carious cavity, you must carefully follow all the rules for filling a carious cavity with filling material and use the matrix when filling carious cavities on contact surfaces.
Incorrect selection and preparation of filling material
Incorrect selection and preparation of filling material often leads to immediate complications. It must be remembered that any violation of the technology for preparing the filling material and the filling technique causes a sharp deterioration in the quality of the filling. The choice of material is determined by the clinical situation, and deviation towards aesthetics at the expense of strength, or vice versa, subsequently leads to the destruction of the filling or a violation of the cosmetic effect of the filling.
Antibacterial treatment of carious cavities
Comparison of the antibacterial effectiveness of 2% chlorhexidine and diode laser radiation with a wavelength of 810 nm at the stage of preparing a carious cavity for filling
| G.B. Lyubomirsky Candidate of Medical Sciences, Assistant at the Department of Therapeutic Dentistry, Izhevsk State Medical Academy Ministry of Health of Russia, dentist-therapist Address: 426034, Udmurt Republic, Izhevsk, st. Kommunarov 281 Tel. |
Summary. The issue of achieving “sterility” of a carious cavity before filling is a pressing issue in modern therapeutic dentistry. One of the reasons for the formation of secondary and recurrent caries is considered to be inadequate antiseptic treatment of the carious cavity. Poor-quality antiseptic treatment leads to the emergence of alternative means for medicinal treatment of dental caries, therefore leading manufacturing companies regularly develop and introduce to the dental market various means and methods that allow achieving “sterility”; The laser industry is no exception to this work.
Key words: dentin caries, sterilization of carious cavity, diode laser, antibacterial effectiveness.
Comparison of antibacterial efficacy of 2% chlorhexidine and diode laser with a wavelength of 810nm at the stage of cavity to sealing (GBLubomirskiy).
Summary. The question of achieving “sterility” before filling the cavity, a key issue for modern odontology. One of the reasons for the formation of secondary and recurrent caries is considered to be defective antiseptic processing. Substandard antiseptic treatment leads to the development of alternative means for medical treatment of a tooth cavity, therefore leading manufacturers regularly develop and submit to
the dental market a variety of means and methods allowing to achieve a “sterile”, not the exception in this work is and laser industry.
Keywords: dental caries, dentin sterilization cavity, diode laser, antibacterial efficacy.
Introduction
An analysis of most studies shows that the “sterility” of a carious cavity before filling is one of the important elements of the successful work of a dentist.
The problem of the occurrence of recurrent and secondary caries is one of the pressing problems of therapeutic dentistry [1, 2]. Leading manufacturing companies in their laboratories annually
invent new means and techniques for complete medicinal treatment of hard dental tissues.
Drug treatment, as one of the key stages in the treatment of dental caries, has the following goals: cleansing the carious cavity, bactericidal effect on the cavity and drying it out. Previously, a solution of 3% hydrogen peroxide and medical alcohol were used for this, and medical ether was used for drying. For deeper cavities, a special solution was prepared, consisting of 1% hydrogen peroxide, 1% chloramine solution, 0.1% furatsilin solution, and the drying process was carried out with warm air. However, the appearance of light-polymer composite materials at dental appointments led to a change in the medical treatment of carious cavities. Thus, a number of authors claim [11,12] that alcohol and ether are not effective for drying, since it has been found that they are relatively toxic and do not fully dry the carious cavity, and 3% hydrogen peroxide reduces the adhesive properties of composite materials and destroys the so-called polymer matrix. Dentists have recognized that the effectiveness of cavity treatment with such methods is far from high, and is also technologically complex. The drugs used are not very pleasant in taste and smell for the patient, and the “safety” of hydrogen peroxide and sodium hypochlorite for future fillings is questionable. Therefore, a number of authors consider it advisable to antiseptically treat the carious cavity with a 2% aqueous solution of chlorhexidine [8].
Poor quality antiseptic treatment of carious cavities has led to the emergence of alternative means for antiseptic treatment, which, according to the authors [7], do not cause sensitization of the body and the development of an allergic reaction, thereby simultaneously reducing their effectiveness. TO
These remedies include herbal remedies: calendula tincture, romazulan. Calendula tincture has a bactericidal effect on coccal microflora, has a pronounced anti-inflammatory,
epithelializing and reparative actions, but less effective against St. mutans, which is one of the microorganisms that leads to the development of caries [4].
Romazulan has a pronounced antiseptic and antimicrobial effect, but in addition to chamomile extract, it contains essential oils, which cannot be used for further fillings
cavities with light composite materials [3].
Ozone treatment of a carious cavity is one of the modern methods used in the treatment of dental caries [5, 6]. Liquids are enriched with ozone in ozonizers or exposed to ozone-air
mixture produced in ozone generators. Proven to be powerful antimicrobial
action potential and strong oxidizing ability of ozone, which suggests its use in reducing the number of cariogenic microorganisms and beneficially suppressing organic acids in
affected areas. Perhaps the stereotype of ozone toxicity or the high cost of equipment do not contribute to the widespread use of these methods in the practice of dentists in Russia.
Based on the modern dental market and the realities of the work of dentists, an obviously urgent task was to consider one of the hardware methods of antiseptic treatment of a carious cavity, which includes diode laser radiation. Today, photodynamic therapy techniques are known using special solutions [9,10], which are used with diode lasers, including those with a wavelength of 810 nm. In our study, we did not use chemical compounds for PDT, which, it should be noted, are rare and are not cheap.
noah, but used in isolation only the bactericidal properties of the laser beam itself (810 nm) declared by the manufacturer.
The purpose of our work was to study the bactericidal properties of diode radiation
laser with a wavelength of 810 nm in comparison with traditional medicinal treatment of carious cavities before filling teeth.
Materials and methods
In total, the study involved 65 people (25 men and 40 women) aged from 20 to 60 years with dentin caries, who were treated with 132 chewing teeth of the upper and lower jaws.
Carious cavities were localized on the occlusal surface of the tooth. At the time of treatment, the patients were without severe somatic pathology. The scope of interventions was determined according to the plan of a comprehensive clinical trial. Dynamic observation was carried out after 1, 3, 6, 12
months. All patients were divided into 2 groups according to the type of drug treatment
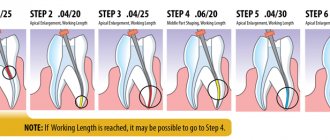
carious cavity before the final stage of filling. Patients of both groups, before treating dentin caries, underwent professional hygiene using a combined method. The first group included 32 people (66 teeth), from whom, before treating the carious cavity, material was taken with sterile cotton swabs (adapted in size to the carious cavity ) from the bottom and walls of a carious cavity formed and ready for filling
Next, the seeds were inoculated with a “lawn” on a solid nutrient medium in a Petri dish (blood agar) (Fig. 2). After this, drug treatment was carried out with 2%
chlorhexidine. Having completed the antiseptic effect on the carious cavity, the stage of collecting material from the bottom and walls of the carious cavity and inoculating it on a nutrient medium was repeated. According to the treatment plan, the stage of filling with light composite materials was implemented.
The second group included 33 people (66 teeth), who, before treating the carious cavity, collected material with sterile cotton swabs (adapted in size to the carious cavity) from the bottom and walls of the carious cavity formed and ready for filling. Next, the seeds were inoculated with a “lawn” on a solid nutrient medium in a Petri dish (blood agar). Afterwards, the stage of “sterilization” of the carious cavity was carried out using diode laser radiation with a wavelength of 810 nm
Picasso Lite (AMD Lasers USA). Laser treatment was carried out in constant mode using a replaceable optical fiber (400 μm in diameter) for 60 seconds. at a power of 0.6 W. It was carried out for 45 seconds. according to the non-contact-labile method - with movements of the “painting brush”, “painting” the bottom and walls of the carious cavity, after - 15 seconds. using the contact-labile method, pointwise touching and scratching the surface of the carious cavity with an optical fiber (Fig. 3). Having completed the antiseptic effect on the carious cavity, the stage of collecting material from the bottom and walls of the carious cavity and inoculating it on a nutrient medium was repeated. According to the treatment plan, the stage of filling with light composite materials was implemented.
Upon completion of the clinical stage in the laboratory, the Petri dish was left in a thermostat for 24 hours at a temperature of 37C.
After incubation, if bacteria grew, they were divided into colonies. Identification of isolated bacterial cultures was carried out by studying the morphology of bacteria, their cultural, biochemical and other characteristics inherent in each species.
Before treatment, all patients signed informed consent for the study.
Statistical processing was carried out using the Stat Soft Statistika ver.6.0 program.
Results and discussion
Analysis of the study results showed that the procedure for laser “sterilization” of a carious cavity does not cause discomfort in patients. As a result of dynamic observation for 12 months, in patients of group 1, clinical well-being associated with the absence of recurrent caries on the treated teeth participating in the study was observed in 100% of cases, in group 2 - 100% (p>0.05); the absence of secondary caries in the first observation group corresponds to 97%, in the second group - 98% (p>0.05). In both groups, we associate the low percentage of secondary caries - 2% and 3% - with poor oral hygiene of patients carried out at home.
During the laboratory stage of the study, it was revealed that before antiseptic treatment of the carious cavity, both small and large colonies are sown. Of the total number of colonies in the first group, small ones are found in 93.2%, large ones - 6.8%, in the second group - 81% and 19%, respectively. During microscopy (light microscope, eyepiece - 10, objective - 90, magnification - 900
times) colonies were detected: Streptococcus mutans, Streptococcus mitis, Streptococcus salivarius, Staphylococcus epidermidis, Lactobacillus, diplococcus (Fig. 4).
After antiseptic treatment of the carious cavity in the first group, a decrease in the number of small colonies was observed by 77%, large colonies by 12.5%. In the second group of the study, where diode laser exposure was used before filling, a decrease in the number of small colonies was noted by 81%, large colonies by 100%. Those. the number of colonies in the first group decreases by 2.2 times, and in the second
study group - 5.5 times. Thus, by following all the principles, stages and techniques of carious cavity preparation, using means of complete retraction and isolation of the working field, and also by abandoning weak antiseptic solutions, we can achieve high clinical results in the treatment of hard dental tissues and significantly reduce the percentage of predicted complications. Using a diode laser with a wavelength of 810 nm in the process of treating a carious cavity, we provide a full bactericidal effect on all surfaces of the carious cavity. An “innovative” approach to the search for methods to achieve sterility of a carious cavity does not exclude issues of synergy in the use of liquid antiseptics in combination with laser radiation. In this case, the combination is justified, but the dentist needs to remember the properties of laser radiation and use the laser at the final stage of treatment, when the carious cavity is dry and prepared for filling.
Literature:
1. Borovsky E.V. Therapeutic dentistry. - M.: Medicine, 1998. - P. 562.
2. Buyankina R.G. Assessing the quality of filling carious cavities and improving the diagnosis of recurrent caries: Abstract of thesis. dis. Ph.D. honey. Sciences / R.G. Buyankina. - Omsk, 1987. - 20 p.
3. Ivanov V.S., Ovrutsky G.D., Gemonov V.V. Practical endodontics. — M.: Medicine. — 224 p.
4. Kuryakina N.V., Alekseeva O.A., Tretyakova T.A., Makarova V.G. Medicinal plants and products
beekeeping, used in dentistry. - M.: Medical book; N. Novgorod: NGMA, 2000. - 282 p.
5. Maslennikov O.V., Kontorschikova K.N. Practical ozone therapy. Benefit. - N. Novgorod: Publishing house “Vector-TiS”, 2003. - 52 p.
6. Bezrukova I.V., Petrukhina N.B. Ozone therapy in periodontal practice. — M.: Medical
information agency, 2008. - 88 p.
7. Marchenko A.I., Baranyuk A.I., Levitskaya E.V., Sokolovskaya E.P. Medicinal plants in
dentistry. - Chisinau: Shtiintsa, 1989. - P.167.
8. Ruvinskaya G.R. Clinical aspects of modern means and methods of intracarnial medicine
in endodontics / G.R.Ruvinskaya, Yu.V.Fazylova, D.A.Yavgildina // Practical medicine. — 2009.
- No. 1. — P. 18-23.
9. Furtsev T.V., Lipetskaya E.A., Kolenchukova O.A. Comparison of the effectiveness of the drug “Consepsis” and the method of photodynamic therapy for antibacterial treatment of cavities in the treatment of deep caries // Russian Dental Journal. - 2012. - No. 6. — P. 15-18.
10. Yusupov A.S. Study of the effectiveness and safety of epigallocatechin-3-gallate (Egallohit gel) during laser resurfacing of skin scars // Bulletin of Dermatology and Venereology. - 2009. - No. 1. - P. 1-4.
11. Aasen SM Bonding systems: A comparison of maleic and phosphoric acids / SMAasen, PDArio // J.Dent.
Res. 1993. - Vol. 72. - P. 137.
12. AI-Negrish AR Composite resin restorations: a crosssectional survey of placement and replacement in
Jordan / ARAl-Negrish // Int. Dent. J. 2002. - Vol. 52. - No. 6. — P. 461-468.
Errors and complications that arise after caries treatment
Pulp inflammation and necrosis
A number of complications can occur at different times (several months or years) after treatment. Inflammation and necrosis of the pulp are quite common. The causes of this complication may be traumatic preparation of the carious cavity, which causes overheating of the pulp and excessive pressure on the bottom of the carious cavity. The occurrence of inflammation in the pulp is facilitated by treating the cavity with toxic or irritating (for example, ethyl alcohol) medications, as well as vigorous drying of the carious cavity with a stream of cold air. Permanent filling materials can irritate the pulp due to toxic (cements, plastics, composite materials) or thermal (amalgam) effects, which manifests itself in the absence or incorrectly applied insulating lining. Some medications that are used to treat acute deep caries can also have a toxic effect on the pulp.
Depending on the strength of the irritating factor, pulp inflammation can occur in the form of various forms of acute or chronic pulpitis with a corresponding clinical picture. Pulp necrosis develops, as a rule, almost asymptomatically and may first appear as a change in the color of the tooth crown (it becomes gray or dark gray). Treatment is carried out according to the rules for the treatment of pulpitis. To prevent such complications, it is necessary to correctly and carefully follow all the rules for preparing and filling a carious cavity.
Secondary caries
Secondary caries can occur due to insufficient preparation of the carious cavity, when areas of demineralized dentin remain on the walls and bottom of the cavity. Insufficient or improper treatment of the enamel edges of the cavity leads to disruption of the marginal seal of the filling, the formation of a gap and, subsequently, caries. The causes of secondary caries can be the irrational shape of the carious cavity, improper application of an insulating lining, moisture entering the cavity during filling, and improper preparation of the filling material. The lack of general treatment of caries (according to indications) can also cause the development of a carious process around cavities filled (even with the best materials).
When secondary caries appears, the remaining fillings are removed, the carious cavity is prepared and filled according to the depth, location and course of the caries.
Papillitis, or inflammation of the interdental gingival papilla
Papillitis, or inflammation of the interdental gingival papilla, occurs when there are defects in filling carious cavities on the contact surfaces of teeth, overhanging edges of fillings, the presence of a single filling in two adjacent cavities, injury to the gums during preparation and filling (for example, with a matrix, instruments) of a carious cavity.
If there is inflammation of the gingival papilla, defective fillings are replaced first, avoiding injury to the gums. Then, if necessary, drug treatment is carried out depending on the type of papillitis. Treatment of papillitis should not be neglected, since chronic trauma to the gums can lead to more severe periodontal damage, such as localized periodontitis.
Acute and chronic apical periodontitis
Acute and chronic apical periodontitis usually develops a few days (acute) or months (chronic) after caries treatment. They may be a consequence of the same reasons that cause inflammation and necrosis of the pulp, and are a continuation of the development of this pathological process. A common cause of periodontitis is chronic overload of the tooth due to increased occlusion with a filling. Treatment of acute and chronic periodontitis requires endodontic procedures.
Changing the color of the tooth crown
A change in the color of the tooth crown (to gray, dark gray) may be a consequence of insufficient preparation and removal of necrotic dentin, pulp necrosis and chronic periodontitis. Darkening of the crown of a tooth can occur after filling teeth with amalgam, especially if it is not carefully prepared. To eliminate areas of pigmented, necrotic dentin, the filling is removed, a thorough necrectomy is performed, and the cavity is filled again with an appropriate filling material. Pulp necrosis and chronic periodontitis require endodontic treatment.
Excoriation of gum areas
Excoriation of areas of the gums that are adjacent to the filling in the cervical area may be a consequence of the body’s increased sensitivity to the material from which the filling is made. This is most often observed in cases where the filling is made of plastic or composite materials (allergic reaction). The cause of excoriation may be a poorly made filling with an unpolished, rough surface. To eliminate such a complication in the case of “contact allergy,” it is necessary to replace the filling with a new one made of inert (non-allergenic) material for the patient’s body. If there is a rough surface of the filling, it is enough to carefully process and polish it.
Displacement, fractures and loss of fillings
Displacement, fractures and loss of fillings most often occur due to violations of the rules for preparing filling material and the formation of a carious cavity. This is especially true for class II cavities, when the shape and size of the auxiliary (additional) cavity do not correspond to the dimensions of the main cavity, a ledge is not formed or it is given an irregular shape. If the spacer and filling material are unevenly distributed along the bottom and walls of the carious cavity, splitting and fracture of the filling material may occur in the place of the smallest thickness of the filling (Fig. 184). The reasons for a filling falling out may be the wrong choice and violation of the rules for preparing the filling material and the filling technique itself, or insufficient isolation of the filling from saliva.
The color of the filling does not match the color of the tooth enamel
The discrepancy between the color of the filling and the color of the tooth enamel most often worries the patient if it is detected on the front teeth and premolars. Sometimes this complication occurs even if the original color of the filling material and enamel match, if the technology for preparing the material and filling is violated. As a result, the filling changes color after some time (usually becomes yellow, yellow-gray). It can absorb food pigments, etc. Fulfillment of the entire complex of requirements for the technology of preparation of filling material and filling allows one to avoid this complication. In some cases, to remove the darkened layer of the filling, it is enough to sand its surface. If this does not give the desired result, then the filling is replaced with another one made of the corresponding color of material.
Ineffective drug treatment of initial caries can be considered a complication or error. This may be a consequence of the wrong choice of tactics, medications, methods of their use and duration of treatment. Sometimes this condition worsens due to the lack of appropriate general sanitation. A carious cavity appears, which requires surgical treatment (preparation and filling).