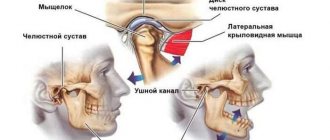
Pain in the jaw when opening the mouth, localized anterior to the ear canal (anterior to the ear) is one of the main signs of problems with the temporomandibular joint (see “TMJ dysfunction”), which provides a mobile connection between the lower jaw and the skull.
Pain in the jaw joint can have varying degrees of severity, intensify when opening and closing the mouth, and be accompanied by difficulty and sometimes impossibility of opening the mouth. May be accompanied by various “noise effects” in the joint area: clicking (see “Clicks when opening the mouth”), grinding, creaking (see “Crunching when opening the mouth”). And also tinnitus. But all these signs, if left unattended, can soon have quite unpleasant consequences for the patient.
During a direct examination by a specialist, you will be able to find out your exact diagnosis, as well as receive a referral for diagnosis or a treatment plan.
Why does pain occur in the lower jaw?
Purulent diseases
The cause of pain is inflammation of the bone, periosteum or nearby soft tissue. In 70-80% of cases the disease is of odontogenic origin. Less commonly, the process is provoked by acute infections and jaw injuries. Complemented by edema, hyperemia, general condition disorder, intoxication syndrome, regional lymphadenitis. Pain is observed in the following pathologies:
- Periostitis.
The symptom is more pronounced in acute purulent periostitis. The pain is sharp, pressing or boring, radiating to the eye, ear, temple, neck. Intensifies when opening the mouth. Weakness, low-grade fever, and swelling of the cheeks are noted. In chronic periostitis, the pain is periodic, moderate or mild, pressing or bursting. The contours of the face are slightly changed. - Osteomyelitis.
Characterized by a sudden manifestation with a rapid rise in temperature to febrile levels, chills, and severe intoxication. The pain is shooting, pulsating, diffuse, radiating to the neck and half of the face. They get worse when swallowing, limiting mouth opening. The teeth are mobile, pus is released from the gums. The oral mucosa and skin of the chin become numb. In chronic osteomyelitis, the symptom increases after closure of the fistula, decreases or disappears after the outflow of pus resumes. - Perimaxillary abscess.
The formation of an abscess is preceded by toothache. Then dense swelling occurs. The pain quickly intensifies, and the symptoms of intoxication increase. The patient refuses food. After spontaneous opening, the manifestations disappear; in the absence of treatment, chronicity with periodic exacerbations, resumption of pain and suppuration is more often observed. - Perimaxillary phlegmon.
Typically acute onset with rapid progression of local manifestations, purulent-resorptive fever. The pain is jerking, aggravated by talking, chewing, and moving the lower jaw, and is complemented by increased salivation and the formation of a diffuse infiltrate with a fluctuation zone. The condition continues to deteriorate due to severe intoxication.
Traumatic injuries
Injuries to the lower jaw most often result from fights. Damage due to falls, car accidents, or industrial accidents is possible. In case of a bruise, the asymmetry of the face is caused by swelling of the soft tissues; the closure of the teeth is normal. The symptom is moderate, quickly decreases, and does not create serious obstacles to articulation or food intake.
Among the fractures, injuries to the body predominate; violations of the integrity of the angle and branches are less common. Half of the fractures are bilateral. At the time of injury, a sharp explosive pain occurs, decreasing only slightly over time, intensifying when talking, biting, or chewing. Possible numbness of the chin and lower lip. Facial asymmetry, articulation disorders, stepped dentition, mobility, and sometimes tooth dislocations are noted.
Fractures of the alveolar process of the lower jaw are less common than the upper jaw; they develop from impacts, falls from a height, etc. They are accompanied by intense spontaneous pain, which intensifies when swallowing or attempting to close teeth. The mouth is half-open, and the protruding edge of a bone fragment can be seen under the mucosa. The bite is broken, the teeth are mobile, dislocations are possible.
Pain in the lower jaw
Neuralgia
The symptom is accompanied by trigeminal neuralgia involving the 3rd branch (n.mandibularis). It is provoked by external factors (shaving, cold air, water), stress on the masticatory muscles. Prosopalgia is paroxysmal in nature and is a series of pain impulses that are felt like a lumbago or electric shock from the side of the face along the lower jaw to the chin. The pain is sudden, lasts several minutes, reaches such intensity that the patient freezes, does not move, does not speak.
With neuralgia of the glossopharyngeal nerve, the pain impulse is caused by chewing, swallowing, talking, lasts from several seconds to 3 minutes, occurs at the root of the tongue, spreads through the tonsils, palate, pharynx, ear. Radiating pain in the lower jaw. In patients with ganglionitis of the submandibular node, the pain is paroxysmal, burning, boring, pulsating. Lasts from 1 minute to 1 hour. They begin in the tongue, spread to the lower jaw, temple, back of the head, neck, and shoulder girdle.
Muscle damage
Bruxism is formed due to spasm of the masticatory muscles. After night attacks, patients are bothered by pain in the jaws, caused by clenching and intense movements relative to each other. Muscle pain, dental pain, headaches, dizziness, and drowsiness are possible. With myofascial syndrome, pain develops due to overload of the masticatory muscles. It is perceived as moderately expressed and deep. At first it appears only under load (chewing, clenching the jaws), then it increases and becomes constant.
Dental reasons
The symptom is disturbing in the first days after tooth extraction. It is especially pronounced in the presence of an inflammatory process, removal of impacted or incorrectly erupted wisdom teeth. Some patients report pain due to wearing braces and dentures. Aching, pressing or pulling pain in the jaw and masticatory muscles, problems with chewing and swallowing, biting the cheeks and tongue are detected in children with malocclusion.
The cause of severe progressive paroxysmal pain, which spreads to the entire lower jaw and intensifies at night, is acute diffuse pulpitis. Prolonged intense pain under the influence of external stimuli, spontaneously occurring pain attacks are also observed during the period of exacerbation of chronic pulpitis. Irradiation along the trigeminal nerve is typical. Between attacks, moderate or minor aching pain is possible, aggravated by biting.
Tumors of the lower jaw
Pain syndrome is characteristic of a number of odontogenic and non-odontogenic benign neoplasms. Distinctive features of such neoplasias are slow growth and lack of germination of surrounding tissues:
- Odontogenic fibroma.
More often diagnosed in children. The pain is aching, not intense, and does not occur in all patients. It can be combined with tooth retention and inflammation in the affected area. - Cementoma.
As a rule, it is localized in the area of molars or premolars of the lower jaw. The course is asymptomatic or with minor pain that increases with palpation. - Osteoma.
Accompanied by pain, facial asymmetry, slowly increasing over months or years. Large tumors limit the mobility of the lower jaw. - Osteoid osteoma.
Unlike other neoplasms, the pain is sharp, intense, intensifying at night and when eating. The face is asymmetrical, in the oral cavity there is a bulge in the area of premolars or molars. - Osteoblastoclastoma.
More common in adolescence and young adulthood. Facial asymmetry, tooth mobility, aching, bursting pain gradually progress. Over time, fistulas form over the neoplasia. Pathological fractures are likely.
Malignant neoplasms of the lower jaw are found less frequently than benign ones. Cancer is characterized by a rapid increase in pain, radiating to the cheek, ear, eye, and temporal region. Accompanied by mobility, tooth loss, germination of masticatory muscles, salivary glands, and ulceration. Osteogenic sarcomas rapidly progress and quickly infiltrate soft tissues. Over the course of several months, the pain increases from moderate, pressing, aching or bursting to constant, unbearable, and can only be eliminated with narcotic analgesics.
Cardiac ischemia
Irradiation into the lower jaw can be observed with angina pectoris and myocardial infarction. Painful sensations are caused by the spread of impulses from the heart to the upper thoracic segments of the spinal cord, from there, along other nerves - to the face, neck, left arm, left shoulder blade. The main symptom is burning, pressing, squeezing or bursting pain behind the sternum.
An attack of angina lasts several minutes and is eliminated after stopping physical activity and taking nitroglycerin. During a heart attack, the pain is wave-like, very intense, lasts more than 30 minutes, and does not disappear when using the methods listed above. In the atypical course of a heart attack and coronary artery disease, retrosternal pain may be absent, only reflected pain is observed, including in the jaw.
Prevention methods
Timely prevention is the key to good health at any age. It is important to form the right habits that will have a positive effect on the health of the heart and blood vessels, teeth and other organs. Doctors recommend:
- eat right, get enough vitamins and microelements;
- give up bad habits - smoking and drinking alcohol affect the condition of blood vessels;
- normalize your daily routine and devote enough time to rest;
- carry out moderate physical activity to train the heart muscle.
At the Clinical Brain Institute you can undergo an accurate and high-quality diagnosis of headaches and pain in the face. There is modern equipment here that can be used to determine the causes of pain. Doctors will also select an effective treatment regimen for use at home or in the hospital of our center.
Diagnostics
Diagnostic measures are carried out by a dentist or maxillofacial surgeon. According to indications, a neurologist, cardiologist, and other specialists are involved in the examination. The doctor determines the nature of the symptom, its changes since its onset, and its dependence on external factors. Identifies other complaints, conducts a general and dental examination to detect objective changes (hyperemia, edema, decayed teeth, asymmetry). To make a final diagnosis, data from studies such as:
- Radiography
. Informative for injuries, purulent processes (except for the acute stage), tumors, and some dental pathologies. Helps confirm the presence of a fracture, identify other bone changes, differentiate osteomyelitis and periostitis from inflammation of the surrounding soft tissues, distinguish between benign and malignant neoplasms. - CT scan
. CT scanning of the jaw provides more accurate data on the condition of hard structures compared to radiography. It is carried out when the diagnostic value of x-rays is insufficient, there is a need to clarify the location of fistulas, the nature of injuries and neoplasia. A CT scan of the skull makes it possible to determine the narrowing of the foramina, which causes compression of the nerve with the development of neuralgia. - Magnetic resonance imaging.
Recommended to exclude tumor and vascular origin of compression of the nerve trunk. Detects cysts, neoplasia, aneurysms, and tortuosity of vessels passing next to the nerve. - Electrophysiological studies
. Electromyography allows you to confirm pathological muscle activity during myofascial pain, bruxism, and assess the quality of neuromuscular transmission during neuralgia. Electroneurography makes it possible to determine the extent and level of nerve damage. An ECG is indicated for patients with suspected ischemic heart disease. - Invasive techniques
. A lymph node biopsy is performed when the submandibular or cervical lymph nodes are enlarged in patients with tumors. For perimaxillary phlegmon with a deep location of the purulent focus, a diagnostic puncture may be required to verify the diagnosis. - Lab tests
. The causative agent of purulent processes is determined by inoculating the discharge on nutrient media. For neoplasms, a morphological study is performed to determine the type and degree of malignancy of neoplasia.
Consultation with an oral and maxillofacial surgeon
Dental pathologies
Inflammatory processes in the oral cavity, wisdom teeth caries, and pulpitis can make it painful to open your mouth. Not every dental pathology manifests itself with such symptoms.
The occurrence of painful sensations
Today, there are many different techniques to cope with caries, pulpitis and stomatitis.
The pain is due to the fact that the inflammatory process involves soft tissues located near the temporomandibular joint on the left or right.
For example, with inflammation of the hood of a wisdom tooth or pulpitis in the molars (back teeth, designated numbers 6 and 7 in dental practice).
Nature of pain and accompanying symptoms
The main localization of pain is the affected tooth or mucous membrane; when opening the mouth, talking and eating, the discomfort spreads to the lower jaw joint. Bad breath often occurs.
Treatment methods
Sick teeth should be treated in a dental office. Today, there are many different techniques to cope with caries, pulpitis and stomatitis. Most often, they resort to removing the affected part of the tooth and placing a filling.
Treatment
Conservative therapy
Therapeutic tactics are determined by the cause of the symptom. For patients with dental pathologies, local treatment is indicated. Removable dentures and orthopedic structures are replaced, and other types of prosthetics are selected. In case of pulpitis, the cavity is treated with antiseptics, antibiotics, proteolytic enzymes, pastes are applied to eliminate inflammation and stimulate regeneration, and after a few days a filling is performed. For other diseases, the following methods are recommended:
- Inflammatory processes
. Antibiotic therapy is carried out in the pre- and postoperative period. At the initial stage, broad-spectrum drugs are administered parenterally. After receiving culture results, the medication is changed taking into account antibiotic sensitivity. Dressings are performed and rinsing is performed. Analgesics are prescribed to reduce pain. - Traumatic injuries
. In case of fractures of the angle, the body of the lower jaw without displacement, conservative immobilization is carried out by double-jaw wire splinting. To prevent inflammation, antibacterial agents are used, and painkillers are used to reduce pain. - Neuralgia
. Anticonvulsants are used to eliminate pain attacks. To enhance the effect, the treatment program is supplemented with antispasmodics, antihistamines, and microcirculation correctors. Trigger point blockade is carried out with a mixture of glucocorticoids and local anesthetics. They give a referral for ultraphonophoresis and galvanization with novocaine. - Muscle pathologies
. For bruxism, an integrated approach is effective, including medication, dental, physiotherapeutic, psychotherapeutic methods, and the use of protective mouthguards. Patients with myofascial syndrome are prescribed muscle relaxants, NSAIDs, and antidepressants. - IHD
. As part of drug therapy, antianginal agents, beta-blockers, calcium channel blockers, antioxidants, antiplatelet agents, and antisclerotic drugs are indicated.
Surgery
The choice of surgical technique depends on the cause of the symptom:
- Inflammatory diseases
: opening, drainage of abscesses and phlegmons, sequestrectomy for osteomyelitis. - Injuries
: open osteosynthesis using bone sutures, polyamide thread, mini-plates. - Neoplasms
: curettage, excision of benign neoplasia within healthy tissue (often with extraction of teeth), resection or disarticulation of the lower jaw for a malignant tumor. - Neuralgia
: microsurgical decompression, percutaneous radiofrequency destruction, stereotactic radiosurgery. - IHD
: thrombolysis, emergency coronary angioplasty in the acute period of a heart attack; planned coronary artery bypass surgery, balloon angioplasty for angina pectoris, post-infarction conditions.
Reason: wisdom teeth
Wisdom teeth, or “eights,” are the outermost teeth in the jaw row. They cut their teeth between the ages of 16 and 25, when the replacement of permanent teeth has already ended. Not all people have “Eights” - some do not have them or are not present in full.
Why does it hurt to open your mouth?
The intensity of pain depends on the characteristics of tooth eruption and the individual pain threshold.
In this case, it's all about the location of the wisdom teeth.
They are located on the edge of the jaw arch in the cheekbone area, the distance between them and the temporomandibular joint is minimal.
In addition, the rudiments of the “eights” are usually located in the gum deeper than the others, so their eruption is much more painful than the appearance of other teeth, causing swelling of the gum mucosa, which can spread to the soft tissues around the joint.
Nature of pain and accompanying symptoms
The pain in such situations is constant, it intensifies when you try to open your mouth completely, while talking, chewing, and it hurts to yawn.
The intensity of the pain depends on the characteristics of tooth eruption and the individual pain threshold - from mild discomfort to serious pain that prevents you from falling asleep.
In addition, the gums swell, the submandibular lymph nodes enlarge, and the temperature may rise. In some cases, the mouth practically does not open.
How to relieve the condition
To relieve pain, you can use medications - Kamistad, Kalgel ointments. To relieve inflammation and swelling, the oral cavity is rinsed with solutions of antiseptics, painkillers and medicinal herbs.
A cold compress may also improve the condition. It is acceptable to take painkillers. If noticeable improvement cannot be achieved within 3-4 days, you need to go to the dentist.
General recommendations
Since the causes of unilateral pain in the lower jaw are varied, it is not recommended to eliminate the symptom on your own. Even within the same pathology, consultation with professionals in several fields is necessary. Prevention of this unpleasant sensation is difficult for the same reason. However, adherence to oral hygiene rules, avoidance of frequent use of chewing gum (increases stress on the muscles), preventive examination by a dentist, refusal of self-medication and timely contact with a professional significantly reduce the risk of an undesirable prognosis.
Vascular damage
Pathological processes in the vessels can lead to disruption of the blood supply to the jaw joint. In this case, the patient not only experiences pain when opening the mouth, but also experiences disturbances in its mobility.
Cause of pain
Pain occurs due to impaired blood supply to the muscles of the lower jaw, as well as due to inflammatory processes in the vessels themselves
Pain occurs due to impaired blood supply to the muscles of the lower jaw, as well as due to inflammatory processes in the vessels themselves.
Nature of pain and accompanying symptoms
The pain can be burning (arteritis), pulling, pressing, squeezing.
It can spread not only to the joint and jaw, but also to neighboring areas - the ear, the wings of the nose, the cheek. Concomitant symptoms include impaired mouth opening.
Treatment methods
Depends on the specific pathology of the vessel. Various therapeutic measures can be carried out - the use of anti-inflammatory drugs, painkillers, and, if necessary, surgery on the vessels of the lower jaw.
Pain when opening a child's mouth
The peculiarity of pain in children is that the child can rarely describe the symptom in detail, as well as assess its severity. In addition, children often tend to hide from adults if they are in pain, especially if they are afraid of doctors.
Parents should pay attention to the following features:
- The child began to speak slurredly and reluctantly;
- It is painful or impossible to open your mouth wide;
- Does not eat well, tries to avoid chewing food;
- There is noticeable swelling on one side of the face;
- The baby holds on to the ear or jaw and constantly touches them.
These signs can indirectly tell parents that the baby has a sore jaw.
Neurological pathologies
Neurogenic pain, i.e. sensations caused by pathologies of the facial or trigeminal nerve often occur after hypothermia, head and face injuries. They are always accompanied by a number of additional symptoms, which makes it possible to determine nerve damage.
Why does it hurt to open your mouth?
It is recommended to use anti-inflammatory drugs, painkillers, warming procedures, and neuroprotectors
Opening the mouth is accompanied by pain because the affected nerve is irritated.
The nature of the sensations and accompanying symptoms
The pain can be completely different in nature.
Associated symptoms depend on which nerve is affected - pain in neighboring areas of the face, dry mouth, impaired facial expressions, cough, sore throat, swallowing problems, sore throat, inability to chew, impaired diction.
Treatment methods
The use of anti-inflammatory drugs, painkillers, warming procedures, and neuroprotectors is recommended. Operative methods are ineffective.
Neoplasms
Malignant neoplasms of the oral cavity are deadly, but often their early manifestations seem harmless.
Why does it hurt to open your mouth?
Malignant neoplasms of the oral cavity are deadly, but often their early manifestations seem harmless
Pain is associated with damage to the soft tissues located next to the temporomandibular joint on the right and left sides, their partial destruction.
Damage to the joint itself is also possible.
The nature of the sensations and accompanying symptoms
The pain is increasing, constant, and in the last stages of the disease the patient cannot sleep.
There is bad breath, ulcers on the mucous membranes, tooth loss, diction and voice problems.
Treatment methods
Chemotherapy and radiation treatment are used to treat malignant tumors. Carrying out a full-fledged operation with the removal of damaged tissue is impossible due to the large number of vital structures - vessels, nerves.