Constant nasal congestion, persistent runny nose... We all know how unpleasant and debilitating such a condition can be. Meanwhile, the reason does not always lie in the runny nose or cold itself. One of the factors that provoke constant nasal congestion may be hypertrophy of the nasal turbinates. Symptoms of turbinate hypertrophy are very similar to those of allergic and chronic rhinitis. Treatment of turbinate hypertrophy depends on the cause of the development of this condition, and may include both conservative and surgical methods. We will talk in more detail about the nature, symptoms, as well as methods of treatment and diagnosis of this disease below.
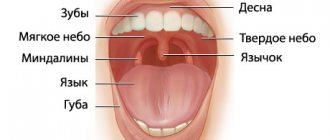
The turbinates are spongy bony structures located in the nasal cavity on the side wall that guide and regulate air flow in the nasal passages. A person has three such paired bony outgrowths on both sides of the nasal septum, which are divided into upper, lower and middle. The turbinates are covered with ciliated epithelium, a special type of mucous membrane that cleans and moisturizes the air passing through the nose. The epithelium also serves as an immunological defense against bacterial and chemical irritants, its cells causing a rapid immune response in the form of an inflammatory reaction to the first signs of microbial or chemical irritation.
SUMMARY
Over the past 130 years, at least 13 surgical techniques have been used to treat inferior turbinate hypertrophy. This article reviews and critically analyzes these methods. Our review of the literature revealed a serious lack of qualified research. There are very few prospective comparative randomized surgical outcome measures. In our opinion, the goal of inferior turbinate surgery should be to reduce complaints while maintaining function. From the above it follows that, apparently, electrocautery, chemical caustic, turbinectomy (subtotal), cryosurgery, and superficial laser surgery should not be used, since these technologies are too destructive. Intraturbinal reduction of conchae (intraturbinal turbinoplasty) seems to be the method of choice.
INTRODUCTION
One of the main causes of chronic nasal congestion is the pathology of the inferior turbinates. However, today there is no agreement on solving this problem. The method of choice is mainly pharmacological treatment. In most cases, nasal topical steroids, antihistamines, and decongestants provide good results. Patients who do not respond to this treatment usually undergo turbinate reduction surgery. Since the last quarter of the 19th century, at least 13 different technologies have been introduced. Some of them have already been abandoned, while others are still in use or have been reintroduced. There is, however, considerable disagreement about the merits of various technologies (Jackson and Koch, 1999).
Some authors consider conchotomy as the most acceptable method of treatment, while others condemn it as too aggressive and irreversibly destructive. Another controversial technology is laser treatment. Although a number of authors have recently advocated this technique, many rhinologists do not approve of it, since the laser destroys the mucous membrane and consequently reduces its functioning. In light of this and other controversies, this article reviews and evaluates publications on the surgical treatment of hypertrophied turbinates.
Research methods
A thorough history and life history was collected. To assess the symptoms of nasal obstruction, the NOSE (Nasal obstruction symptom evaluation) scale was used [9–11], which included 5 points (Table 1), with each item assessed on a 5-point Likert scale. Patients were asked to complete the questionnaire by circling the answer that most closely described their current symptoms. Scores were summed and multiplied by 5 (to perform analyzes based on 100 points). Possible results for assessing the degree of satisfaction with nasal breathing: “nasal breathing is satisfactory” (range 5–25 points, NOSE-1), “moderate degree of dissatisfaction” (range 30–50 points, NOSE-2), “moderate degree of dissatisfaction” (range 50–75 points, NOSE-3) and “high degree of dissatisfaction” (range 80–100 points, NOSE-4) [11]. Rhinological, allergic, and neurological history data were also taken into account when filling out an additional questionnaire with elements of a visual analog scale [11].
The study also used a subjective rating scale (SRS) [12]. Patients independently assessed the degree of nasal congestion, rhinorrhea, and impaired sense of smell. The SOSH test (Table 2) consists of 3 points assessing typical symptoms of AR with SOPS hypertrophy on a 4-point scale characterizing the severity of symptoms: 0 points corresponds to the minimum, 3 points to the maximum severity [12].
Statistical analysis
For statistical processing of the obtained data, Microsoft Excel ver. software was used. 12.0.4518.1014, SPSS Statistics 20. Descriptive statistics methods were used to evaluate the results. For comparative analysis of groups based on quantitative characteristics, the nonparametric Mann-Whitney U test was used. To assess the relationship between signs, correlation analysis was used to calculate the correlation using the Spearman method. Differences were considered statistically significant at p<0.05.
FUNCTIONS OF THE NASAL TUNCHANTS
To critically evaluate the various methods of turbinate reduction, we must first understand the function of the turbinates. We will then define the criteria that surgical techniques must meet to be considered acceptable.
The nasal turbinates, especially the inferior ones, perform several important functions. First, they contribute to inspiratory resistance, which is necessary for normal breathing. The greater the nasal resistance, the greater the negative intrathoracic pressure required for inspiration. The large negative pressure, in turn, increases pulmonary ventilation and venous return to the lungs and heart (Butler, 1960; Haight and Cole, 1983). This is what we would call the "resistive function" of the turbinates. Second, as part of the nasal valve, the inferior turbinate helps convert inspiratory airflow from laminar to turbulent. Turbulence in the outer layers of air increases the interaction between the air and the nasal mucosa. This improves humidification, warming and air purification. Due to the large surface of the mucous membrane and extensive blood supply, the inferior conchae play a large role in this process. This role can be called the "diffuser function" of the inferior turbinates. Finally, they are important in the nasal defense system (mucociliary transport, humoral and cellular defense). All of these functions require large amounts of normally functioning mucosa, submucosa, and turbinate parenchyma.
Causes of vasomotor and hypertrophic rhinitis
In the nasal cavity there are the nasal turbinates (inferior, middle, superior), which consist of a huge number of different plexuses of blood vessels. They narrow and expand, thereby regulating the lumen of the nasal passage, and consequently, a person’s breathing. The narrowing and expansion of these vessels depends on the temperature and humidity of the environment, atmospheric pressure, etc. For example, in the cold season, the vessels in the nose expand, and this allows you to inhale cold street air more slowly, which warms you up better.
The mechanism for regulating vascular tone can be disrupted under various pathological and physiological conditions, such as:
- deviated nasal septum;
- allergic rhinitis;
- endocrine diseases;
- pregnancy.
At the same time, the vessels that are located under the nasal mucosa are constantly filled with blood, which significantly thickens the mucous membrane, and therefore interferes with proper breathing through the nose. This leads to the development of vasomotor rhinitis , and in the long-term process to hypertrophy of the nasal turbinates and persistent difficulty in nasal breathing.
Possible complications of vasomotor rhinitis
With constant difficulty in nasal breathing, patients often begin to use vasoconstrictor drops for a long time, which leads to negative consequences. Using decongestants for more than 5–7 days may cause:
- damage to the ciliated epithelium in the nasal cavity;
- development of chronic dry rhinitis, accompanied by the formation of crusts in the nasal cavity, sanguineous discharge from the nose;
- chronic vasospasm and, as a result, increased blood pressure;
- chronic cerebral hypoxia;
- disruption of ventilation of the paranasal sinuses and patency of the auditory tubes, which subsequently leads to the development of various pathological processes in the paranasal sinuses and middle ear.
It is to prevent all these complications that it is necessary to consult a specialist as early as possible.
CRITERIA FOR EVALUATING METHODS FOR REDUCING THE VOLUME OF NASAL TURNACLES
All methods must be assessed according to two main criteria:
- The effectiveness of the technology to reduce difficulty breathing, hypersecretion, sneezing and headaches;
- Side effects that occur in the immediate and long term. In other words, the extent to which the functional tasks of the nose are respected and preserved. It would be a mistake to focus solely on the degree of dilation of the nasal passages based on endoscopic findings, rhinomanometry, and acoustic rhinometry. A wider nasal cavity does not necessarily mean that the nose works better. The goal of surgical treatment should be “elimination of complaints while maintaining function” and “optimal amount of reduction while maintaining function” (Huizing, 1998). Taking this concept as a basis, this review evaluates various inferior turbinate reduction techniques used in the past or currently in use. They are described briefly and critically assessed in chronological order. A basic overview of the sources is presented in Table 1.
Table 1. Various treatments for inferior turbinate hypertrophy
| Method | Year of implementation | Used | Left |
| Thermal coagulation, electrocautery | 1845–1880 | + | |
| Chemical coagulation, chemocaustics | 1869–1890 | + | |
| Turbinectomy | 1882 | + | |
| Lateralization, lateropexy | 1904 | + | |
| Submucosal bone resection | 1906–1911 | + | |
| Crush+flatten, partial resection | 1930–1953 | + | |
| Corticosteroid injections | 1952 | + | |
| Injections of sclerosing drugs | 1953 | + | |
| Videoneurectomy | 1961 | + | |
| Cryosurgery | 1970 | + | |
| Turbinoplasty | 1982 | + | |
| Laser surgery | 1977 | + | |
| Power tools | 1994 | + |
METHODS FOR DIAGNOSIS OF HYPERTROPHY OF THE NASAL TUNCENTS
- History taking and physical examination. During the examination, complaints are clarified and the nose is examined using a rhinoscope - a special dilator.
- Nasal endoscopy. Nasal endoscopy is a minimally invasive medical procedure performed to diagnose nasal diseases. It helps to examine the inner lining of the nose and visualize its cavity, which is impossible to do with a regular examination. The procedure is performed using a nasal endoscope, which consists of a thin, flexible tube with fiber optics to illuminate the nasal cavity. The endoscope is connected to a light source and a video camera, which sends images to a monitor. During an endoscopy, pictures may be taken or recorded for further examination.
THERMAL COAGULATION - ELECTROCAUSTIC
The first method for treating hypertrophied inferior turbinates was electrocautery. Already in 1845, its use was supported by Heider from Vienna and Krusel from St. Petersburg. After the dissertation of Middeldorpff (1854) and the work of Bruns and Voltolini (1871), this method gradually gained popularity. It eventually gained widespread use following the introduction of cocaine as a local anesthetic (Koller, 1884) and adrenaline (epinephrine) as a vasoconstrictor (1897). In the 1880s, electrocautery of the nasal mucosa was used not only to treat nasal diseases, but also to treat other ailments such as dysmenorrhea, abortion, gastralgia, etc. In those days, "nasal reflex neurosis" (Fliess, 1893) was a common superstition. Electrocautery has increasingly been criticized for its need for repetition and because it leads to serious complications such as synechiae and stenosis. In 1890, at the World Congress in Berlin, this procedure became the target of ridicule: “And then the nose is burned out, because, as we know, this always helps!”
Surface electrocaustics. The first method was galvanocaustics using a galvanic apparatus (Voltolini, 1871). The standard technique consists of coagulation from back to front with two parallel grooves along the medial surface of the concha. High temperature coagulates the tissue, causing necrosis, which leads to fibrosis and shrinkage of the shell (Figure 1). While bleeding is rare, temporary complaints of crusting are noted. Over time, various types of electroplating tools have been developed. Later, high-frequency surface diathermy was introduced (e.g., Bourgeois and Poyet, 1922; Castex, 1929; Sinskey, 1932; Jaros, 1933). This technology has been used for both zonal tissue destruction and linear coagulation.
Figure 1. Surface electrocautery technique (from the textbook Laurens, 1924)
Surface electrocautery is a clearly destructive procedure. It causes mucosal atrophy, metaplasia, loss of cilia and decreased mucociliary transport. Permanent crusts and synechiae may form between the nasal septum and the turbinates. Although these undesirable effects are known, it remains one of the most commonly used methods in practice.
Coblation (“controlled ablation”) is a very recently introduced method of high-frequency bipolar diathermy. Because the results are achieved at low temperatures, damage to surrounding tissue is minimized (Smith et al., 1999).
Intraturbinal coagulation. Since superficial electrocautery causes significant damage to the mucous membrane, intraturbinal thermocoagulation was introduced. Neres (1907) introduced a gold needle during this procedure and then passed a galvanic current for several seconds. Horn in 1908 described a similar submucosal technology. Later, high-frequency diathermy was introduced. Beck in 1930 was apparently the first to describe the use of a monopolar electrode for submucosal linear burning. Hurd first reported bipolar intraturbinal diathermy in 1931. Two parallel wires were inserted through the anterior incision into the depth of the shell (Figure 2). Then horizontal parallel grooves 2-4 mm deep are burned into the shell tissue in the direction from back to front. After World War 2, Richardson (1948) and Shahinian (1953) again reported submucosal diathermy. Like the Hurd, they both used a bipolar electrode to ensure precise current delivery. Simpson and Grooves (1958) advocated the use of a monopolar electrode because a single wire is easier to position. The effect of submucosal diathermy is achieved by coagulation of the venous sinuses within the concha, resulting in submucosal fibrosis (Woodhead et al., 1989). This method has several disadvantages. Firstly, it is difficult to dose the volume of tissue treated in depth (Wengraf et al., 1986). Second, the results are often temporary, requiring the procedure to be repeated (Jones and Lancer, 1987; Meredith, 1988). The most common complications are late bleeding, prolonged nasal discharge and crusting (Meredith, 1988; Williams et al., 1991). Despite these disadvantages, submucosal diathermy remains the treatment of choice for most ENT physicians, simply because of its ease of performance and relatively rare complications.
Figure 2. Bipolar intraturbinal coagulator (after Hurd, 1931)
Radiofrequency turbinate reduction (RTR)
During this procedure, the doctor performs local anesthesia of the nasal cavity, after which the patient is positioned on the treatment table and the doctor performs radiofrequency reduction of the nasal turbinates using a special electrode. The principle of operation of RTR is based on short-term heating of the tissues of the nasal concha with an electrode, which leads to their compression and expansion of the respiratory passages.
What a patient should expect when undergoing the procedure in Singapore:
- Preparing for RTR only takes 15-20 minutes;
- The procedure is mostly painless and minimally uncomfortable;
- Immediately after the procedure, the patient may not experience significant relief from congestion due to slight swelling and crusting. However, immediately after the cleaning (which is performed by the doctor a few days after the procedure), the patient will be able to experience the full benefits of radiofrequency turbinate reduction;
- The procedure does not require hospitalization - the doctor performs it on an outpatient basis in the clinic. Immediately upon completion, the patient can return to his daily activities;
- The period of complete recovery and healing takes about 4-6 weeks;
- During the first few days after the procedure, patients are not recommended to swim in the pool.
CHEMICAL COAGULATION - CHEMOCAUSTICS
The use of chemical coagulation of the surface of shells in order to reduce their size also came into practice in the last decades of the 19th century. First, a saturated solution of trichloroacetic acid (TCA) was used, which was applied to the mucous membrane (eg, von Stein, 1889); later, chromic acid melted to form a pearl was also used (Figure 3). As early as 1903, doubts arose about the merits of chemical coagulation. In most clinics the results were described as positive, but microscopic examination revealed severe necrosis of the mucous membrane (Meyer, 1903). This author recommended intensive application of TCA, with the assumption that the epithelium would recover better as new epithelium outgrew the necrotic tissue.
Figure 3. Melting chromic acid into a pearl for chemocaustics of the mucosal surface (from the textbook Seiffert, 1936)
This method is becoming less and less popular. Due to its limited effect on the volume of the turbinates, this procedure requires repetition several times. Secondly, this technique leads to serious damage to the nasal mucosa with characteristic symptoms of atrophic rhinitis.
Taking into account the “optimal amount of reduction while preserving function”, this technology should be strictly prohibited. This technique is the worst thing imaginable: while the shells are only slightly reduced, it causes massive destruction of the functional structures of the mucous membrane, cilia and glands. It is noteworthy that this method has recently been advocated as safe and effective in reducing hypersecretion in patients with nasal hyperreactivity and allergies (Yao et al., 1988, 1995).
Vasotomy – what do patients need to know?
Vasotomy must be performed under general anesthesia, since the procedure requires precise work by the surgeon, and the patient's movement can lead to a negative impact on the outcome of the operation.
Discontinuation of blood thinning drugs such as acetylsalicylic acid should be done after consultation with your doctor 7-10 days before surgery. Stopping medications for a short period of time significantly reduces the risk of postoperative bleeding.
CONCHOTOMY
Resection and surgical reduction of turbinates has been known since the last decades of the 19th century. To our knowledge, Jarvis (1882) was the first to describe resection of parts of the inferior concha using a wire loop. Then in the 1890s, Hartmann described his experience with operations on the inferior conchae (cited in Mabry, 1988). Later, Jones (1895) and Holmes (1900) proposed total conchotomy. This method of irreversible resection was soon criticized. Spielberg (1924), for example, warned fanatical rhinologists who would not rest until they had removed, resected, or cauterized every mass they found in the nasal cavity. The disadvantages of conchotomy were obvious. Some patients suffered from atrophic rhinitis or what is known as secondary ozena with symptoms of nasal dryness, crusting, bleeding, soreness and headache (eg Dutrow, 1935; Harris, 1936; House, 1951; Tremble, 1960). Conchotomy was discredited; many surgeons have opted for more conservative techniques such as lateralization and submucosal resection. However, total conchotomy was again recommended by several authors in the 1970s and 1980s (Fry, 1973; Courtiss et al., 1978; Martinez et al., 1983; Pollock and Rohrich, 1984; Ophir et al., 1985; Odetoyinbo, 1987; Thompson, 1989; Wight et al., 1990). Some of these authors disputed the claim that conchotomy leads to post-turbinectomy syndrome, or “empty nose” syndrome as it has recently been called (Stenquist and Kern, 1997). The rationale was that this undesirable postoperative effect was never reported by Courtiss and Goldwyn (1990), who wrote: “The fear of dry nose syndrome is unfounded.” Others disagree, reporting long-lasting signs and symptoms of crusting, dryness, and pain in some patients (Moore et al., 1985; Salam and Wengraf, 1993; Garth et al., 1995; Neves-Pinto, 1995; Berenholz et al. , 1998). An overview of controversial reports is presented in Table 2.
Table 2. Development of dryness and crusting after (sub)total resection of the inferior turbinates according to recent studies
| Author | Dryness and crusts |
| Courtiss and Goldwyn '83, '90 | NO |
| Martinez et al. '83 | NO |
| Moore et al. '85 | YES |
| Ophir '85, '90 | NO |
| Odetoyinbo '87 | NO |
| Thompson '89 | NO |
| White '90 | YES |
| Salam and Wengraf '93 | YES |
| Carrie et al. '96 | YES |
| Berenholz '98 | YES |
Recurrent nasal congestion has already been reported (Otsuka et al., 1988; Wight et al., 1990; Carrie et al., 1996). In addition to long-term consequences, early complications, especially severe bleeding, must be taken into account (Fry, 1973; Dawes, 1987).
In our opinion, in patients with hypertrophy of the inferior turbinates, total or subtotal conchotomy is not justified. Conchotomy is incompatible with the “preservation of function” task. Conchotomy is irreversible and deprives the nose of one of its important organs. Thus, there is no place for this technology in modern functional nasal surgery. To achieve the desired effect, there are more conservative surgical methods. This view was recently confirmed in a comparative randomized trial by Passali et al. (1999). These authors compared the long-term results of six different technologies using patient symptom severity scores, rhinomanometry, acoustic rhinometry, mucociliary clearance measurements, and secretory IgA measurements before and after surgery. The topic of turbinectomy is closed, since this is the most traumatic technology (Table 3).
Table 3. Main results of a prospective randomized study of six different methods of reduction of the inferior turbinates, as concluded by Passali et al., (1999)
| Technology | Effect on nasal congestion | Recurrence of nasal congestion | Effect on function | Complications |
| Electrocaustics | + | + | – | + |
| Cryosurgery | + | + | – | + |
| Laser surgery | + | + | = | + |
| Submucosal reduction | + | + | = | + |
| The same + lateralization | + | – | = | 0 |
| Turbinectomy | + | – | – | 0 |
LATERALIZATION, LATEROPEXY
In response to the side effects of conchotomy, Killian proposed lateralization of the inferior turbinate in 1904. The concha was broken and displaced laterally by a flat elevator or nasal planum with long branches. This procedure is simple and does not have any particular risks or complications (Salam and Wengraf, 1993). On the other hand, it does not seem particularly effective. Lateralization is performed well when the inferior meatus is wide enough to move the inferior concha. Otherwise, she tends to take her previous position (Goode, 1978). Lateralization is an acceptable technique in terms of preserving function. Since its effect is limited, it can be used as an additional procedure, for example, in combination with septal surgery.
Lateropexy (or conchopexy) involves moving the fractured concha into the maxillary sinus after removing part of the lateral wall of the nose (Fateen, 1967; Legler, 1974, 1976). It is quite clear that this method has not gained much popularity.
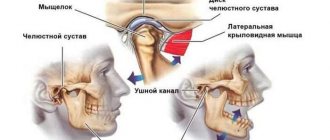
Diagnostics
When diagnosing the symptoms of acute sinusitis, rhinoscopy (examination of the nasal cavity), endoscopy of the nasal cavity, x-ray examination and, if necessary, diagnostic puncture of the maxillary sinus with bacteriological examination of the washed contents are performed. If necessary, studies are prescribed using pulsed ultrasound, thermal imaging, computed tomography (CT) and magnetic resonance imaging (MRI). It is imperative to carry out a differential diagnosis of acute sinusitis and distinguish it from neuralgia of the first and second branches of the trigeminal nerve.
SUBMUCOUS RESECTION OF THE BONE OF THE INNER TUNALE
Complications after conchotomy have forced a number of surgeons to look for more conservative surgical methods to reduce the size of the inferior turbinate. The first surgical alternative presented was submucosal resection of the inferior turbinate bone (Low, 1906; Linhart, 1908; Würdemann, 1908; Zarniko, 1910). Würdemann stated that he was “irritated by almost every case of complete removal of the turbinate” and wanted to “prevent disastrous results.” A milder version of this new concept was described by Freer in 1911: “to submucosally elevate the membrane of the inferior turbinate with a sharp elevator, a fairly small vertical incision is made, and further exposed with a sharp raspator, this approach permits a longitudinal resection of the inferior turbinate” (Figure 4). Although convincing, this technique received only limited use (Strandberg, 1924; Odeneal, 1930; Harris, 1936). In 1951, Howard House revived this method. Good results were later reported by Loibl and Pfretzschner (1972) and Tolsdorff (1981), who combined this method with lateral displacement. Mabry (1982, 1984) refined this technique and coined the term “turbinoplasty.” Observing patients after surgery for a year, he found that the size and function of the shells remained normal. In a study conducted by Passali et al. (1999), submucosal bone resection combined with lateral displacement was rated as the best method in terms of effectiveness and preservation of function.
Figure 4. Intraturbinal resection of the bone and parenchyma of the inferior turbinate through a vertical incision (a) of the head of the concha (after Freer, 1911)
Contraindications to vasotomy and conchotomy of the nasal turbinates
The main contraindications to operations on the nasal turbinates are:
- acute inflammatory diseases in the nasal cavity and paranasal sinuses
- bleeding disorder
- atrophic and ulcerative processes of the mucous membrane of the nasal cavity..
- severe concomitant diseases in the stage of decompensation (heart, kidney failure, diabetes mellitus, etc.)
Endoscopic vasotomy and conchotomy, performed at the Yauza Clinical Hospital, make it possible to preserve the nasal concha, and most importantly, to restore free nasal breathing.
CORTICOSTEROID INJECTION
In 1952, injections of long-acting corticosteroid solutions were introduced as a new technique for reducing hypertrophied turbinates (Semenov, 1952). A number of authors have reported that corticosteroid injections are effective in eliminating nasal hyperresponsiveness, regardless of etiology (Semenov, 1952; Simmons, 1960, 1964; Baker and Strauss, 1963). Corticosteroid injections are minimally invasive, but the subjective improvement in nasal breathing is short-lived. This procedure successfully reduces turbinate swelling for only 3 to 6 weeks (Mabry, 1979, 1981). Later, most authors rejected concha injections because they can cause acute homolateral blindness (Baker, 1979; Byers, 1979; Evans et al., 1980; Mabry, 1982; Saunders, 1982; Rettinger and Christ, 1989).
NEUROECTOMY OF THE VIDIAN NERVE
In 1961, Golding-Wood took a fundamentally new approach to solving the problem. He proposed cutting the parasympathetic nerve fibers in the Vidian canal to reduce the parasympathetic tone of the nasal mucosa. In this way he hoped to reduce the symptoms of hypersecretion and nasal congestion. This technology was developed in an era when drug treatment for hypersecretion was still very limited. Subsequently, various approaches to the Vidian Canal were developed. Initially, the transantral approach was used (Golding-Wood, 1973; Ogale et al., 1988), later supplemented by the endonasal method with ganglion coagulation (Portmann et al., 1982). Neuroectomy of the Vidian nerve has been widely used, but its effect has been limited (Krant et al., 1979; Krajina, 1989). Hypersecretion was reduced, but not nasal congestion (Principato, 1979). For these reasons, this technology was abandoned in the early 1980s.
CRYOSURGERY
Cryosurgery was introduced in the 1970s by Ozenberger (1970). This method involves freezing the shell under local anesthesia with a cryoprobe using nitrous oxide or liquid nitrogen as a cooling agent. Necrosis after freezing was found to be different from that after caustic. It was assumed that the necrotic tissue would be replaced by new respiratory epithelium. Although the method has become widespread, published results have varied (Grache and Holopainen, 1971; Puhakka and Rantanen, 1977; Principato, 1979; Bumstead, 1984; Chiossone et al., 1990, Hartley and Willatt, 1995). The immediate results were largely satisfactory, but the outcome was not durable (Warwick-Brown and Marks, 1987; Haight and Gardiner, 1989; Rakover and Rosen, 1996). According to Puhakka and Rantanen (1977), performance improves after repeated applications.
Other than transient headache, no postoperative sequelae have been reported (Moore and Bicknell, 1980). One month after surgery, there is a marked reduction in the orifices of the glands, scar tissue has formed, and the ciliated epithelium appears normal (Principato, 1979; Keller-hans and Schlageter, 1988). However, in some studies, mucociliary clearance did not return to normal (Wengraf et al., 1986; Elwany and Harrison, 1990). According to some authors, cryosurgery would be more effective for allergic rhinitis than for non-allergic turbinate hypertrophy, since it is particularly effective in controlling rhinorrhea (Principato, 1979; Rakover and Rosen, 1996).
Cryosurgery was gradually abandoned for a number of reasons. It is difficult to predict the amount of tissue removed. Moreover, compared with other methods, long-term results are disappointing, as recently confirmed by studies by Passali et al. (1999).
CRUSHING AND LEVELING - PARTIAL RESECTION
The long-term complications of total turbinectomy have convinced most rhinosurgeons that partial resection of the inferior turbinate would be the best choice. Several technologies have been proposed - trimming, horizontal and diagonal resection of the lower edge; resection of the posterior part and resection of the anterior part.
In 1930, Kressner introduced crushing of the shell with specially designed blunt forceps and then straightening it. Since then, this method has been used by several surgeons. This technology was successfully used in our department (Huizing, 1988).
Resection of the posterior end of the concha was proposed, among others, by Proetz (1953), since he believed that in most cases it is the posterior half of the inferior turbinate that causes difficulty in nasal breathing.
Goode (1978), Pollock and Rohrich (1984), Fanous (1986), and many others have advocated resection of the anterior portion of the inferior turbinate. Unlike Proetz, they considered the head of the inferior turbinate as the most common obstruction to breathing.
Horizontal inferior resection of the inferior margin was recommended by Courtiss and Goldwyn (1990), Dessi et al. (1992), Ophir et al. (1992), Percodani et al. (1996). This method avoids the risk of bleeding from the pterygopalatine artery (Garth et al., 1995). Some authors argue that it only partially solves the problem because symptoms return (often due to new hyperplasia) and the outcome worsens over time (Courtiss and Goldwyn, 1983, 1990; Warwick-Brown and Marks, 1987; Wight et al ., 1990; Schmelzer et al., 1999).
Spector (1982) proposed diagonal resection of most of the turbinate. With this method, the functionally important head of the inferior turbinate is preserved. Severe bleeding from the posterior nasal cavity may occur as this technique cuts off a large source of blood supply to the turbinate (Padgham and Vaughan-Jones, 1991).
From a function preservation perspective, all of the partial turbinectomy options discussed above appear acceptable if performed in a gentle manner. We particularly prefer shell crushing followed by horizontal leveling, as this technique seems to be the best compromise between the desired result and side effects. In our opinion, resection of the head of the concha appears to be too destructive. It can relieve anterior obstruction, but partially deprives the nose of its resistive and diffuser functions. Resection of part of the posterior end of the concha appears functionally acceptable, but is effective only in patients with pathology limited to the tail of the concha.
Material and research methods
The present pilot observational study was conducted from June to September 2022 at the ENT Department of Thai Nguyen National General Hospital (Vietnam) after receiving approval from the hospital's ethics committee. Patients living in both urban and rural areas applied to the ENT department. The urban environment is characterized by a population density of 400–3000 people per 1 km2 (data for 2022), the rural environment - by a density of 200–400 people per 1 km2, as well as developing modern agricultural production and industrial enterprises.
TURBINOPLASTY
In the 1980s, the term “turbinoplasty” was coined (Mabry, 1982, 1984). It combines various intraturbinal methods of surgical reduction of the inferior turbinate while preserving the mucous membrane. Recently, a number of authors have developed and disseminated techniques for intraturbinal reduction of the inferior turbinate (Gray, 1965; Lenders and Pirsig, 1990; Grymer et al., 1993; King and Mabry, 1993; Illum, 1997; and Marks, 1997; Huizing, 1998). After displacing the concha medially, an L-shaped incision is made on its inferolateral edge. The mucosal flap is raised and a portion of the bone and parenchyma is resected as needed. Then the mucous flap is placed in place and fixed.
Figure 5. Anterior turbinoplasty technique according to Pirsig and Huizing (from the textbook Huizing and De Groot, 2001)
a. Medialization and L-shaped incision of the head of the nasal concha with a Beaver knife No. 64; b. Separating a flap of the mucous membrane and resection of part of the bone and adjacent parenchyma of the inferior turbinate; c. Placement and fixation of the mucosal flap and lateralization of the reduced inferior turbinate.
When the resection of bone and parenchyma is limited to the anterior part of the concha, we speak of an “anterior turbinoplasty.” This technique is used in patients with inspiratory respiratory obstruction due to hyperplasia of the head of the concha. Another technique is “partial lower turbinoplasty.” This technique involves making two separate incisions that connect at the center of the shell. The wedge-shaped part of the shell is then removed and the edges of the resulting defect are joined together (Schmelzer et al. 1999). Intraturbinal turbinoplasty allows for size reduction while preserving all mucosal functions, as recently demonstrated by Passali et al. (1999) in a comparative study. Its second advantage is the low likelihood of postoperative bleeding and crusting. From the point of view of “optimal amount of reduction while preserving function,” intraturbinate turbinoplasty is the method of choice for the treatment of turbinate hypertrophy. This is a tissue-reducing procedure, but it can be modified according to pathology without regard to mucosal function.
LASER SURGERY
Lenz in 1977 was the first to report the use of laser technology for reduction of the inferior turbinate, using an argon laser (Lenz et al., 1977; Lenz, 1985). Subsequently, other types of lasers were used: CO2 laser (Mittelman, 1982; Simpson et al., 1982; Fukutake et al., 1986, Kawamura et al., 1993; Kubota, 1995; Lippert and Werner, 1997; Lagerholm et al., 1999; Papadakis et al., 1999; Katz et al., 2000); potassium titanium phosphate (KTP) laser (Levine, 1989, 1991); neodymium-YAG laser (Werner and Rudert, 1992); diode laser (Min et al., 1996); and holmium-YAG laser (Serrano et al., 1998).
The laser produces a beam of coherent light that is absorbed by tissue; the degree of absorption depends on the wavelength. At the same time, its energy leads to evaporation of the tissue. The depth of the resulting damage thus depends on the wavelength, the degree of tissue absorption and the amount of energy applied. Its diameter depends on the size of the laser beam spot. Therefore, laser technology can be used for various purposes depending on the parameters applied. One of the parameters is the operating mode, either continuous or pulsed. Most authors use pulsed mode, since a continuous laser beam can cause damage to a large area. A series of spots or small craters are created on the mucous membrane at a distance of 1-2 mm (Figure 6). Laser energy can be supplied directly (CO2 laser) or through optical fiber (KTP, Nd-YAG, Diode, Ho-YAG). Some authors prefer to make linear cuts as with electrocautery. Continuous radiation expands the thermal damage zone. The laser can also be used to remove tissue during partial (or total) conchotomy or intraturbinal tissue reduction. Thus, laser technology can be used to perform partial conchotomy and intraturbinal tissue reduction. The laser can be used in cases where a knife or scissors would normally be used. We emphasize that laser surgery is not a new operation, but a new type of equipment for performing the operation.
Figure 6. Laser treatment of the inferior turbinate (after Werner and Lippert, Rhinology 35: 33-36, 1997)
Microscopic studies of the mucosa after laser exposure have revealed limited regeneration of the ciliated epithelium, while the number of seromucous glands and cavernous plexuses gradually decreases (Kubota, 1995; Elwany and Abdel-Moneim, 1997). Another study found significant degeneration of the superficial submucosal layer and its replacement by granulation tissue, with scar tissue visible after a year (Fukuta et al., 1986).
Laser turbinate surgery can be performed under local anesthesia on an outpatient basis. The hemostatic properties of laser exposure are such that postoperative bleeding is very rare and nasal tamponade is not necessary. However, temporary crusting is common, and synechiae may also occur.
Published results of turbinate laser surgery vary widely (from “43% success” to “excellent results”). However, almost all studies are retrospective and non-comparative. Therefore, they are of little value and are not considered here. We are aware of only one prospective comparative study that compared the results of different types of laser surgery. This study did not find significant differences (DeRowe et al., 1998).
Laser surgery for conchae does not meet the requirement of “optimal amount of reduction combined with preservation of function.” With limited evaporation of the mucous membrane and submucosal layer, the volume of reduction is clearly insufficient. If the volume removed is sufficient, then the functional changes are severe and irreversible. Therefore, laser surgery is not compatible with the modern concept of functional nasal surgery and should not be used to treat hypertrophied inferior turbinates.
Treatment
Treatment of inflammation of the sinuses is aimed at eliminating the source of infection, the phenomena of the inflammatory process and the evacuation of discharge. In addition, it is necessary to restore ventilation and drainage functions. This is important from the point of view of preventing relapses (repeats) of this disease.
The disease is usually treated on an outpatient basis. For catarrhal rhinosinusitis, local antibacterial and anti-inflammatory treatment is prescribed. It is necessary to carry out so-called “unloading” therapy (washing using the fluid displacement method, YAMIK catheterization, nasal lavage according to Proydu, puncture of the maxillary sinus). Secretomotor (expectorant) and secretolytic (thinning viscous mucus) drugs must be prescribed with caution and according to indications.
In severe cases, as well as in cases of suspected development of possible complications of acute sinusitis (usually rhinogenic meningitis), in the presence of concomitant severe pathology, and if it is impossible to carry out specialized ENT procedures on an outpatient basis, the patient is sent to treat acute sinusitis in the ENT department of the hospital.
For purulent sinusitis, antibacterial drugs must be prescribed simultaneously with anti-inflammatory drugs. One of the washing methods is mandatory. If it is difficult to evacuate mucopurulent discharge from the maxillary sinus, and this happens when the maxillary anastomosis is blocked, a puncture is performed. Sometimes it is carried out several times, until the so-called “clean rinsing waters”.
ELECTRICAL TOOLS
Recently, electric instruments for turbinate surgery such as “shavers” have come into use (Setcliff and Parsons, 1994). These instruments are used both on the conchal surface and intraturbinally, often in combination with endoscopic guidance. They are claimed to allow precise removal of soft tissue. Some surgeons cut away portions of the shell from the lateral and inferior margins, while others work with a shaver inside the shell (Friedman et al., 1999; Van Delden et al., 1999). This technology is said to be fast, effective, well tolerated and low in pain (Davis and Nishioka, 1996).
The use of power tools is determined by personal preferences. It depends little on the type of instrument. This is more of a surgical technique than a measure of the amount of turbinate reduction.