No one is immune from jaw displacement. Dislocation of the lower jaw can occur either as a result of a blow or when the mouth is suddenly opened. But there are a number of factors that provoke the occurrence of such situations. How to behave if jaw displacement occurs? How soon can it be put back in place, and where should one go if the lower jaw is dislocated? Experts answer these questions.
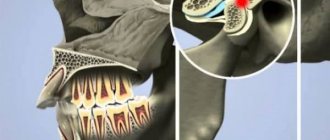
Dislocation of the lower jaw is a situation when the articular head of the temporomandibular joint is displaced. Dislocation can only affect the lower jaw, since the upper jaw is immobile. The mandible is connected to the temporal bone by the TMJ, which helps the mandible move.
Why does dislocation of the lower jaw occur?
Mandibular displacement can occur because:
- the patient suddenly opened his mouth during a conversation or yawned;
- the man dropped his jaw sharply;
- the patient suffers from certain diseases that have weakened the skeletal system and articular ligaments. Among the most common diseases that provoke dislocation of the lower jaw are osteomyelitis, rheumatism, arthritis, etc.;
- a person has a habit of opening bottles with his teeth;
- the temporomandibular joint was affected due to improper distribution of the load on the teeth (for example, if on one side there are no chewing teeth, but on the other side they are there and do more work).
Causes
For each patient, the intensity of mechanical impact for the development of the problem is different. In some people, subluxation can develop when yawning, while others suffer serious blows to the jaw without consequences.
In general, there are a number of situations that lead to displacement of the bone structure:
- Road accidents, fights, traumatic sports in which the maxillofacial region suffers.
- Yawning with a wide opening of the mouth.
- Shout.
- Trying to bite off a hard or large piece of food.
- Involuntary muscle contraction during epileptic or convulsive seizures.
Jaw displacement is not always associated with traumatic factors. Pathology often manifests itself against the background of internal disorders in the human body:
- osteomyelitis;
- arthrosis;
- gout;
- rheumatism.
These diseases gradually lead to joint degeneration and loss of functionality. As a result, the shape of the bones changes and the ligaments are weakened.
How to understand that a dislocation of the lower jaw has occurred?
The symptoms of dislocation of the lower jaw are quite clear:
- it becomes impossible to open your mouth;
- pain is felt in the projection of the jaw, as well as in the area of the temporal bone;
- after dislocation of the lower jaw there may be speech impairments;
- redness may be observed in the area of the temporomandibular joint;
- the lower jaw is pushed forward or shifted to the side;
- against the background of joint dislocation, uncontrolled salivation occurs.
As a rule, a person immediately understands that something is wrong with the lower jaw. Visually, the displacement of the lower jaw is also visible. If you notice similar symptoms of dislocation, you should urgently seek help from a doctor.
First aid
Before visiting a doctor, the patient must be given first aid. All measures in this case will be aimed at minimizing the load on the joint and reducing the intensity of pain symptoms.
First of all, the affected joint is immobilized with a bandage or scarf. The jaw is fixed from top to bottom and from front to back using two flaps of fabric. At this time, the patient is prohibited from speaking and opening his mouth wide.
Options for fixing the jaw using a bandage
If a person has dislocated his jaw, his mouth will be slightly open. To prevent dirt and dust from getting into the cavity, cover it with a damp cloth. This will also reduce saliva production. For severe pain, a non-steroidal solution can be administered intramuscularly. An ice container is placed at the site of the suspected injury to reduce the severity of swelling. This event will also reduce the intensity of pain.
Which doctor should I go to if I have a problem? Jaw injuries require consultation with a surgeon. After examining the patient, the doctor decides whether to realign the joint or perform surgery. Jaw subluxations often occur in the dentist’s office, when the patient opens his mouth wide during manipulation. In this case, the specialist provides the person with qualified assistance on the spot.
If bone damage occurs at night, an ambulance is called for the person. The victim is taken to a 24-hour emergency room, where the necessary manipulations are performed. Before determining a treatment regimen, the doctor orders an x-ray to analyze the characteristics of the injury.
What types of dislocations of the lower jaw are there?
Depending on the side of displacement of the articular head, there are:
- posterior dislocation of the lower jaw (when the jaw moves back);
- anterior dislocation of the lower jaw (when the jaw is pushed forward).
Based on the nature of the injury, we can distinguish:
- complex dislocation of the jaw, when soft and hard tissues are affected, and an open wound is visible;
- simple or closed dislocation of the lower jaw, when the displacement of the jaw bones is not visualized.
Based on the number of affected joints (and there are two of them) in articular dislocation of the lower jaw, the following are distinguished:
- bilateral dislocation of the lower jaw is a complex diagnosis in which the jaw “pops out” of both joints and is therefore pushed forward, the mouth remains slightly open, the jaw moves forward, the person is drooling, and there are problems with speech;
- unilateral articular dislocation of the lower jaw, when one temporomandibular joint is involved, while the chin shifts towards the unaffected joint.
If, when the lower jaw is dislocated, the tips of the bones do not touch each other, a complete dislocation of the lower jaw is diagnosed. If the ends of the bones partially touch, most likely the patient has articular subluxation of the lower jaw.
Classification
All jaw dislocations can be classified according to various indicators:
| According to the placement of the articular head relative to the fossa (it is indicated in which direction it came out) |
|
| By location: |
|
| By statute of limitations: |
|
| By severity: |
|
| By etiology: |
|
Any dislocation can and should be treated. Immediately after the incident, you should go to a hospital or emergency room to seek qualified medical care.
How can you determine that a dislocation of the lower jaw has occurred?
As we said above, based on the symptoms, the patient immediately understands that something is wrong with his lower jaw. A doctor will be able to make an accurate diagnosis based on the following diagnostic steps:
- general examination;
- radiography of the jaw;
- computed tomography or MRI of the joint.
The specialist must also make sure that the dislocation or subluxation does not hide a fracture of the jaw, which is much more serious and requires surgical intervention.
It is important! If a person has a dislocation of the lower jaw as a result of injury or an accident, he should be given first aid - apply a tight bandage to the jaw and take him to a medical facility.
Structure
The formation of the mandibular region is the result of the evolution of the human body. In the process of development, the entire structure became mobile and autonomous, gaining the ability to move freely and perform the basic functions necessary for a person. The temporal joint is localized in the fossa, connecting to the bony part.
When a subluxation occurs, the head of the joint partially comes out of the fossa, succumbing to the influence of external factors. As a rule, this phenomenon becomes a consequence of a general weakening of the ligaments or disturbances in the articular cavity. If you have the proper skills and practical experience, you can restore the original position of the jaw yourself, but the systematic occurrence of such a problem is the basis for complex treatment.
Treatment of lower jaw dislocation
To solve the problem of dislocation of the lower jaw, the jaw should be moved back into place. This should be done exclusively by an orthopedic traumatologist or orthopedic dentist. Adjusting bones yourself after a dislocation is fraught with complications - do not try to repeat the same thing at home, contact a professional.
The procedure for realigning a patient's jaw consists of 5 main steps:
Step No. 1 - the person lies down on a hard surface, takes a comfortable position;
Step No. 2 - the doctor places his thumbs on the chewing teeth of the lower jaw, the remaining fingers seem to clasp the lower part of the face;
Step No. 3 – the specialist makes movements, moving the jaw back and down, but at the same time slightly lifting the chin;
Step No. 4 - the doctor must make sure that the articular head has moved down the back of the TMJ tubercle and returned to its original position;
Step No. 5 – the doctor needs to have time to remove his fingers from the teeth so that the person does not automatically bite them, closing the jaw.
Repositioning the jaw after a dislocation takes several minutes, but must be done very carefully.
If a person’s jaw has been dislocated for a long time and for some reason he has not consulted a doctor, the bones have shifted, he is prescribed surgery under local or general anesthesia.
In case of complex dislocations, a person is recommended to have a reconstructive operation, in which the height of the articular tubercle is artificially increased, while the articular capsule is reduced. Thus, an optimal balance of the elements of the connecting apparatus is achieved, and the jaw does not move.
As a recovery after jaw realignment or surgery to correct a dislocation, the patient is recommended to wear special orthodontic appliances.
Independent actions
When a jaw is dislocated, a person should not make sudden movements. Severe pain is relieved with analgesics. In this case, the victim must know for sure that there is no allergy to the medication. Trauma is often accompanied by increased blood pressure. If the indicator increases significantly, you should take a drug that normalizes blood pressure.
Independent actions when realigning the jaw:
- Fixation of the jaw in one position using available means or a splint.
- Place a bandage in the mouth that will absorb the saliva that is produced.
- Call an ambulance. If the victim cannot speak, then he needs to ask neighbors or passersby for help (if the dislocation occurred on the street). If there is a clinic near the scene of the incident, you should go there immediately.
Before receiving qualified medical assistance, you should say as little as possible, since any movements can cause pain or complications of the dislocation. It is not advisable to adjust the joint yourself. Illiterate actions can lead to damage to the helping fingers or long-term dysfunction of the jaw apparatus in the victim.
How to behave after lower jaw reduction?
If the doctor has successfully adjusted the lower jaw, the patient is recommended to wear a thick elastic bandage for 10 to 14 days, which will securely fix the bones.
During this time, you should stop eating solid food - it is better to concentrate on liquid soups, pureed cereals, fruits and berries. It is important not to overload the jaw with chewing load, so as not to provoke re-dislocation.
With successful reduction of the lower jaw after dislocation and a professionally performed operation, the prognosis for the patient is favorable. In some cases, jaw mobility may be impaired.
If you or your loved ones have a displacement of the lower jaw, contact dental specialists. Here, experienced doctors will help you with dislocations even in the most difficult cases.
Reviews
Regardless of the reason why subluxation of the jaw develops, the situation should under no circumstances be left to chance. The main thing is to contact the clinic in a timely manner.
If you have encountered this anomaly from your own experience, you can leave your comment in the appropriate section, and perhaps this will be extremely useful to someone.
If you find an error, please select a piece of text and press Ctrl+Enter.
Tags: jaw subluxation
Did you like the article? stay tuned
Previous article
What is dangerous about viral stomatitis in children and the subtleties of its treatment
Next article
Technological features of All on 4 implantation
Let's look at examples
Joint deformity can be caused by epilepsy, rheumatism, encephalopathy, arthritis or osteomyelitis. Displacement appears during sudden movements, if a person’s ligaments are weakened, with excessive opening of the mouth (excessive yawning, screaming, laughter), smoothing of the articular fossa (most often this is a congenital pathology) and, of course, due to mechanical injuries. The root causes include the presence of general joint disorders in people, possible disorders of the jaw structure (for example, the removal of one or more teeth), any types of pathologies that provoke the occurrence of seizures, improper food intake (pieces that are too large and hard).
Clinical manifestations
Symptoms depend on the type of dislocation. Common manifestations include:
- difficulty closing and opening the mouth;
- protrusion or distortion of the jaw forward;
- sharp pain radiating to the temple;
- profuse drooling;
- inability to pronounce words normally.
Treatment of habitual jaw dislocation should be carried out exclusively by a specialist. The only thing the patient can do is fix the position by bandaging his chin with a scarf. Painkillers and ice will help reduce pain.
On our website Dobrobut.com you can sign up for a consultation with the right specialist and undergo diagnostics if necessary.
Possible consequences
Having figured out how to straighten the jaw yourself, it is worth focusing on the fact that in most patients, at the time the procedure is completed, the jaw joint involuntarily closes. And if you do not have time to remove your fingers in time, you can get a new serious injury. All these actions bring the temporomandibular joint back to normal, but in some cases you shouldn’t even think about how to straighten your jaw at home.