Occlusion and bite
Why does a patient come to the orthodontist? That's right: straighten your teeth and correct your bite... We have already talked about this (see here)
But what a bite is and what it is eaten with (especially what is a regular and incorrect bite of teeth) the patient usually does not have the slightest idea. For another patient, for example, what the bite and what the taste is unambiguous. That’s how they formulate it: “We’re... about this at Vkus ... like straightening it out.” Many of my colleagues are not far behind them: out of ten dentists I interviewed from different specialties (orthodontists, orthopedists, surgeons, therapists), only four were able to more or less clearly formulate what a bite . And on the question (desire) to justify and clarify the meaning of the concepts of occlusion and occlusion, every single one floated. How...
But such concepts as bite and occlusion are key not only in orthodontics, but in dentistry in general. Therefore, together with you and my colleagues, I would like to speculate on this topic and finally decide on the concepts of what kind of bite this is (which sometimes you really want to correct). And what exactly is correct and incorrect bite?
Dental occlusion is any (any) closure of the teeth of the upper and lower jaws. The key word here (both in the concept of occlusion and in the concept of occlusion) is closure . If there is no closure, this is no longer an occlusion. This is disocclusion (its absence).
Depending on the position of the lower jaw (and as you and I know, it is mobile), several types of occlusion are distinguished: central , anterior , posterior and lateral .
a ) Central occlusion; b ) Posterior (distal) occlusion; c ) Anterior (sagittal) occlusion
Central occlusion (CO) is something of an ideal or template. In life and practice, the practically unattainable, or rather, often simply not achievable (for various reasons). It is generally accepted that CO is characterized by three (although later we will understand that it is far from three) main factors: dental , articular and muscular .
Well, with the dental factor everything is clear: the teeth must close together. And preferably not anyhow, but in a clear order. But I’ll tell you about this a little later, when we talk about bite . What about the other two factors? Let me explain.
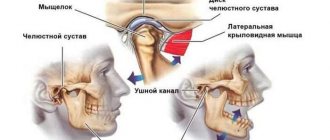
Joint factor CO (central occlusion). You and I know that the position of the lower jaw can be determined by the position of the articular heads of the temporomandibular joint (TMJ). Well, with central occlusion, the articular heads stand most evenly and correctly, reflecting the ideal position of the lower jaw relative to the upper jaw.
Let me remind you: the upper jaw, unlike the lower jaw, is practically motionless. It is tightly nailed (and in some cases screwed) to the skull. JOKE! We will have a separate conversation about fixing the upper jaw to the skull... Everything there is also very interesting and not so simple.
The ideally even placement of the articular heads of the lower jaw in the articular fossa of the temporal bone should be ensured by the most uniform and balanced work of certain muscles of the maxillofacial area. After all, it is the muscles that ensure the position of the lower jaw in space (in fact, like any other bone). Here you have the muscle factor .
I repeat once again - CO (central occlusion) is like a certain ideal that everyone seems to strive for, but getting it is something with something (does everyone, and does it always succeed?). Because just imagine how many confusing factors (and you can’t even imagine how many) are preventing you from achieving this ideal. Well, we'll talk about this later.
What about other types of occlusion? Everything is simpler here. He moved the jaw forward - anterior occlusion . Pushed it back (it's not that easy, right?) - you get posterior occlusion . The jaw is turned to the right and left (the only thing is that the teeth must be in contact) - this is lateral occlusion .
the
occlusion . What is a bite ?
“Bite is the closure of the teeth in the usual, static position of the lower jaw” (L.S. Persin)
Based on the very formulation of the concept of occlusion, its main feature is the closure of the teeth (occlusion) or the absence of their closure (disocclusion). And the connection to the position of the lower jaw (and it is this, as we have already said, that determines the type of occlusion), allows us to say that a bite is the closure of the teeth in the usual occlusion. Those. occlusion is a very special case of occlusion. And it turns out that it is purely individual.
Someone’s teeth may be perfectly straight and seem to fit together correctly (i.e., have the most multiple and dense contacts). Those. The bite is basically there. But the lower jaw (and the articular heads clearly show this) is shifted, for example, into lateral occlusion. And for a person this closure will be habitual (teeth close together better than ever). And it is this habitual closure that will be his bite. Individual. Which, by the way, due to the incorrect position of the lower jaw, it would be nice to correct it... Despite the possible complete “Hollywood” with teeth.
So it turns out that when the bite (the habitual closing of the teeth) coincides with the central position of the jaws (central occlusion), the bite is physiological. And with anomalies of occlusion, the usual position of the lower jaw does not coincide with the CO. And then the type of bite is determined by the position of the lower jaw, which is familiar to a person.
This is how a physiological bite is distinguished from an abnormal one .
The concepts of physiological occlusion and physiological occlusion are identical. In the case when there is a problem with the closure of the teeth, but their closure still takes place, we can talk about an malocclusion (occlusion). For example: distal occlusion, mesial occlusion, etc. Those. There is closure of the dentition, it’s just disturbed. When there is no closure of teeth at all, then they don’t talk about bite. In this case it simply does not exist. Just as there is no occlusion. Therefore, for example, it is wrong to diagnose “open bite.” If there is no bite, it means disocclusion.
Physiological occlusion has a number of signs:
Fig.1:
Fig. 1: The upper lateral teeth overlap the lower ones to the depth of the longitudinal fissure (b) , and in the anterior section the upper incisors overlap the lower ones by no more than 1/3 of the height of their crowns (a)
Fig.2:
Fig. 2 : Each tooth intersects with two antagonist teeth (a) . In addition to the lower central incisors and the upper last teeth (they have one antagonist each) (b)
Fig.3:
Fig. 3: Each upper tooth intersects with the lower and posterior lower teeth of the same name (a) . And each lower one has the same upper and front upper teeth (b)
Fig.4:
Fig. 4: The midline should pass between the central incisors
Fig.5:
Fig.5:
• On the upper jaw, the dental arch is larger in diameter than the alveolar arch, and the alveolar arch is larger than the basal (jaw)
• On the lower jaw it’s the opposite: the basal arch is the widest, then the alveolar, and the narrowest is the dental
Fig.6:
Fig. 6: The teeth of one jaw are in contact with each other pointwise, on approximal (lateral for incisors and canines, and anterior-posterior for premolars and molars) surfaces
Fig.7:
Fig. 7: The height of the tooth crowns decreases from the central incisors to the molars, with the exception of the canines. The upper teeth are inclined outward (vestibular), and the lower teeth are vertical
Fig.8:
Fig. 8: The first molars, with their mesial-buccal cusp, enter the intercuspal fissure of the lower molar of the same name
Now we understand what, what closure (as a result of treatment) we should strive for? Although this is just the “external” part of the occlusion (bite). And in the modern interpretation, occlusion (occlusion) is not only the teeth and their closure. Everything there is much deeper and more interesting. But we'll talk about this a little later...
There are also closure of baby teeth ( deciduous occlusion ), closure of permanent teeth ( permanent dentition ) and mixed occlusion (closing of teeth during the period of change of baby teeth to permanent ones).
Well, we seem to have determined the guidelines for the “correct” bite. Have you read it? Remember. Great. Now... forget it. Why? Yes, because the landmarks here are the teeth. Only teeth. And teeth are a very superficial and very unreliable guide. Dependent on many other guiding factors. This means that it is at least unreasonable to determine the “correctness” or “incorrectness” of a bite only by the closure of the teeth. This is unreliable. Not exactly. It is fraught with errors and problems, which we see almost every day.
Unfortunately, in the vast majority of cases, all orthodontic treatment is based on these “unsteady”, unreliable “purely dental” guidelines. Yes, not only orthodontic, but dental in general. Prosthetics, implantation, and dental restoration also rely on the teeth themselves. Only on the teeth. In fact, the goals and objectives of dental (and orthodontic, including) treatment very often boil down only to “attracting” teeth to each other. And a prosthetic device is inserted into the lung and implanted. Getting a certain external effect, the appearance of a “correct” bite, the illusion of successful treatment. And then comes the reckoning...
Expensive crowns and bridges break for no apparent reason. The implants fall out or become inflamed. And crooked teeth are corrected in the wrong direction. And with the temporomandibular joint, the problem suddenly pops up out of the blue. And this, by the way, is really a problem, since you won’t find specialists in TMJ during the day. No, of course there is a lot of advertising and show-off. Has anyone seen the results?
Or even more abruptly: problems of a different order begin, seemingly far from the teeth: the lower back aches, the head hurts, the pressure jumps, the body somehow reacts negatively to the weather... And endless trips to neurologists, neurologists, psychotherapists, osteopaths, and other “atams” begin ", "-istam", and "-ologam". Endless, because these specialists usually also see nothing except “their” sore.
And it is not known that these troubles, including the incorrect formulation of the concepts of occlusion and occlusion, are to blame. But naturally, it is the patient who pays for this “broken aim.” Not with money (or rather, not only with money). The main thing, and the saddest thing, is your health. And often without even realizing that the cause of many (oh, many) sores is an incorrect, and sometimes incorrectly corrected, bite. And why all? Yes, because the attitudes and dogmas on which modern dentistry exists have not changed, by and large, for a hundred and fifty years. And what then is the “modernity” of today’s dentistry? Only in the fruits of technological progress? It turns out to be some kind of “race in width”. You look at the topics of training seminars and it makes you feel sick. What are they talking about: “which braces are cooler...”, “which fillings are better...”, “which ceramics are more beautiful...”. And what? Just spend your life on this? Is it hard to dig deep?
And the very formulation of the concepts of occlusion and occlusion , as the main guidelines in dental treatment, is high time to change. Otherwise we will remain Neanderthals. Savages armed with modern equipment. Incapable, with all their “weapons”, of competent treatment, of real help.
Are you upset? Understand. But let's figure it out...
So let’s start right away with the formulation of the bite. Remember what it sounds like? “Closing of teeth in habitual occlusion.”
Closing teeth . Where do teeth come from? That's right - from the jaws . And if, say, the jaw is in the wrong position, or is deformed, will this affect the closure of the teeth or not? Of course yes.
And where does the jaw (let’s take the upper one) grow from? Let's remember the anatomy... That's right - it is attached to the skull . To the very base of the skull. And if the cranial bones are deformed, or are in the wrong position (displaced as a result of injury), can this be reflected in the position of the upper jaw? Maybe. And therefore, such a displacement will also affect the closure of the teeth (bite). How interesting, right?
What about the lower jaw? In general, it also seems to be “attached” to the skull. Through the temporomandibular joint (TMJ). And an integral part of the joint is the temporal bone (skull bone!!!). More precisely, its articular fossa. And if the temporal bone is, for example, in some kind of external rotation (and this is quite common), do you think this will have any negative consequences for the lower jaw and lower teeth (and further for occlusion)? And there is no need to think - the answer is obvious.
In addition, the lower jaw (its position) is directly dependent on the position of the upper jaw. The dependence is approximately the same as a door depends on the door jamb: the jamb is smooth and the door does not creak. And it opens normally. And the jamb is crooked - and the door is also incorrectly positioned, which leads to problems with its opening and closing...
And it’s the same with the jaws: if the upper jaw is deformed or incorrectly positioned in space (by itself or due to “distortions” of the cranial bones), then the lower jaw is forced to adapt to the “wrong” upper jaw. And how is the adjustment (forced position) ultimately ensured and carried out? Yes, the teeth are compensatory and incorrectly positioned. Here you go: get the wrong bite.
Go ahead. And what does the skull “contact” with anatomically? That's right - with the spine. This means that any problem with posture (scoliosis of some kind) will immediately cause a compensatory restructuring of the bones of the skull. And with them the upper jaw. And then, as in the fairy tale about the turnip: the spine bent - the skull “moved” - followed by the upper jaw, followed by the lower jaw. Plus, the dentition is compensatory deformed... (read the mechanism above). The “exit” is, again, the problem of teeth closing.
One thing needs to be understood: teeth are part of the skeleton . And the skeleton is a closed kinematic system. Everything in it is built on compensation (to maintain balance). And we still treat flat feet separately. Separately, we “correct” the posture. And we are separately trying to solve the problem of teeth closing (occlusion). And we are also surprised when something “not very good” comes out.
Or on the other hand... Imagine if you thoughtlessly “correct your bite” and “straighten” your teeth. As many people think, put on braces and wear them for a year and a half. That's all. Happiness will arrive. And the fact that by “correcting” the bite we have “corked” all the skeletal distortions (unaccounted for), as if with a cork – how is that? What then is the treatment? And how (what problem) will the patient pay for straight teeth?
Even a hedgehog has long understood that the closure of teeth depends on many “non-dental” factors. And that the bite is not just teeth. That is why there is a need (long overdue) to expand our understanding of what occlusion and dental occlusion . And give a more precise formulation of these concepts.
READ CONTINUED…
Sign up for diagnostics
Social Like
Comments for the site
Cackl e
This method was developed by I.P. Pavlov - the method of conditioned reflexes, with the help of which he expanded the reflex theory, showing that the most complex and advanced forms of behavior are carried out on the basis of conditioned reflex activity.
Reflexes can be classified according to various indicators. According to their biological significance, reflexes are divided into orientational, defensive, food and sexual. According to the location of the receptors, they are divided into exteroceptive - caused by irritation of receptors located on the outer surface of the body; interoreceptive - caused by irritation of receptors of internal organs and blood vessels; proprioceptive - arising from irritation of receptors located in muscles, tendons and ligaments. Depending on the organs that are involved in the formation of the response, reflexes can be motor (locomotor), secretory, vascular, etc. Depending on which parts of the brain are necessary for the implementation of this reflex, they are distinguished: spinal reflexes, for which spinal neurons are sufficient brain; bulbar (arising with the participation of the medulla oblongata); mesencephalic (neurons of the midbrain are involved); diencephalic (neurons - diencephalon); cortical (which require neurons of the cerebral cortex). It should be noted that in most reflex acts both the higher department of the central nervous system - the cerebral cortex - and the lower departments are involved simultaneously.
Reflexes can also be divided into unconditioned (innate) and conditioned (acquired during individual life).
The structural basis of the reflex, its material substrate, is the reflex arc - a neural chain along which a nerve impulse passes from the receptor to the executive organ (muscle, gland).
The reflex arc includes:
1. receptor that perceives irritation;
2. sensitive (afferent) fiber (axon of a sensitive neuron), along which excitation is transmitted to the central nervous system;
3. nerve center, which includes one or more interneurons;
4. efferent nerve fiber (axon of the efferent neuron), along which excitation is directed to the organ.
A reflex reaction always involves afferent neurons that transmit impulses from receptors (for example, proprioceptors) of the executive organ to the central nervous system. With the help of reverse afferentation, the response is corrected by the nerve centers that regulate this function. Therefore, the concept of a “reflex arc” is currently being replaced by the concept of a reflex ring, since functionally the arc is closed both at the periphery and in the center by nerve signals continuously circulating during the operation of the organ.
The simplest reflex arc (monosynaptic) consists of two neurons: sensory and motor. An example of such a reflex is the knee reflex. Most reflexes involve one or more sequentially connected interneurons and are called polysynaptic. The most elementary polysynaptic arc is the three-neuron reflex arc, consisting of sensory, intercalary and efferent neurons. The implementation of food, respiratory, and vasomotor reflexes involves neurons located at different levels - in the spinal cord, medulla oblongata, midbrain, diencephalon, and cerebral cortex.
Reflexes arise under the influence of stimuli specific to them that act on their receptive field. The receptive field of a reflex is an area of the body containing receptors, the irritation of which always causes a given reflex reaction. Thus, the pupil constriction reflex occurs when the retina of the eye is illuminated, extension of the lower leg occurs when a light blow is applied to the tendon below the knee, etc.
Nerve centers
A nerve center is a functional association of neurons that ensures the implementation of a reflex or the regulation of a specific function. The neurons included in the nerve center are usually located in one part of the central nervous system, but can be located in several. The breathing center is located in the middle third of the medulla oblongata, the urination center is in the sacral, and the knee reflex center is in the lumbar spinal cord. As a rule, not one, but many centers located in different parts of the brain, including its higher parts, take part in the implementation of complex reflexes of the whole organism. For example, the act of breathing involves not only the breathing center in the medulla oblongata, but also the nerve cells of the pons, cerebral cortex and motor neurons of the spinal cord.
Features of the spread of excitation in the central nervous system are mainly determined by the properties of nerve centers:
1. Unilateral conduction of excitation . In the central nervous system, excitation can spread only in one direction: from the receptor neuron through the intercalary neuron to the efferent neuron, which is due to the presence of synapses.
2. Slower conduction of excitation compared to nerve fibers . The time interval from the moment of application of stimulation to the receptor to the response of the executive organ is called reflex time. Most of it is spent on conducting excitation in nerve centers, where excitation passes through synapses. The release and diffusion of the transmitter in the synapse requires a time period of 1.5–2 ms (synoptic delay). The more neurons in the reflex arc, the longer the reflex time.
3. Summation of excitations (or inhibitions). Nerve centers can sum up afferent impulses, which manifests itself in an increase in the reflex with an increase in the frequency of stimulation or the number of irritated receptors. There are two types of summation: temporary summation - if impulses arrive at the neuron along the same path through one synapse with a short interval, then the EPSP is summed up on the postsyaptic membrane and it depolarizes to a level sufficient to generate an AP; spatial summation is associated with the summation of EPSPs arising simultaneously at different synapses of the same neuron. Both types of summation occur in the region of the axon hillock, where AP is generated.
4. Convergence . In a nerve center, several cells can transmit impulses to one neuron, i.e., excitations converge on it. Convergence may result from the arrival of excitatory or inhibitory inputs from different sources. Thus, motor neurons of the spinal cord can receive impulses: from peripheral nerve fibers entering the spinal cord; fibers connecting segments of the spinal cord; corticospinal fibers from the cerebral cortex; inhibitory pathways from the reticular formation. As a result of convergence, impulses from these sources are summed up and a response arises, which is the total effect of heterogeneous information.
5. Divergence and irradiation . Excitation of even a single nerve fiber through which impulses enter the nerve center can cause excitation of many nerve fibers emerging from the center. The morphological substrate for the wide distribution of excitation impulses (irradiation) is the branching of axons and the presence of a large number of interneurons within the center.
6. Relief and occlusion . Not only the fibers of their own afferent inputs terminate on the neurons of the nerve centers. Each of them receives branches from afferents of the neighboring center, which can cause the development of occlusion (blockage) or, conversely, relief.
The phenomenon of occlusion is that the number of excited neurons with simultaneous stimulation of the afferent inputs of both nerve centers is less than the arithmetic sum of excited neurons with separate stimulation of each afferent input separately. The phenomenon of occlusion leads to a decrease in the strength of the total response. The phenomenon of central relief is characterized by the opposite effect. Facilitation is based on clearing the path - the spread of excitation not along the chain of neurons through which information did not arrive previously, but through neurons that have already been facilitated by the first irritation.
Treatment of occlusal pathology or when the problem is not in the bite
The application of fundamental occlusal concepts in practice is possible only with an objective assessment by the doctor of the patient’s problems with bite and temporomandibular joint, and determination of which of the constituent structures of the dentofacial apparatus requires the greatest therapeutic attention. Typically, patients with masticatory muscle pain are advised to use full or partial appliances with a modified bite plane. But it is equally important to understand when and why to use certain devices for the correction of occlusal-associated disorders. In this article we will describe the methodology for analyzing certain aspects of occlusal pathology, and possible options for correcting them through different therapeutic approaches.
Introductory Occlusion Concepts
When applying occlusal concepts in prosthetic and restorative dentistry, it is important to clearly understand the difference between centric occlusion and the position of maximum fissure-tubercle contact (maximum intercuspidation). When moving from one jaw position to another, the doctor can identify the so-called guide tooth. This tooth is a reference point for the entire jaw, as it determines its movement into central occlusion. If during the intervention this tooth is somehow changed through restoration, global occlusal disturbances develop, which are quite difficult to correct. In dental practice, it is not recommended to carry out any correction of the guide tooth, except in cases where such intervention is therapeutically necessary and justified.
Determination of Central Ratio
The centric relation represents the most superior and anterior position of the joint in the glenoid fossa. This concept should not be confused with central occlusion, maximum intercuspidation, adaptive central position, centric slides (shifts) and centric stopping points. The Glossary of Orthopedic Terms defines centric relation as the relationship of the maxilla and mandible in which the articular heads articulate opposite the thinnest and most avascular part of the articular disc in an anterosuperior position just on the slope of the articular eminence. This position does not depend on the closure of the teeth, and is specific to the joint. Frank Spear states that the centric relation is formed in a position of the articular head in which the lateral pterygoid muscles relax and the muscles that elevate the mandible contract, while ensuring adequate position of the disc between the structural elements of the joint. The muscles ensure alignment of the entire dentofacial apparatus in an intact state and in the absence of joint pathologies. Essentially, the centric relation is a self-centering position. An example would be the position of a marble in a cup: in the end it will still end up exactly in the center of the cup. If the lateral pterygoid muscle is inflamed, the joint will not be able to occupy the centric relation position. This is the same as acting on a metal ball in a cup with a magnet - it will begin to change the position of the ball from side to side. The same thing happens to the masticatory apparatus when the muscles are damaged.
Registration of centric relation
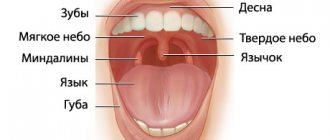
Registration of the central ratio can be carried out using several methods. The simplest of these (but at the same time the least accurate) is to ask the patient to touch the back of the roof of the mouth with his tongue, and try to bite. In this situation, the jaw should independently take the position of the central relationship. The second method of recording centric relation is bimanual jaw orientation, which is very sensitive to perform. You need to create a “C” shape with your hand: place all fingers except the thumb on the body of the jaw and chin, and the thumb on the branch of the jaw. In this case, you need to ask the patient to carefully open and close his jaw so that he gets used to this movement. After several cycles of repetitions, the doctor should ask the patient to relax and activate the masticatory muscles with the same movement that the patient himself previously performed. In this case, it is important not to “push” the articular process too posteriorly, but to carefully center it in the anteromedial and superomedial position. The third method is to use an anterior deprogrammer. Instruments such as Lucia jig or quicksplint are placed in the oral cavity along with impression material to register the bite. The deprogramming device is fixed on the central incisors. The patient begins to move the jaw back and forth along the plane of the jig to relax the muscles. After the muscles have relaxed, the patient should bite down on the flat surface of the deprogrammer with the jaw in a posterior position. In this case, the articular head occupies a certain position in the fossa. For the same purpose, you can use a sheet calibrator, which performs the same function as the front deprogrammer. Using a sheet calibrator, teeth can be separated to different heights depending on the number of sheets used. Whether it is possible to detail the jaw with a sheet calibrator is a controversial issue, but at a minimum, this tool will guide the dentist in the right direction. If the joint is completely intact, then it is logical that when using a sheet calibrator, the muscles self-center the articular head in the desired direction. A well-fitting bite guard can also help determine the centric relation. After recording the centric relation, it is necessary to identify the point of first contact. This could be a guide tooth. But not all patients have a functional guide tooth. Photo 1 shows teeth 2 and 3 and the point of first contact on the mesiolingual cusp of tooth 2, as evidenced by the clearest imprint of the articulation paper. You can also note the presence of a small mark on the distal cusp of the 3rd tooth. When the jaw is positioned in centric relation, the point of first contact or points of first contact form the so-called central occlusion. Thus, the centric relation is the position of the joint and does not depend on the contact of the teeth. When centering the joint, the teeth may not touch at all. If the antagonist teeth somehow contact in the position of the central relationship, then this relationship is called central occlusion.
Photo 1. Registration of points of first contact.
Determination of central occlusion
The term “maximum intercuspidation” is used to define the habitual dentition in which the patient has the maximum number of antagonist teeth in contact. Central occlusion can be determined during bimanual orientation (Figure 2), or using a sheet calibrator (Figure 3).
Photo 2. Bimanual manipulation and mandibular guide.
Photo 3. Sheet calibrator.
The position of central occlusion may or may not coincide with the position of maximum intercuspidation. If the dentist decides to carry out restoration in the area of the formation of the first contact between the teeth, then he needs to determine the presence or absence of a slide between the position of maximum fissure-tubercle contact and central occlusion. The author in his practice uses the following method for this: you need to ask the patient to close the jaws together as tightly as possible in the position of maximum intercuspidation, after which it will immediately become clear whether the jaw is moving from this position or not. Before determining the presence of a slide, the doctor needs to clarify the parameters of the vertical and horizontal overlap, which can be done using a periodontal probe. If changes in horizontal overlap are greater than vertical overlap, the clinician should pay special attention to the patient's entire treatment protocol (Figure 4).
Photo 4. Assessment of changes in the parameters of vertical and horizontal overlap.
For patients with a slide in central occlusion, changes in the parameters of the vertical overlap are more pronounced than in the horizontal position. The slide in most patients is directed to the left, right, or forward or backward. A slide of more than 1.5-2.0 mm in a predominantly horizontal direction, compared to the vertical, indicates the presence of functional problems, which very often can affect the guide tooth. The very concept of a guide tooth is used because its presence determines stability in the relationship of the jaws and the implementation of normal occlusal function. With any restoration of the guide tooth, unforeseen general occlusal changes may follow. The only way to foresee the consequences of interventions on the guide tooth is to compare the jaws in centric relation and analyze how the bite changes after eliminating contact in the area of the guide unit of the dentition. Due to the unique parameters of physiology, as soon as the pattern of how the bite was formed along the guide tooth, which, in fact, maintained the entire system in a stable state, is removed from the functional memory, then, in addition to changes in the relationship of the teeth, changes in the work immediately begin to develop chewing muscles. If such violations are repeated and not corrected in time, conditions may arise in which the patient will never again be able to achieve the original state of occlusion. Therefore, tooth preparation should be carried out only after the doctor has determined the role of each individual tooth in the formation of occlusal relationships. If, after checking the models in the articulator, there is a redistribution of contact points, or a change in the relationship of the jaws as a whole, then you need to think about whether the chosen treatment method is worth the possible risk of developing occlusal complications. Today it is impossible to predict how much the human dentofacial apparatus can adapt to certain changes in the occlusal scheme, but it is obvious that the range of compensation is limited, so it should be treated with great caution.
Perform a thorough diagnosis before starting treatment
Before starting any iatrogenic interventions, the initial state of the occlusal scheme and other functional parameters of the patient’s dentofacial apparatus should be assessed. Thus, the dentist must conduct a thorough diagnosis of the muscles, joint, dentition and occlusal relationships in general, and only then begin treatment. The purpose of such a diagnosis is to identify patients at risk for whom orthopedic treatment can provoke a number of subsequent iatrogenically caused occlusal complications. The doctor should carefully analyze the patient's general and dental health history, identifying the presence or absence of symptoms of snoring, obstructive sleep apnea, gastroesophageal reflux disease, antidepressant use, headaches, injuries or pain in the face and jaws. Patients with obstructive sleep apnea may not be aware that they have this pathology, so to diagnose it, the doctor may use the Epworth rating scale or similar diagnostic algorithms that assess the risk of changes in sleep physiology.
Control over the level of invasiveness of iatrogenic interventions
After collecting anamnesis and analyzing clinical signs, the further process of treatment planning becomes more reasoned. The doctor should definitely ask the patient about his subjective opinion about the existing state of occlusion; perhaps the patient himself notes symptoms of abrasion or clenching. The patient interview should range from collecting less personal details to more personal complaints. The dentist must also check the condition of the eight muscles of mastication. Four of them are quite easy to diagnose (masseter muscle, temporalis muscle, medial pterygoid muscle and lateral pterygoid muscle) (photo 5-7).
Photo 5. Chewing muscle.
Photo 6. Temporalis muscle.
Photo 7. Medial and lateral pterygoid muscles.
The digressor, sternocleidomastoid, trapezius and splenius capitis muscles can, of course, also provoke occlusion and joint problems, but their diagnosis is not necessary before a diagnosis of temporomandibular joint dysfunction is made. First you need to palpate the masseter muscle with moderate pressure. By carefully checking all areas of the muscle, the dentist can determine which area is experiencing the most severe pain. The temporalis muscle is also diagnosed using the same method. Both pterygoid muscles are palpated through the oral cavity, but this procedure is somewhat difficult. It is easier to assess the function of the pterygoid muscles by asking the patient to stick the jaw forward while pressing posteriorly on it in the chin area. The dentist can also diagnose muscle function by placing his fingers on them and asking the patient to move the jaw in the desired direction.
Joint noises and TMJ range of motion
It is extremely important to obtain information about the range of motion in the joint, and possible noises that the patient may notice in its structure during function. Palpation of the joint occurs by placing the dentist's fingers on the lateral side in the projection of the head, after which the doctor asks the patient to open and close his mouth. The doctor may also apply 3 to 5 pounds of gentle pressure to the joint to determine if it may cause any pain. When applying pressure, the fingers can be placed slightly behind the projection of the initial position of the joint head, and the pressure itself can be applied in the direction opposite to the main directions of movements of the head. If the patient notes pain during the diagnosis, the doctor asks him to rate these sensations on a point scale. The range of motion of the joint is determined using a ruler, triangle, or other specially designed tool. Range of motion should be assessed in closed and open mouth positions (depending on the presence of an open or deep bite). The physician should also evaluate the range of lateral movements of the jaw and determine whether there are any functional limitations.
Joint stress tests
After assessing all of the above parameters, the patient's overall occlusion status, centric relation, and centric occlusion should be assessed. Load tests allow you to determine how much a joint can compensate for applied forces. These diagnostic procedures are carried out using a leaf calibrator, after biting on which the patient is asked to move the jaw back and forth. If it is painful for the patient to move the jaw forward, then there are no problems with the load on the joint, but there are problems associated with the work of the muscles and the intactness of the tissues located behind the joint disc. After this, the patient moves his jaw back and bites - the presence or absence of pain indicates how much the disc is displaced. The dentist can determine whether the patient has only lateral disc displacement, or whether there is also medial displacement, which is more difficult to treat. After diagnosing the joint through stress tests, the doctor evaluates for signs of pathological abrasion, fremitus and chipping of hard tissues in the patient’s mouth. Diagnosis of occlusion involves identifying the point of first contact and all existing occlusal interferences. If the doctor accurately determines the nature of occlusal excursions, it will be easier for him to establish the cause of the development of pathological abrasion, fremitus and existing chips of enamel and dentin. The presence of occlusal interference is established using articulation paper of two colors. First, the dentist uses thinner paper and asks the patient to move the jaw left, right, forward, backward, just chew the paper, try to bite it, and move the jaw to the maximum amplitude. Clenchers will have limited range in all of the above jaw movements. After the doctor has recorded the nature of the excursion movements of the jaw using thin occlusal paper, he takes thicker, dark-colored occlusal paper and asks the patient to close the jaws firmly and several times in the position of maximum fissure-tubercle contact. Thus, the doctor is able to compare the position of occlusal interference with the position of the points of interdental contact in the most comfortable position for the patient. However, this stage of diagnosis in no way allows us to identify occlusal problems associated with joint disorders. The above-described manipulation can be optimized through the use of T-scan technology.
Disc examination and treatment methods
The gold standard for diagnosing the condition of the disc remains the magnetic resonance imaging (MRI) method, which allows you to record the condition of the disc in various positions. Also, the doctor can obtain certain information about the condition of the disc using conventional dental tomography, but the capabilities of the latter in this aspect are quite limited. Given that MRI is not a routine or commonly used examination method, the doctor often has to diagnose the disc through a routine clinical examination. The doctor must carefully listen to the noise in the structure of the joint when the patient opens and closes the mouth, and also carefully palpate the area of interest. Visually, you can detect the presence of deviations or deviations during various movements of the jaw. Deviations indicate displacements of the disc from the side to the center: first to the left or right, and then again to the middle. Deviations (deflections) indicate displacement of the disc to one side or the other, with its retention in a changed position. Listening to the joint can be done with a stethoscope, which allows you to identify the presence of sudden changes in its position by sound. Doppler ultrasound of the joint area can also be performed. The Doppler effect allows audio noises from outside to be transmitted so that the patient can also hear them. In this case, of course, you have to deal with a lubricating gel, which spreads over the study area, but provides better signal conductivity. Another diagnostic option is to perform joint vibration analysis (JVA). ABC is carried out using a small microphone that is attached to the headphones in the joint area. For comparison, they use the already existing library of noises and sounds of the joint, which are characteristic of the normal state. This diagnostic method is quite expensive, but is extremely necessary in cases of verification of initial joint-associated disorders.
Determining the condition of the joint
The condition of the joint before treatment can be classified according to the scale proposed by Dr. Piper. Stage I of the joint condition indicates its normal function, stage II indicates a loose state of the ligament (weakness of the ligament, it becomes like chewing gum - it can stretch and remain deformed, causing the development of noise), stage III indicates a displacement of the lateral pole of the disc (as as a rule, pain is observed after some recent incident, but often pain as a symptom may be absent), stage IV - about medial displacement of the disc (acute or chronic), stage V - about tissue changes in the retrodiscal space (acute or chronic perforation). To classify the joint condition according to the system described above, it is necessary to clearly understand the patient's existing joint position.
Devices for the treatment of muscle pain
The success of treating muscle pain depends on the design of the device, which the doctor chooses for the appropriate purpose. Based on the possible purpose of treatment, you need to understand which device can help most effectively in each individual clinical case. If, for example, a patient shows signs of pathological tooth wear and the condition of the joint is classified as healthy, a regular mouth guard can be used to prevent the effects of excessive occlusal forces. Night guards that are used by doctors to treat muscle pain are called splints or orthopedic splints. Splints are used to change the position of the jaw in space, and thus change the direction of the acting forces.
Full overlap tires
If a patient develops pain due to disc displacement, then it is logical that the designs of splints used for such purposes should differ from mouthguards that are used to prevent consequences in bruxists. Classic splint designs are rigid splints with full coverage of the teeth. These splints protect teeth and can reduce pain. They can also be used to assess the severity of clenching and bruxism. Rigid classic mouthguards are quite simple and quick to manufacture, but their use should be avoided in most clinical cases with disc displacement. Softer versions of hard full-coverage splints, in addition to protecting teeth, also serve to stabilize the joint, relax muscles, and help the doctor determine the centric relation. If the patient has muscle soreness without disc displacement and it is difficult for the clinician to clinically record the position of the centric relation, a classic rigid splint can be used to make this task easier. In addition, rigid, full-coverage splints reduce and optimize stress on the joint ligaments. However, it is worth remembering that there is simply no single bus to solve all clinical problems. The Pankey/Dawson splint is a lower jaw splint with a flat plane without any changes in inclination, which avoids posterior displacement of the disc and joint. The Michigan Anterior Guide Plane Splint is a rigid acrylic splint that covers the anterior teeth of the upper jaw. The purpose of using this mouthguard is to limit contact in distal areas. The Tanner splint allows the occlusion to be slightly opened in the vertical direction while maintaining joint and disc positions in which the muscles relax. In this way, the condition of the joint can be identified for further diagnosis.
Hybrid tires
Hybrid splints can be used for many purposes, sometimes even requiring the patient to wear several of them at the same time. The anterior bite plane is used by many clinicians because it is relatively simple to recreate, easy to modify, and can be used in many clinical settings. When the anterior bite plane is combined with a lingual ramp behind the teeth, the Farrar appliance is created, which is used to treat patients with existing obstructive sleep apnea. This device does not cause distalization of the joint, it provides retention of a certain vertical position and prevents posterior displacement of the jaw, since it is held by the lingual ramp. The use of Gelb-type distal onlays allows you to create only distal occlusion. They are quite effective in many cases, but they should not be worn for more than 12 hours a day and for no more than 3 months at a time, as this may cause the development of an anterior open bite. The Hawley front stopper is widely recommended by Dr. Kois. The Kois splint is used for equilibration of occlusion with further restoration interventions. This tire can also be used as a guide, eliminating the need to reuse the sheet calibrator. The doctor asks the patient to bite on the splint, and after a while removes it from the mouth. The dentist then begins to determine the desired positions of the distal stoppers until complete balance is achieved. The disadvantage of any equilibration procedure is that it can provoke an underestimation of the vertical parameters of the bite, which can be detrimental to the joint. Nociceptive inhibition of the trigeminal nerve can also be performed using a splint with an anterior bite plane. Hybrid types of mouth guards should not be used 24 hours a day. This is especially true for distal linings, which can provoke changes in the bite. If the risk of changes in bite as a result of using a splint is very high, the dentist should conduct a preliminary conversation with the patient, explaining to him all the possible negative consequences of splint therapy. The primary goal of using all hybrid tires is to resolve or at least alleviate pain.
Important steps in choosing a mouth guard
If the initial diagnosis is correct, the choice of one or another mouthguard design is etiologically or pathologically justified. To adequately fit the mouthguard in the oral cavity and modify it, the doctor will need several burs, polishing systems, rubber bands of different colors and, most importantly, knowledge. Before placing the mouthguard, you should thoroughly dry your teeth. After this, using articulating paper of different colors, the doctor begins to fit the mouthguard, identifying those areas that prevent an ideal fit. According to the experience of the author of this article, it is best to first check the mouthguards in the articulator, and only then transfer them to the oral cavity. When planting, you should carefully check the accuracy and depth of the structure on both sides, since biting on one of them can cause an overall imbalance and the development of subjective discomfort in the patient. Registration of all displacements of structures using articulating paper will allow us to level out the areas of the most significant interference. Typically, red articulation paper is tested to analyze the fit of the aligner on both sides, while blue articulation paper is tested to ensure vertical adequacy. Correction of the mouthguard design is carried out using burs of different shapes.
When bite is not a problem
Recently, the topic of sleep bruxism has become increasingly widespread in the dental community. In 2005, the American Academy of Sleep Medicine (AASM) defined sleep-associated bruxism as a sleep-related motor disorder that is similar to restless leg syndrome or oral parafunctional activity. As a rule, such disorders are associated with awakenings during sleep. The current definition of sleep bruxism suggests the following formulation: “repetitive activity of the masticatory muscles, characterized by clenching of the jaws or abrasion of teeth and/or protrusion or other movements of the lower jaw.” A 2014 study by Hosoya et al found a correlation between obstructive sleep apnea and severe sleep bruxism pathology. This argues for the need to diagnose dental patients for the presence of risk factors associated with the development of sleep bruxism pathology. If possible, the patient should be examined by a sleep specialist, who can ultimately help the dentist make the correct diagnosis. Patients with sleep bruxism are also characterized by the presence of symptoms of dental hypersensitivity, a raised appearance of the tongue, dysfunction of the dentofacial apparatus, pain in the masticatory muscles and the presence of noise or clicking in the joint structure. Patients with sleep apnea tend to appear tired and snore while sleeping.
Conclusion
Patients with symptoms of malocclusion, changes in joint structure, and muscle pain should always undergo a comprehensive dental diagnosis to determine the underlying cause of the development of functional pathology. Understanding the concepts of guide tooth, muscle adaptation, sleep bruxism is part of the clinical practice of the dentist, which he should take into account when appropriate signs are present in individual clinical cases. Every dentist should, at a minimum, be proficient in recording centric relation, centric occlusion, assessing muscle function, verifying joint range of motion, and articular head and articular disc displacement. Information obtained during a thorough diagnosis of the patient, taking into account a previously collected anamnesis and the results of preliminary treatment, will determine whether the patient is at risk for developing potential complications after appropriate restorative manipulations. A clinical examination involves an analytical analysis of the condition of the dentofacial apparatus from the outside inwards with a detailed assessment of the function of the masticatory, lateral and medial pterygoid and temporal muscles. Load tests allow you to evaluate the condition of the joint and select the most appropriate mouth guard design to resolve the patient's symptoms. It is also important to determine whether the patient has sleep bruxism, which is often the cause of the development of the patient’s occlusal disorders. Taking into account and implementing all the above principles in the clinical practice of a dentist will optimize the success of the chosen method of complex rehabilitation, improving the quality of dental care for patients with occlusal dysfunctions in general.
Posted by Scott Cairns, DDS
Relief and occlusion.
Spatial summation. This phenomenon, which results in an increase in signal strength, is transmitted by involving an increasing number of sensory fibers in its transmission. The set of such receptors, formed by one pain fiber, often covers an area of skin up to 5 cm in diameter. This area is called the receptive field of this fiber. The number of endings in the center of the field is large, but decreases towards the periphery. The branches of different pain fibers partially overlap in space, so a pin prick of the skin usually simultaneously stimulates the endings of many fibers. Since the number of free endings of an individual pain fiber in the middle of its receptor field is much greater than in the periphery, a pinprick in the center of the field stimulates this fiber to a much greater extent than the same pinprick in the periphery.
Temporal summation. The second way to transmit signals of increasing strength is to increase the frequency of nerve impulses in each fiber, which is called temporal summation.
Temporal and spatial facilitation (or summation) is of great importance in coordinating processes in the central nervous system. Temporary relief is manifested by an increase in neuronal excitability during successive EPSPs as a result of rhythmic stimulation of the neuron. This is because EPSP durations last longer than the axon's refractory period. Spatial facilitation in the nerve center is observed with simultaneous stimulation of, for example, two axons. With separate stimulation of each axon, subthreshold EPSPs arise in a certain group of neurons in the nerve center. The joint stimulation of these axons produces a larger number of neurons with suprathreshold excitation (an AP occurs).
Briefly: Temporal and spatial facilitation is an increase in the reflex response when exposed to a series of sequential stimuli or their simultaneous impact on several receptive fields. Explained by the phenomenon of summation in nerve centers .
The opposite of relief in the central nervous system is the phenomenon of occlusion. Occlusion is the interaction of two excitation streams with each other. Occlusion was first described by C. Sherrington. The essence of occlusion lies in the mutual inhibition of reflex reactions, in which the total effect is significantly less than the sum of the interacting reactions. According to C. Sherrington, the phenomenon of occlusion is explained by the overlap of synaptic fields formed by the afferent links of interacting reactions. In this regard, when two afferent messages arrive, the EPSP is caused by each of them partly in the same motor neurons of the spinal cord. Occlusion is used in electrophysiological experiments to determine the common link between two impulse paths.
Briefly: Occlusion is the opposite phenomenon of relief. When the reflex response to two or more suprathreshold stimuli is less than the responses to their separate effects. It is associated with the convergence of several excitatory impulses on one neuron.
Once again: Central relief is explained by the structural features of the nerve center. Each afferent fiber, entering the nerve center, innervates a certain number of nerve cells . These neurons are the neural pool . Each nerve center has many pools. Each neuron pool has 2 zones: central (here the afferent fiber above each neuron forms a sufficient number of synapses for excitation), peripheral or marginal border (here the number of synapses is not enough for excitation). When stimulated, neurons in the central zone are excited. Central facilitation: with simultaneous stimulation of 2 afferent neurons, the response may be greater than the arithmetic sum of stimulation of each of them , since impulses from them go to the same neurons in the peripheral zone.
Occlusion - with simultaneous stimulation of 2 afferent neurons, the response may be less than the arithmetic sum of stimulation of each of them . Mechanism: impulses converge to the same neurons in the central zone. The occurrence of occlusion or central relief depends on the strength and frequency of stimulation. Under the influence of an optimal stimulus (the maximum stimulus (in strength and frequency) that causes the maximum response), central relief appears. When exposed to a pessimal stimulus (with strength and frequency causing a decrease in response), the phenomenon of occlusion occurs.
The property of facilitating the conduction and occlusion of a nerve impulse is the result of the convergence (convergence) of nerve impulses from different axons to one nerve cell. To generate a nerve impulse, the excitation reaching the nerve cell along the process of one axon may not be enough. In this case, excitation from another axon arriving at the same nerve cell facilitates the generation of a nerve impulse.
Several axons can approach a nerve cell, and each of them individually can cause excitation. When they are simultaneously excited, some signals sent to the nerve cell become blocked and cannot reach the effector apparatus. Of course, this is only a general diagram of the possible interaction of excitations coming from different nerve conductors to one nerve cell. In reality, when the excitatory or inhibitory influences of hundreds and thousands of nerve processes converge on one cell, summation and occlusion become purely statistical phenomena.