Tooth nerve and indications for its removal
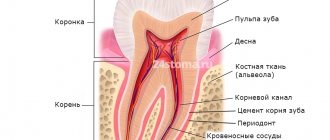
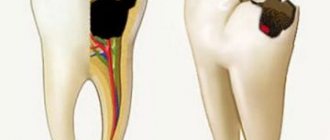
The dental nerve is its main organ, located at the root - the pulp. It is a system of blood vessels and is responsible for the reaction to stimuli. When it is completely removed, the tooth is considered “dead” because its blood supply is cut off. As a result, the enamel darkens, the tooth loses its resistance to irritants and quickly collapses. If, as a result of caries, the dental nerve is damaged - pulpitis - the question arises of complete or partial amputation of the pulp. When pulpitis progresses to the stage of periodontitis, removal becomes inevitable. Indications for removal also include destruction of bone tissue, a wide area affected by caries, persistent toothache.
Consequences of nerve removal
In the first 1–2 days after treatment, the tooth may hurt, but the intensity of the pain gradually decreases. To alleviate the condition, you can take analgesics recommended by a specialist. There are no other consequences of nerve removal.
Since pulpitis is most often caused by caries, during the treatment process the dentist removes the affected crown tissue. Restoring the integrity of the tooth is performed after removing the temporary filling. For correction, a filling material that does not contain toxic substances is used. In some cases, when the area of the carious cavity is too large and there is a risk of the filling falling out, it is recommended to install prostheses (stump or artificial crown.
Many parents mistakenly believe that depulpation implies the absence of a nerve in a permanent tooth. However, this is not at all true. Temporary and permanent teeth have separate systems and tissues that are not interconnected.
Martinka Children's and Adolescent Dentistry treats pulpitis by removing the nerve. Timely and correctly performed removal of the nerve of a baby tooth has no consequences. The integrity of the tooth is restored, and its functionality is preserved.
Removing dental nerve using arsenic
Previously, dental nerve amputation procedures were performed using arsenic. The root canal was enlarged using a drill, then arsenic was applied to the pulp and closed with a temporary filling to “kill” the nerve. The process took 2 days and was accompanied by pain, which could not be suppressed even with the help of analgesics. After the expiration of the period, the temporary filling had to be removed, the nerve removed and the root canal cleaned. The whole procedure was very painful and lengthy, requiring visits to the doctor several times. The main disadvantage of this method is the use of arsenic, known for its strong toxic properties. Both the doctor and the patient had to be extremely careful when using this substance in treatment, because if arsenic remained in a person’s tooth for longer than the permitted period, this led to tissue destruction and even tooth loss. For these reasons, today arsenic is no longer used in medical practice, but new techniques for amputating the nerve of a tooth are being successfully introduced.
What is arsenic used for in dentistry?
Doctors in our clinic always provide comfortable conditions for their patients. We try to make procedures less painful and faster, using various modern techniques and painkillers. But, if the situation with a bad tooth has been severely neglected, doctors have to resort to removing the nerve. This happens if the pulp is severely inflamed and treatment with other methods no longer helps. This procedure is painful and unpleasant, and to make it easier for the patient to endure it, arsenic paste is used in dentistry.
Effect of arsenic on the nerve
Arsenic has a necrotic effect on the nerve, pulp and nerve endings, that is, it essentially kills the nerve within a couple of days. The doctor applies arsenic paste to the affected area and places a temporary filling on top. After a couple of days of exposure to arsenic on the nerve, the doctor will be able to safely remove the pulp and clean the canals without discomfort for the patient. Pastes with arsenic contain anesthetic agents, so the process of nerve necrosis is also painless. The most common reasons for using arsenic are:
- Inability to use other anesthetics. There are cases when patients experience an allergic reaction or immunity to the effects of anesthetic drugs.
- Urgent treatment by the doctor on duty, when it is not possible to postpone the procedure.
- Inability to use local anesthesia due to the patient's health condition.
How dangerous is the use of arsenic?
Arsenic is indeed a strong poison, but only its derivative is used in dentistry. Thanks to the work of qualified specialists, the effect of the poison occurs exclusively on the nerve. The seal, which the doctor places on top of the applied arsenic paste, reliably protects against the poison getting into the blood or stomach. But the remedy is completely safe only if you carefully follow the instructions of your doctor.
If arsenic remains in the tooth for too long
Despite the fact that the content of toxic substances in the paste is minimal, the product must be removed from the tooth within the period specified by the doctor. The consequences of long-term use of arsenic for a patient can be very unpleasant, for example, leading to the development of diseases such as periodontitis or periostitis. Exceeding the prescribed period of use of the drug also leads to an expansion of the zone of its influence, as a result, destruction of the nerve endings of other teeth, and burns of the gums. An installed filling can, of course, last six months or a year, but this does not mean that you can postpone visiting a specialist.
Signs that the product has been in the tooth for too long:
- headache;
- nausea;
- vomit;
- heat;
- pale or bluish skin tone.
Arsenic is placed in the tooth only for a certain period, which is discussed in advance with the patient. During the next visit, the doctor removes the arsenic and installs a permanent filling.
How to remove the nerve of a tooth today
Today it has become possible to remove the dental nerve by visiting the dentist just once. Depending on the diagnosis, the nerve is removed completely or partially.
- Complete removal. It is performed under anesthesia. After an anesthetic injection, the doctor removes the affected dental tissue and extracts the pulp with a special tool. The procedure lasts on average half an hour. If the depulpation process was controlled using a microscope, the dental canals and the tooth itself are thoroughly filled after the procedure. Sometimes the dentist first places a temporary filling, and then, after making sure that the procedure was completed successfully, changes it to a permanent one.
- Partial removal. It is carried out when only the coronal part of the pulp is affected. The root is preserved, and the inflamed tissue is removed. If the nerve is partially amputated, tooth decay does not occur as quickly. Therefore, this method is recommended for carious disease of molars in children.
When is depulpation performed before prosthetics?
Until recently, nerve removal was a routine process before the installation of permanent structures. Recently, the views of dentists have changed. The fact is that a tooth without pulp is considered “dead”. There is no tissue exchange, secondary dentin is not produced. He becomes fragile. In addition, when there is no pulp, the inflammatory process can completely destroy the tooth, because there will be no pain for a long time.
On the other hand, if the pulp becomes inflamed under the crown, then an expensive and complex restoration will have to be removed in order to carry out treatment.
There is no consensus among dentists whether it is necessary to remove the nerve during prosthetics. Each point of view has its defenders and opponents. The golden rule of dentistry is to carry out manipulations strictly according to indications.
Causes of toothache after nerve removal procedure
It happens that after depulpation, patients complain of pain in the tooth. Most often, this pain is temporary and is explained by surgery and blocked with analgesics. It is caused by eating cold or hot food and jaw movements. After a couple of days, such pain goes away. But if it was not possible to remove the nerve completely or the root canal was poorly cleaned, inflammation and pain return. In rare cases, the cause of pain is an allergic reaction to the filling material. All this can lead to complications and even tooth loss, so if you have complaints, you should not postpone a visit to the doctor.
Without a doubt, removing the dental nerve is a very unpleasant and frightening procedure, but often it is simply necessary in order to save the tooth. Today, this service is provided by many clinics in which qualified doctors will carry out all the necessary manipulations efficiently and as painlessly as possible.
Arsenic poisoning
Before doctors arrive, the victim should be induced to vomit. To do this, he is given 0.5-1 liter of clean water to drink, after which he is pressed with his fingers on the root of the tongue. The manipulation is carried out several times until a clean washing liquid begins to flow away, in which there are no foreign impurities. Next, the patient must be laid down and an influx of fresh air must be provided. For unconscious people, gastric emptying is contraindicated.
First aid
Acute arsenic poisoning requires first aid on the spot. The patient is advised to undergo gastric lavage using at least 10 liters of water mixed with adsorbent. After the procedure is completed, the patient is given 8-10 tablets of activated carbon and 50-100 ml of magnesium sulfate to drink as a laxative. An alternative is unithiol administered into the stomach through a tube. The same drug is infused intramuscularly.
At the prehospital stage, other measures are taken to maintain vital functions. To eliminate hypovolemia and correct electrolyte balance, infusion therapy is started. Anticonvulsants are used for seizures. In order to reduce pain, antispasmodics and analgesics are prescribed. Transfer to mechanical ventilation and titrated supply of vasopressors may be required.
Hospital treatment
Unithiol therapy continues in the hospital setting. The drug is prescribed in a course of 5-6 days. In its absence, the patient should receive N-acetylcysteine, which acts as a donor of monothiol groups. In case of damage by arsenous hydrogen, mecaptide is added to the regimen. Active methods of detoxification are required: intestinal lavage with the introduction of 8-10 liters of saline enteral solution into the intestines, hemodialysis, repeated gastric lavage.
After intestinal lavage is completed, the patient is given an antidiarrheal drug to drink. Infusion of saline solutions is required; in case of severe dehydration, infusion of colloids. Adult patients can receive fluids by mouth (rehydration solutions) as long as this does not cause vomiting. Additionally, glucocorticoids, ascorbic and nicotinic acid are prescribed. Severe metabolic acidosis is eliminated with sodium bicarbonate.
Recovery
After discharge from the hospital, the patient is recommended to be monitored by a local therapist to exclude the development of delayed consequences of chemical injury. It is possible to visit gastroenterological sanatoriums. Food must meet the requirements of table No. 4 according to Pevzner. Restrictions must be observed until the gastrointestinal tract is completely stabilized.