Most often, a sore throat is associated with viral inflammation, which is accompanied by fever, cough, runny nose and minor difficulty swallowing. But, unfortunately, in some situations these diseases can be complicated by the development of purulent-inflammatory complications, for example, peritonsillar abscess, and the task of the ENT doctor at the present stage is the correct diagnosis of this complication and timely treatment, because this complication does not tolerate deposits and is fraught with more significant spread of infection into the deep tissues of the neck. At the GMS Hospital Otolaryngology Center, a comprehensive approach is used to treat peritonsillar abscesses, combining conservative and surgical techniques.
More about the disease
Peritonsillitis is an acute condition secondary to tonsillitis or tonsillopharyngitis, which results in the penetration of an infectious agent (bacteria) into the loose peritonsillar tissue (peritonsillar space). The process is always one-sided, as a result of which it has certain symptoms:
- pain or increased pain on one side;
- severe difficulty swallowing;
- swelling and bulging on the neck on one side;
- asymmetry and bulging of pharynx tissues.
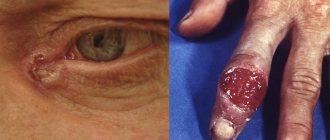
A peritonsillar abscess occurs when a cavity filled with pus forms, located in the peritonsillar (peritonsillar) tissues.
It can form several days after the development of a sore throat or an exacerbation of tonsillitis. Less commonly, due to traumatic injury to the oropharynx or penetration of a foreign body into the tissue around the tonsils. In people with a weak immune system, an abscess can form within a day. It is more often unilateral, but cases with bilateral paratonsillar abscess have been reported in the literature. This pathology is one of the most severe purulent lesions of the oropharynx. With further spread, the infection moves into the deep tissues of the neck (parapharyngeal space), which can lead to a life-threatening condition. Depending on their location, there are several forms of peritonsillar abscess, but all of them require surgical treatment.
The Surgical Otolaryngology Center at GMS Hospital provides proper treatment and diagnosis of paratonsilitis and paratonsillar abscess of any form. Treatment tactics are selected by specialists individually, depending on the stage of the disease, the presence of complications and concomitant pathologies.
Classification
The classification is based on several characteristics. According to the localization of the pathological process, anterior-superior, posterior, posterior-superior, anterior, lateral (external), inferior and bilateral peritonsillar abscess .
According to clinical and morphological manifestations, they are distinguished: edematous , exudative-infiltrative and abscess forms , which, in fact, are stages of development of the pathological process in the peritonsillar tissue that transform into one another. It is the first two forms that are combined with the term “acute paratonsillitis.” The abscess formation stage, with timely and adequate therapy, may not occur.
Why is it necessary to open and drain a peritonsillar abscess?
Peritonsillar abscess is an urgent condition in otolaryngology. The proximity of vital structures (windpipe, large vessels of the head and neck) requires immediate diagnosis and treatment. In the initial stages, when an abscess has not yet formed, the pathology responds well to drug therapy. A course of antibiotic therapy, anti-inflammatory and painkillers is prescribed. If conservative treatment is ineffective, the abscess is opened surgically.
Peritonsillar abscess is dangerous due to its complications, fraught with the development of phlegmon, mediastinitis and even sepsis. The Otolaryngology Department at the GMS Clinic has everything you need to accurately diagnose and treat peritonsillar abscesses.
The opening of the abscess is carried out using modern surgical equipment. During the operation, the potential of laser and radio wave surgery is actively used, which allows the procedure to be performed in the most gentle manner, eliminating the development of surgical complications. Opening abscesses in children is performed under anesthesia, which significantly increases the comfort of the intervention.
Cost of treating peritonsillar abscess
The prices indicated in the price list may differ from the actual prices. Please check the current cost by calling +7 495 104 8605 (24 hours a day) or at the GMS Hospital clinic at the address: Moscow, st. Kalanchevskaya, 45.
| Name | Price |
| Opening of the epiglottis abscess | RUB 54,999 |
| Opening abscesses, phlegmon of the laryngopharynx | RUB 64,995 |
| Opening a paratonsillar or retropharyngeal abscess | RUB 46,998 |
| Drainage of peritonsillar abscess | RUB 24,997 |
| Tonsillectomy + removal of peritonsillar abscess (According to Quinzey) | RUB 189,994 |
Dear Clients! Each case is individual and the final cost of your treatment can only be found out after an in-person visit to a GMS Hospital doctor. Prices for the most popular services are indicated with a 30% discount, which is valid when paying in cash or by credit card. You can be served under a VHI policy, pay separately for each visit, sign an agreement for an annual medical program, or make a deposit and receive services at a discount. On weekends and holidays, the clinic reserves the right to charge additional payments according to the current price list. Services are provided on the basis of a concluded contract.
Plastic cards MasterCard, VISA, Maestro, MIR are accepted for payment. Contactless payment with Apple Pay, Google Pay and Android Pay cards is also available.
Western standards of treatment (evidence-based medicine)
Continuous staff development
Regular interaction with leading Russian and foreign medical institutions
Modern medical equipment and advanced diagnostic and treatment methods
Unified standard of service
We work around the clock 24/7/365
Make an appointment We will be happy to answer any questions Coordinator Oksana
Signs and symptoms of paratonsillitis
The disease has an abrupt onset. An abscess forms a few days after an exacerbation of tonsillitis or the onset of a sore throat and is accompanied by vivid symptoms:
- acute pain in the throat, radiating to the jaw or ear;
- sensation of a “lump” in the throat;
- fever (temperature 39-40°C);
- submandibular lymph nodes are greatly enlarged;
- difficulty swallowing (even drinks);
- the appearance of a repulsive odor from the mouth;
- neck pain that gets worse with exercise;
- general weakness;
- inability to fully open the mouth;
- headache;
- speech impairment (voice as if there is a hot potato in the mouth);
- difficulty breathing (with large ulcers).
Spontaneous breakthrough of suppuration into the throat cavity is accompanied by an improvement in well-being and the appearance of an admixture of pus in the saliva.
The spread of the abscess contents into the peripharyngeal space significantly worsens the condition, so there is no need to delay operations to open the abscess. If you have even one of the symptoms listed above, schedule a consultation with an otolaryngologist today. Doctors at the Center for Operative Otolaryngology at GMS Hospital use gentle microsurgical techniques, which contributes to a speedy recovery and the absence of relapses of the disease.
How is an abscess removed?
A few days before the planned surgery, the patient needs to start taking antibiotics.
Before the autopsy begins, the patient is given an anesthetic for local anesthesia. In the place where the wall of the pharynx protrudes most and has the smallest thickness, the doctor makes an incision into the purulent formation. Its depth does not exceed 10-15 millimeters - this way it is possible to prevent damage to adjacent vessels and nerves. Using a special suction, the surgeon removes purulent contents from the cavity, after which he inserts a blunt instrument into the incision and destroys the partitions of the cavity from the inside to improve the outflow of pus. Next, an antiseptic is injected into the cavity, the doctor stops the bleeding and sutures the edges of the wound.
If during the process it is discovered that the pus does not have a clear localization, but has spread between the fascia of the neck, the surgeon decides to take the necessary therapeutic measures. The scope of the operation is expanding, since this condition is deadly for the person being operated on. If necessary, a drainage tube can be inserted into the patient through incisions in the neck. Each specific situation requires different surgical procedures.
Diagnostics
For the differential diagnosis of paratonsillitis, the following research methods are used:
- examination by an otolaryngologist;
- laryngoscopy;
- pharyngoscopy;
- laboratory tests (blood tests, culture for flora and sensitivity to antibiotics, etc.).
In some cases, to clarify the diagnosis, additional studies are performed - ultrasound, CT scan of the soft tissues of the head and neck.
A comprehensive examination allows you to assess the condition of the abscess and tonsil, determine treatment tactics and the scope of intervention. You can complete all the required tests at the GMS clinic in a day.
Causes
The leading etiological factors of the disease are:
- Penetration of pathogenic microflora into the tissue surrounding the palatine tonsils. The most frequently cultured infectious agent is group A β-hemolytic streptococcus (in 76% of cases). Group G and C streptococci, diphtheria bacillus, and gonococci are much less common among bacterial pathogens; extremely rarely - chlamydia and mycoplasma, Klebsiella, Escherichia coli, pneumococci, fungi of the genus Candida. A significant number of patients with paratonsillitis have various forms of anaerobes.
- Odontogenic factor (dental pathologists - chronic gingivitis , periostitis of the alveolar processes , caries of the upper molars, etc.
- Traumatic injuries with infection of wounds of the mucous membrane of the mouth/throat.
The development of the disease is promoted by:
- Anomalies in the development of the tonsils.
- Chronic inflammatory diseases of the nasopharynx and paranasal sinuses.
- Diabetes.
- Immunodeficiencies.
- Alcohol abuse/smoking, poor nutrition.
- Local/general hypothermia.
Treatment methods
The treatment tactics for paratonsillitis depend on the extent of the spread of the purulent process and the presence of complications. Peritonsillitis in the initial stage is treated conservatively, with antibiotics, decongestants, painkillers and anti-inflammatory drugs. If drug treatment is ineffective or an abscess forms, the abscess is surgically opened and its cavity is drained. The opening of the paratonsillar abscess is carried out under local anesthesia. The otolaryngologist dissects the wall of the abscess, removes the purulent contents, and rinses the cavity with an antiseptic. An improvement in the condition is observed immediately after opening and draining the abscess.
You have questions? We will be happy to answer any questions Coordinator Tatyana
Prevention of paratonsillitis
The following simple preventive measures will help prevent the development of peritonsillar abscess:
- strengthening the immune system;
- healthy lifestyle;
- timely treatment of acute and chronic diseases of the ENT organs (sinusitis, adenoids, pharyngitis, tonsillitis, etc.), caries;
- rejection of bad habits.
In the presence of recurrent abscesses, elective tonsillectomy is recommended.
Opening a peritonsillar abscess at the GMS clinic is a simple and safe surgical procedure that is performed in an outpatient or inpatient setting. Recovery takes 10-14 days, after which you will return to your normal life. You can make an appointment with an otolaryngologist at GMS Hospital by phone or using an online application.
List of sources
- Palchun V.T., Kryukov A.I. Otorhinolaryngology: A guide for doctors. M., 2001: 257-315.
- Taukeleva S.A. Peritonsillitis. Almaty. 1997. pp. 38-43.
- Izvin A.I. Clinical lectures on otorhinolaryngology, Tyumen, 2004.
- Palchun V.T., Luchikhin L.A., Kryukov A.I. Inflammatory diseases of the pharynx. M.: “GEOTAR-media”, 2007: 288 p.
- Kiselev A.S. Towards the diagnosis of acute purulent inflammation of the para- and retropharyngeal spaces // News of otorhinolaryngology and logopathology. 1998. No. 4. pp. 80–82.