Traumatologist-orthopedist
Shelepov
Alexander Sergeevich
13 years of experience
Doctor
Make an appointment
Many people mistake a small bulge that appears on the bone as the result of an injury. Education in the early stages does not create any special problems or cause discomfort, so a visit to the doctor is postponed. As a result, patients consult a doctor after the onset of painful sensations, when the osteoma becomes visually noticeable, begins to cause severe discomfort and leads to deterioration of health.
Osteoma is a benign tumor-like neoplasm developing from bone tissue, which is not predisposed to transition to a malignant state. It develops slowly. Osteoma is dangerous because it develops imperceptibly, without pronounced symptoms, so most people turn to doctors when the pathology is severely advanced and long-term treatment is necessary. Osteoma grows slowly, which allows patients to be successfully treated if treated in a timely manner.
Symptoms and signs
Osteoma, the size of which depends on the nature of the formation, can appear on any part of the body. As the formation develops, the symptoms appear clearly. The presence of pathology may be indicated by:
- the presence of a lump, noticeable visually or felt by palpation;
- swelling of the tissues around the formation;
- a feeling of numbness in an area of the body due to pressure on blood vessels;
- increasing pain;
- difficulty moving.
When palpated, osteoma, the symptoms of which vary depending on the location, is felt as a dense formation. Osteoma of the brain is the most difficult to determine; it can be accurately diagnosed only with the use of modern diagnostic equipment.
Depending on the location, the pathology manifests itself as follows:
- Osteoma on the head, when localized on the internal plates of the cranial vault, manifests itself as headaches, memory problems, and seizures;
- occipital osteoma leads to frequent headaches, in some cases to epileptic seizures;
- osteoma of the lower limb bone causes gait disturbances, muscle pain when walking, swelling of the legs;
- osteoma of the frontal sinus is manifested by headaches and increased intracranial pressure;
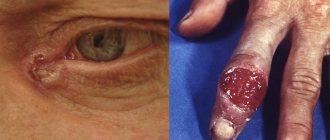
- Osteoma of the skull can manifest itself as a strong protrusion of the eyeball;
- Osteoma of the nose is manifested by the disappearance of the sense of smell, difficulty in nasal breathing, deterioration of vision, drooping of the eyelid;
- osteoma of the lower jaw is manifested by difficulties in chewing food, etc.;
- osteoma of the rib bone is manifested by pain behind the sternum;
- Pathology in the vertebral area leads to the formation of scoliosis.
Osteoma of the sinuses and osteoma of the jaw are most often the reason for seeking medical help.
Solitary form of peripheral osteoma on the lower jaw
Osteoma is a rare, slow-growing, benign osteogenic tumor that most often occurs in the maxillofacial region. These types of neoplasms can be found both on the surface of the bone (formed from the periosteum - peripheral, periosteal or exophytic form), and in the structure of the bone marrow space (formed from the endosteum - endosteal or central form). The case of verification of osteoma in the structure of muscle tissue is rare.
The pathogenesis of peripheral osteoma remains a completely unresolved clinical and scientific issue: there are opinions that the neoplasm can be attributed to true tumors or to reactive lesions provoked by trauma, constant traction of the muscles attached to the periosteum, as well as the action of infectious factors. Endocrine changes, in turn, can be a direct etiological factor initiating the occurrence of a neoplasm. Depending on the action of endocrine factors on the tumor, they can be classified as central and peripheral, or extraosseous.
Osteoma is the most common benign tumor of the nose and paranasal sinuses and the most common neoplasm in the frontal sinus. Single peripheral osteomas that occur in the lower jaw are quite rare lesions and are diagnosed in people of different age categories (from 4.8 months to 50 years), equally often in both men and women. Typically, clinically the tumor grows asymptomatically, and radiographically it manifests itself as a distinct contrasting area of a round or ovoid lesion. Depending on the histological picture, compact, spongy and mixed forms of osteoma are distinguished. The presence of many small osteomas in the structure of the lower jaw is diagnosed as Gardner's syndrome, which is also characterized by the presence of perirectal polyposis and associated skeletal abnormalities. These symptoms can be used to differentiate between Gardner's syndrome and multiple dental impaction.
Treatment of osteomas is carried out through surgical excision of the tumor, but only in those patients who complain of accompanying uncomfortable symptoms of the tumor. Until now, only 26 clinical cases of verification of single peripheral osteomas of the mandible not associated with Gardner's syndrome have been reported in the literature.
Based on the extreme rarity of the disease, the purpose of this article is to illustrate an unusual clinical case of a single peripheral osteoma found in the structure of the mandible, as well as to conduct a retrospective analysis of the literature data regarding the pathogenesis, differential diagnosis and choice of treatment for this type of benign tumor.
Clinical case
A 30-year-old patient applied to the Department of Dentistry with the main complaint of swelling on the inside of the posterior part of the lower jaw, which she had noticed since the age of 8. 8 years ago, the formation that had been present since childhood increased to 5 mm in diameter, after which it began to grow progressively. Although the swelling was asymptomatic, due to its large size it provoked a feeling of discomfort when eating. The latter motivated the patient to seek dental care. The patient did not have any hereditary diseases in her own or family history, as well as a recent injury to the problem area of the jaw. Based on the fact that no other symptoms other than a tumor in the mouth were found, Gardner's syndrome was excluded from the list of possible diagnoses. Clinically, a single pedunculated oval node was detected on the lingual side of the jaw in the area of the 36th and 37th teeth. The tumor was more than 1 cm in diameter (Figure 1), and the overlying mucosa showed no signs of change or inflammation. Upon palpation, the tumor was painless, and it was also possible to manually establish its lobular shape and hard consistency.
Photo 1: View of a tumor in the oral cavity.
On a cross-sectional radiograph of the lower jaw, a clear radiopaque area of irregular shape is visualized, connected to the cortical plate of the jaw in the area of the 37th tooth through a pedicle (photo 2). The radiographic density of the formation is similar to the density of the body of the lower jaw. In the process of differential diagnosis, possible variants of bone exostosis, peripheral osteogenic fibroma, osteoid osteoma, osteoblastoma and osteosarcoma were analyzed. After carefully explaining to the patient the essence of the future surgical procedure and the possible risks of manipulation, complete excision of the tumor was performed using rotary instruments and a bone chisel. During surgery, an excisional biopsy of the tumor was also performed under local anesthesia.
Figure 2: Cross-sectional radiograph of the mandible.
Histopathological analysis of the lesion helped to establish that the tumor consists of dense bone tissue, in which concentric layers of bone plates are observed, as well as osteocyte cells in the lacunae (photo 3). The results of histopathological examination along with clinical and radiological findings helped confirm the diagnosis of compact osteoma.
Photo 3: Hematoxylin-eosin staining (10x magnification).
Discussion
According to the World Health Organization classification, osteoma belongs to benign neoplasms, consisting of differentiated mature bone tissue cells with a predominance of laminar structure, and with a very slow growth pattern.
It is not yet clear whether osteomas are true benign neoplasms or hamartomas. Although, on the other hand, the latest WHO classification of diseases defines osteoma as a truly benign tumor of bone tissue, clearly differentiating it from exostoses and other types of hamartomas.
The true etiology of the lesion has not been thoroughly elucidated, although Fetissof and Varboncoeur argue that the tumor develops either from embryonic cartilaginous remnants or from persistent embryonic cells contained in the periosteal structure. According to the embryological theory, osteomas originate from the area of sutures of bone structures filled with tissues of different embryonic origin (membranous or enchondral). Other possible etiological factors are inflammation, trauma or endocrine pathologies. Kaplan et al suggested that the combination of trauma and persistent muscle traction in the periosteal region plays a key role in the development of the peripheral type of neoplasm. But the above-mentioned theories of osteoma formation do not explain the mechanism of its development in the described clinical case. Regezi and Sciubba, as a result of a comprehensive analysis, came to the conclusion that none of the proposed etiological theories fully explains the cause and mechanism of development of the neoplasm.
Histologically, three types of osteomas can be distinguished: hard or compact (consisting of a dense, ivory-like compact substance with a small amount of spongy bone, this type of pathology is quite difficult to resect), cancellous (trabecular), or mature (consisting of soft spongy bone and bone marrow) and mixed. Single peripheral osteomas (PO) of the jaws are quite rare lesions and are most often diagnosed in young people with the same frequency in both men and women. The patient described in the clinical case mentioned above was 30 years old. Typically, osteomas are asymptomatic tumors and can often go undetected until they cause visible facial asymmetry or functional malocclusion. In this case, the pathology must be confirmed by x-ray examination. The most common topography of osteomas is the area of the body of the mandible behind the premolar on the lingual surface and the area of the condylar process. Less often, osteomas occur in the area of the angle, coronoid process and ramus of the mandible, or in the area of the external auditory canal, orbit, temporal bone, maxilla, zygomatic arch and pterygoid processes. Often osteomas can be verified as part of Gardner's syndrome, characterized by the presence of several tumors in the jaw structure, pararectal polyps with a high degree of malignancy, cutaneous fibromas, congenital retinal hyperpigmentation, tooth retention, enostosis, epidermal cysts and supernumerary teeth. Gardner syndrome is an autosomal dominant disease caused by a mutation in the structure of the APC suppressor gene, which is responsible for the occurrence of adenomatous polyposis of the colon. It is extremely rare, but detection of osteomas is also possible in Haberland syndrome (encephalocraniocutaneous lipomatosis).
Radiologically, a peripheral osteoma may have a mushroom-shaped or oval-shaped lesion that is in close contact with the adjacent cortical plate of the mandible. Moreover, the bone density in the jaw area and in the area of the neoplasm is almost identical. Traditional radiography methods, such as occlusal radiographs, are usually sufficient to diagnose osteoma, as in our case. When the tumor is located deeper in the tissues of the maxillofacial region, other highly effective imaging methods can be used to identify it: panoramic radiography, occipitomental projection radiography of the sinuses, computed tomography (CT), magnetic resonance imaging (MRI) or cone -radiation computed tomography (CBCT). Spiral computed tomography provides opportunities for three-dimensional reconstruction of osteoma: using radionuclide imaging, it is possible to distinguish between actively growing neoplasms (“hot”) and stable lesions (“cold”). In the structure of spongy osteoma, the vascular component predominates, while in the compact type of tumor there are almost no vascular elements observed. Differential diagnosis of different types of formation can be carried out using intravenous angiography.
Differential diagnosis of osteoma is carried out with bone exostoses, osteochondroma, osteoid osteoma, periosteal osteoblastoma, peripheral osteosarcoma, peripheral osteogenic fibroma, Paget's disease, fibrous dysplasia and odontoma. Exostoses are hamartomas that are usually located on the lower jaw or in the palate. Typically, exostoses stop growing after puberty, while osteomas continue to slowly increase in size, occupying a limited volume and forming a lobulated radiopaque structure. Osteochondromas consist of areas of endochondral ossification, calcified cartilage, and adipose or bone marrow tissue within the lumen of the trabecular space. Osteoid osteomas, on the contrary, are characterized by rapid growth, are often painful and contain a large number of vessels and an osteoid component. Periosteal osteoblastoma is also a rapidly growing, painful, round or oval tumor attached to a specific area of the cortex. Parosteal osteosarcoma is often diagnosed in the posterior region of the mandible, representing a homogeneous or heterogeneous formation with a poorly verified lobular sclerotic structure. Telangiectasias are often observed at the periphery of the tumor, and Codman's triangle can be seen on the radiograph. Peripheral osteogenic fibroma can be found only in the gum area; it is a reactive lesion of dense consistency, often found in the anterior part of the upper jaw. Symptoms of Paget's disease are more typical for the anatomical areas of the femur, skull and vertebrae, while in the jaw area, bone damage is observed much less frequently and more often in the older age group. In this case, bone damage, as a rule, is always bilateral, and more often affects the upper than the lower jaw. Bone tissue in Paget's disease becomes deformed and increases in size. Fibrous dysplasia is usually seen in the posterior maxilla and radiographically appears as a diffuse, contrast-enhancing mass that may resemble ground glass, orange peel, or cotton wool. Odontomas often complicate the physiological eruption of permanent teeth, while their radiological density is almost identical to that of enamel and dentin, and the affected area is always surrounded by a radiopaque capsule.
conclusions
During the clinical examination of patients with osteomas, significant attention should be paid to the family history to exclude a possible diagnosis of Gardner's syndrome. Asymptomatic osteomas should be under constant observation, and pathologies that cause uncomfortable symptoms should be surgically removed, having previously organized a complex of clinical and radiological studies to accurately make the final diagnosis.
By Rohit Agrawal Shipra Agrawal Shitij Bhargava Mahesh Motlani Rahul Agrawal
Causes
The exact reasons for the development of tumor formations of this type have not currently been established. The cause of some formations is heredity.
Among the reasons that can lead to the development of osteoma, experts name:
- gout;
- rheumatism;
- chronic inflammatory processes;
- some infections, in particular syphilis;
- metabolic problems (calcium imbalance);
- purulent chronic processes.
Experts also believe that osteoma, the symptoms of which depend on the location, can form as a result of injuries, repeated injuries or hypothermia. When a bone is damaged due to a bruise, crack or fracture, compact osteoma is most often diagnosed, the development of which is due to natural regeneration processes.
Risk factors
In addition to injuries and inflammatory diseases, the following unfavorable factors can provoke pathology:
- chronic rheumatism;
- bad ecology;
- metabolic problems, in particular disturbances in calcium metabolism;
- chronic inflammatory processes.
Complications
Osteoma does not transform into a malignant formation, so patients can lead a normal lifestyle. The cause of complications is compression of adjacent anatomical structures by the enlarged tumor. Some forms of pathology can cause serious problems, in particular osteoma of the frontal sinus can lead to a brain abscess. Osteoma of the sinuses can cause decreased or sharp deterioration of vision.
Complications during the development of education, depending on the location, can be circulatory disorders, brain pathologies, diseases of the nervous system due to damage inside the membranes of the brain, blood vessels, and nerve roots. In many cases, if osteoma is diagnosed, removal is the only effective solution to the problem.
Etiology and pathogenesis
The causes and origin of osteoma are not fully known. Some researchers consider it a neoplasm that develops at a certain time. Others tend to classify the lesion as an anomaly of the craniofacial bones.
Doctors also named the following as possible etiological factors:
- trauma, since most formations are located in the lower part, which is more susceptible to traumatic lesions;
- combination of injury and muscle strain;
- infectious or inflammatory processes of the oral cavity or jaw bone tissue
Study of the etiology of benign jaw lesions
When to see a doctor
If signs of pathology appear, the only correct decision is to consult a doctor. The answer to the question of which doctor treats osteoma depends on the location of the tumor. You should make an appointment with a doctor if you experience:
- paroxysmal headaches, muscle cramps, problems with memory and concentration (localization in the skull);
- deformation of the skull, severe pain, breakdown with chewing (osteoma of the jaw);
- difficulties when moving, etc.
If signs appear, the patient must contact a traumatologist, who, based on the results of the examination, will refer to a specialist (maxillofacial surgeon, neurosurgeon).
Our clinic in the center of Moscow offers the services of highly qualified doctors - specialists of the highest categories. They have knowledge and experience in diagnosing and treating osteoma.
Factors
There is a consensus among experts on the question “what are the reasons for the formation of such a tumor?” does not exist. It is argued that there is a connection between osteoma of the jaw and a number of factors. These include:
- Trauma to the maxillofacial bones, chronic or one-time (bruise, damage to the integrity of the oral mucosa, untreated teeth (which caused them to quickly collapse), tartar (hard dental deposits), dentures and dental implant crowns that change the bite (poorly fitted) ), poor surface treatment of dental fillings that do not allow the jaws to fully close).
- Inflammation in the area of the nose and jaw (actinomycosis, sinusitis, periodontitis, osteomyelitis, periostitis, sinusitis and other pathologies), chronic or acute.
- Aggressive environmental effects (smoking, chemical, ionizing and radioactive exposure).
- Foreign particles in the sinuses above the upper jaw (often fragments of teeth or particles of materials used to fill teeth).
Experts do not classify osteoma itself as an odontogenic disease. But there are factors that provoke the appearance of a tumor.
Diagnosis of osteoma
If a patient is suspected of having osteoma, diagnosis is carried out using all diagnostic methods (clinical and radiological). The main goal of diagnosis is to determine the nature of the tumor. The list of diagnostic methods includes:
- palpation;
- blood analysis;
- x-ray to assess the functioning of the affected areas (joints);
- MRI to accurately determine the type of tumor;
- computed tomography with 3D reconstruction to determine the size and density of the pathology and select the appropriate course of treatment;
- histological analysis (biopsy) to exclude the possibility of developing an oncological process;
- scintigraphy;
Types of osteomas
Diagnosis of osteoma involves differentiation from similar neoplasms and determination of its type in order to select subsequent treatment.
Tumors are divided by number, type of tissue they are made of, method of germination and complexity of structure. Each of them can be located in different parts of the musculoskeletal system and provoke different symptoms. Based on the number of tumors, they are divided into single (solitary) and multiple, and based on their composition into solid, spongy and medullary. The first consist entirely of bone tissue without bone marrow, the second of spongy substance, and the third of bone marrow cavities. Tumors originate from different tissues (bone or connective) and because of this they have different names:
- hyperplastic – consist exclusively of bone (osteomas and osteoid osteomas),
- heteroplastic - osteophytes, composed of different tissues.
Osteomas are composed of normal bone tissue, are localized on the bones of the skull, and often put pressure on neighboring organs, such as the eyes. Osteoid osteomas consist of osteogenic tissue penetrated by blood vessels, bone membranes, areas of destroyed bone tissue, and are localized anywhere, in 50% of cases - on the tibia. At the initial stage of development of the disease, there are no symptoms, and then a flat, thin infiltrate appears (if we talk about epiphyseal osteoma, it accumulates in the joint). If in children this type of tumor occurs in the bone growth zone, then one limb will increase in length.
Osteophytes are also divided into 2 types - ectostoses, which grow from above (the skull, face, pelvic bones are the favorite places for their localization), and enostoses, internal, growing into the medullary canal. Exostoses have the shape of a hemisphere, cauliflower, thorn, or mushroom. One of the features of osteophytes (heteroplastic osteomas) is that they appear on the diaphragm, lining of the heart, brain tissue, etc.
Treatment
Specialists select a course of treatment based on examination data, depending on which the doctor may decide to remove the osteoma or choose other treatment tactics.
Osteoma surgery is prescribed in cases where the formation negatively affects the human body, with severe pain.
Surgery is indicated if:
- the tumor is large;
- the activity of related organs is disrupted;
- movement functions are impaired;
- the tumor negatively affects appearance.
Osteoma surgery is performed using various surgical methods:
- traumatologists and orthopedists operate on limbs;
- Facial surgeons and neurosurgeons operate on jaw, frontal and maxillary sinus pathologies.
Treatment of osteoma by removal is also carried out by evaporation using a laser (endoscopy). This technique is used to remove seals of any location. Its use ensures a speedy recovery.
If osteoma is diagnosed, removal of the seal is possible using radiofrequency ablation using electrode needles. Heating the seal leads to the destruction of formations on the bone.
Drug treatment of osteoma is also used by prescribing painkillers. This treatment is prescribed for small tumors.
How to make an appointment with a traumatologist
JSC "Medicine" (clinic of academician Roitberg) in Moscow offers the services of qualified specialists in the field of diagnosis and treatment of osteoma. If you suspect osteoma, you can make an appointment with a traumatologist in various ways:
- select a doctor in the “Our Doctors” section and make an appointment online;
- call +7 (495) 775-73-60;
- leave a request for a call in a special form on the website.
The clinic is located in the central district of Moscow at 6 2nd Tverskoy-Yamskaya lane 10 (Tverskaya, Chekhovskaya, Mayakovskaya, Belorusskaya, Novoslobodskaya metro stations).