Definition
Dental cement is a special bone tissue that completely covers the root, close to the tooth enamel. Thanks to cement, the tooth is firmly attached to the bone alveolus and does not fall out of the gums. Without such a protective coating, the root dentin would be exposed to pathogenic bacteria, causing the tooth to continually deteriorate from the inside.
Kinds:
- primary or acellular, which covers the lateral surfaces of the tooth root;
- secondary or cellular, which covers the bifurcation area of multi-rooted teeth, as well as the apical third of the root.
Most often, cement is layered onto the enamel, leaving the root unprotected. More often the cement comes close to the enamel, but it also happens that it does not reach, leaving a strip of dentin unprotected. This is quite dangerous, since unprotected dentin is susceptible to cervical caries.
Dental cement is formed throughout life, and the formation process is not uniform. With chronic periodontal inflammation, cement formation increases significantly, which can even lead to hypercementosis. And in cases of tooth root resorption, the newly formed cement can not only replace the dead areas of the root, but even help restore its function.
Periodontal fibers
The bulk of periodontal fibers consists of type I collagen. It is synthesized in fibroblasts. Next, tropocollagen molecules are formed, which form microfibrils, then fibrils, threads and bundles:
This structure of collagen fibers allows them to be both strong and flexible. In longitudinal section they have a wavy shape:
As with gingival fibers, many classifications of periodontal fibers have been proposed. According to one, there are 6 groups of periodontal fibers:
- transseptal;
- alveolar ridge fibers;
- horizontal;
- oblique;
- apical;
- intraradicular (interradicular).
The term “Sharpey fibers” is also often found in the literature, but this is not another group. These are the terminal, partially or completely calcified parts of periodontal fibers of all 6 groups, which intertwine and perforate the cement and alveolar bone. Plus, Sharpey's fibers are associated with non-collagenous proteins (osteopontin, bone sialoprotein) in bone and cement (red arrow in the figure), which ensures such a strong connection.
Transseptal fibers
Transseptal fibers (F) pass over the alveolar ridge (A) and connect two adjacent teeth (T). They are often classified as gingival fibers because they are not woven into the bone.
Alveolar ridge fibers
They originate in the area of cementum of the tooth root immediately below the attachment epithelium, go in an oblique direction and attach to the alveolar ridge or periosteum.
Horizontal, oblique and apical fibers also extend from the cementum to the bone. The only difference is in the angle at which they are directed and in which part of the periodontal ligament they are located. Horizontal ones are located at right angles closer to the edge of the tooth socket, apical ones in the area of the root apex. There are more oblique fibers between them. They are the ones who take on the vertical load that occurs during chewing and “transfer” it to the bone.
Interradicular fibers (as the name suggests) pass between the roots of a multi-rooted tooth (from the furcation) to the bone.
In addition to the main groups, the periodontal ligament also contains other, less ordered collagen and elastic fibers. Elastic fibers are mainly located parallel to the tooth in the cervical third of the root. They regulate blood flow in the vessels of the ligament.
Periodontal fibers are constantly renewed due to the work of periodontal cellular elements.
Structure
The structure of primary and secondary cements is different.
- Primary (acellular) consists mainly of collagen fibers, as well as an amorphous adhesive substance.
- The secondary (cellular) structure is similar to coarse-fiber bone, only without blood vessels, and contains mainly cementocytes, cementoblasts and intercellular substance.
Unlike real bone tissue, cement is nourished diffusely through the periodontium. The chemical composition consists of organic substances, which make up 32%, and inorganic substances, which make up 68%.
Tooth root cement: structure and functions
In this article, the author examines the general concept of tooth root cement. The detailed structure of root cement and its main functions is also given. Histological preparations are considered.
Key words: dental cement, dentistry, histological preparations, tooth structure.
Within the framework of this article, the author considers the general concept of tooth root cement. The detailed structure of the root cement and its main functions are also given. Histological preparations are considered.
Keywords: tooth cement, dentistry, histological preparations, tooth structure.
Dental cement is a highly mineralized tissue, similar in structure to coarse-fibered bone, that covers a thin layer from the root of the tooth (to its neck). But unlike bone tissue, root cement does not undergo constant restructuring, it does not have blood vessels, and its trophism is carried out due to the usual diffusion of nutrients dissolved in the main amorphous substance of the periodontal structure. [1]
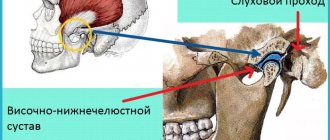
The main function of cement is the formation of the ligamentous apparatus of the tooth (periodontal attachment), which holds the tooth in the socket and also helps to redistribute chewing pressure from the tooth to the alveolar bone. Let us recall that periodontal fibers begin to develop simultaneously - both from the side of the root cement and from the side of the compact lamina of the alveoli. In addition, with the help of immature collagen (procollagen) in the center of the periodontal fissure, the ends of these fibers are tied together and fiber bundles are formed. [2, p. 43]
Rice. 1. Structure of tooth cement
The cementum layer is present only in human teeth, as well as in the teeth of other mammals. In the area of the tooth neck, the thickness of the cement is less - from 20 to 50 microns, and in the area of the root apex - from 100 to 150 microns. I think you are familiar with the fact that “secondary dentin” is produced by odontoblasts throughout life, and similarly, throughout life there is a constant accumulation of cementum on the root surface. So, if you live to retirement age, the cement in your teeth will likely have grown to at least three times their thickness (Figure 1).
In terms of chemical composition and strength, cement is close to coarse-fiber bone tissue. Inorganic components in the composition of cement make up about 65% - mainly calcium phosphate (in the form of hydroxyapatite crystals or amorphous calcium phosphates) and calcium carbonate. Organic components make up about 23% and consist almost entirely of collagen; plus about 12% water. [4, p. 31]
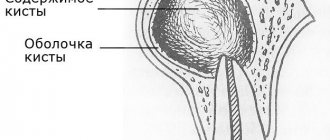
Cementum is divided into 2 forms - primary (acellular) and secondary (cellular). A layer of primary cement covers the dentin of the entire surface of the tooth root, and a layer of secondary cement, in turn, will be located on top. However, this so-called secondary “cellular cement” will no longer cover the entire surface of the root, but only its apical third + in multi-rooted teeth also the bifurcation/trifurcation zone of the roots (Fig. 2).
Rice. 2. Cement layers (electron microscopy)
1) Primary cementum (acellular) - Primary cementum covers the entire tooth root. It does not contain cells and consists only of a calcified intercellular substance, which includes collagen fibers and a basic amorphous “glue” substance. The collagen fibers of this cement layer are characterized by uniform mineralization, some of them having a longitudinal direction relative to the root surface, and some of them having a perpendicular (radial) direction. They are called "Sharpei's fibers" and are very important for holding the tooth in the socket. [5, p. eleven]
2) Secondary cement (cellular) - Secondary cement is formed after tooth eruption, and it does not cover the entire surface of the root, but only its apical third + the area of splitting of multi-rooted teeth. It can be placed either on the primary cementum or directly adjacent to the root dentin. Secondary cementum consists mainly of cells, as well as intercellular substance, which, in turn, consists of a basic amorphous substance and randomly directed collagen fibers.
Cementocytes (Fig. 3) - lie on the surface of the cement in special lacunae (cavities) and in their structure are very similar to cementocytes of bone tissue. Cementocytes have long processes, and where the cellular cement adheres directly to the dentin surface, the processes of the cementocytes may directly contact the dentinal tubes. As new layers of cement form, the cement cells of the inner layers gradually die, creating empty spaces in the cement.
Cementoblasts - these cells are “cement builders,” i.e., they ensure the deposition of new layers. Cement deposition by cement explosions occurs throughout a person’s life, and therefore the thickness of cement in the area of the root tips increases several times by the end of life [3, p. 65]
.
Rice. 3. Cementocytes in secondary cement (histology): 1 - cementocyte, 2 - dentinal tubules, 3 - contacts of cementocyte processes with dentinal tubules
3) Collagen fibers - the most important part of the collagen fibers of cementum are the so-called “Sharpey's fibers”. They represent the end sections of the fibers of the periodontal attachment of the tooth on the cement side. In Fig. 4 you can see a histological specimen that shows that the radial collagen fibers of the periodontal fissure and the cementum of the tooth root are “one whole”.
Rice. 4. Connection of periodontium and cementum of the tooth root
It was previously believed that the radial periodontal fibers (which are attached to the lamina compacta of the alveoli on one side and to the root cementum on the other) were a single unit. But modern research shows that this is not entirely true. The terminal sections of periodontal dento-alveolar fibers begin to form separately from each other: one part - from the side of the cement of the tooth root, and the other part - from the side of the bone plate of the alveoli. [2, p. 10]
And when both parts of the fibers reach the middle of the periodontal cleft, they are connected with the help of immature collagen fibers (procollagen fibers) into a single network. The plexus of immature collagen fibers in the center of the periodontal cleft is called the "Siecher plexus"
Topography of cement in the area of the tooth neck - There are 3 options for connecting cement and tooth enamel. This may be either "joint to joint", or the cement may penetrate slightly into the enamel, or there may be a strip of exposed dentin (Fig. 5). Studies have shown that enamel and cement border “joint to joint” - only in 30% of cases. At the same time, 60% of teeth have a layer of cement along the edge of the tooth enamel (Fig. 6), and a strip of exposed dentin is found in 10% of cases.
Rice. 5. Options for the enamel-cement boundary (diagram): 1 - enamel, 2 - dentin, 3 - cement, and options for joining enamel and cement (I - cement partially extends onto the tooth enamel; II - cement joins the enamel, III - cement does not reaches the tooth enamel)
Rice. 6. Variants of the enamel-cementum border (histology)
Functions of tooth root cement:
1) Protective function - the content of inorganic components in cement reaches 70%, which makes it durable to mechanical loads. Therefore, one of its functions will be to protect root dentin from damaging effects. [4, p. 89]
2) Participation in the formation of periodontium - the formation of periodontal fibers occurs simultaneously both from the side of the cement of the tooth root and from the side of the bone plate of the alveoli. According to some authors, these collagen fibers subsequently intertwine with each other through immature collagen (procollagen), turning them into a single whole. The depth of immersion of periodontal fibers into the cement of the tooth root is from 3 to 5 μtl.
3) Fixation (retention) - cement of the tooth root together with the compact plate of the alveoli and periodontal fibers - ensures fixation of the tooth in the alveoli.
4) Compensatory function - when the length of the tooth decreases as a result of physiological abrasion of the enamel, there is an increased production of cement in the area of the tip of the tooth root. As a result, the tooth is pushed out of the alveoli into the oral cavity, and thus the size of the clinical crown of the tooth increases. This is especially noticeable in older patients.
5) Participation in reparative processes - for example, when the cause of root resorption is eliminated, its partial restoration may occur. Or, if there is a crack in the root of the tooth, cement may form between the fragments, which can lead to the elimination of the defect.
The reasons for the additional formation of cement are during periodontitis and chronic periodontitis, when the enamel on the occlusal surfaces is erased, when the load on the tooth increases, and also in the absence of an antagonist tooth, intensive deposition of cement is observed in the apical third of the root. Trauma to the root of the tooth, as well as orthodontic treatment, can also lead to this. [3, p. 58]
In addition, there is also such a formation as “cementite”. This is nothing more than a rounded formation consisting of cement located in the periodontium. They arise due to the mineralization of microvessels in the region of the islets of epithelial cells of Malasse.
Development of cement (cementogenesis) - The formation of cement occurs in two stages. At the 1st stage, the synthesis of an organic matrix (cementoid or primary cement) occurs. At the 2nd stage, mineralization of the cementoid occurs with the formation of secondary cement. Let's see how it all happens.
First, dental papilla cells (as a result of the inducing effect of the epithelial sheath) differentiate into root odontoblasts, which form root dentin. Next, the cementoblasts of the dental sac begin to produce an organic cement matrix (cementoid), as well as collagen fibers and the main amorphous substance. As a result, the cementoid is deposited on the surface of the root dentin - in the form of a highly mineralized structureless Hopewell-Smith layer (this layer contributes to the strong attachment of cement to the root dentin) [5, p. 99].
Next, the first primary cementum is formed, which does not contain cells. It is slowly deposited as the tooth erupts, covering 2/3 of the root surface (closer to the crown of the tooth). Next, mineralization of the cementoid occurs, which is associated with the deposition of phosphates and calcium carbonate. This process occurs in waves, and then cellular, i.e., secondary cement is formed in the apical third of the root and the furcation zone.
Literature:
- The European Academy of Paediatric Dentistry (EU)
- Gaivoronsky I.V., Petrova T.B. “Anatomy of human teeth.” Tutorial. St. Petersburg: ELBI-SPb, 2005. - 56 p.
- A. M. Politun, N. I. Smolyar. "Therapeutic dentistry". Per. with him. -Lvov: GalDent, 1999. - 409 p.
- Glinkina V.V. “Histology of the oral cavity.” 2nd ed., revised. and additional - Samara: Etching, 2011. - 186 p.
Cement for dental crowns and dentures
In dentistry, cement means not only the natural material that covers the root of the tooth, but also the artificial material with which dentures, crowns and veneers are attached. Artificial cement for crowns is used for their permanent fixation; it is constantly in the patient’s mouth and therefore should be as close to natural as possible. It should not affect the dental pulp or injure the soft tissues of the oral cavity, and should not dissolve in saliva or shrink during use.
Therefore, in modern dentistry, only those materials are used that best meet the requirements.
Denture cement is also called dental glue, because it is used to glue not only crowns and bridges to teeth, but also veneers, lumineers, and other dental structures, the main purpose of which is to give the patient a snow-white Hollywood smile.
TOOTH PULP
There is a cavity inside the tooth that resembles the shape of a crown, and at the root of the tooth it continues in the form of a canal. The root canal ends at the apex of the tooth root with an opening. The tooth cavity is filled with loose connective tissue, rich in blood vessels and nerves - pulp. The dental pulp is divided into crown and root parts. The pulp of the tooth crown is represented by loose connective tissue with a delicate network of collagen and precollagen fibers with a large number of cellular elements. In the tooth root pulp, collagen structures are denser, thicker and oriented longitudinally along the neurovascular bundle.
Based on the cellular composition of the pulp, they are divided into: peripheral, subodontoblastic and central layers.
The peripheral layer consists of specialized cells - odontoblasts, which take part in the metabolic processes of enamel and dentin. They are located in several rows.
The odontolast has an elongated pear-shaped shape. It has a peripheral protoplasmic process (or dentine), which runs in the dentinal tubule to the dentinoenamel junction, and short lateral processes that anastomose with neighboring cells in the early stages of differentiation.
The subodontoblastic and central layers consist of small, poorly differentiated stellate cells connected to each other by short processes. The pulp contains many fibroblasts that participate in the formation of a fibrous capsule that limits the focus of inflammation.
In the central layers there are cytoplasmic cells - histiocytes. During inflammation, they acquire the ability to move and phagocytose and are called macrophages.
The blood supply to the pulp is provided by blood vessels that penetrate into it through the opening of the apex of the tooth root and through additional canals from the periodontium. The lymphatic system in the pulp is presented in the form of slits, capillaries, and vessels. The outflow of lymph from the pulp occurs in the submandibular and mental lymph nodes. Arterial trunks accompany veins. The pulp vessels have numerous anastomoses. Through the apical foramen, sensitive pulpy and non-pulse fibers of the trigeminal nerve pass, which innervate the pulp, forming plexuses.
The dental pulp has a trophic, protective and plastic function. The trophic function is carried out due to the developed network of blood and lymphatic vessels; protective - due to histiocytes, plasma cells; plastic is the participation of the pulp in the formation of dentin.
The bulk of the tooth is dentin, which surrounds the tooth cavity. In the area of the tooth crown, dentin is covered with bright white enamel. The dentin of the root is covered with cement.