Caries (from the Latin process of decay) is a disease of dental tissues with their subsequent destruction. Dental caries account for 90% of all visits to the dentist. Caries develops as a result of the activity of pathogenic microflora. During the life of bacteria, acids are left on the surface of the teeth, destroying the enamel and deeper layers of the tooth.
Pathological processes occur slowly, and symptoms often appear only in the later stages of caries and are caused by exposure of the pulp capsule. If left untreated, caries also affects the pulp, leading to atrophy of the root system and early loss of teeth.
What is caries - main aspects
Dental caries is a long-term process of demineralization of enamel and destruction of hard tooth tissues. The disease is characterized by several stages of development. With a long course, a cavity defect is formed, which can be seen upon careful examination. A dental examination can detect caries at the chalk spot stage, an early stage of defect formation.
Symptoms of the early period of destruction of dental tissue are mild. On the surface of the enamel, spots ranging from pale yellow to gray are barely visible. Increased reaction to temperature and chewing of food. Medium and deep caries increases the intensity of symptoms, pain appears during exercise or at rest.
The disease can be complicated by the formation of retention cysts, pulpitis, and periodontitis. Complications from progressive caries are the main cause of tooth loss. According to WHO statistics, the incidence reaches 97%, with children accounting for 35% of the population. The largest number of cases are recorded in economically developed countries.
Types of acute caries
Acute caries is divided into three types:
Acute superficial (or initial)
With this type, patients either do not show any complaints at all, or talk about tooth reactions to chemical irritants - sweet, sour and salty, less often a slight reaction to cold occurs. The reason is the destruction of the enamel, a violation of its mineral composition. A carious spot is visible, which has already passed into the stage of a shallow hole that has not yet passed beyond the boundaries of the enamel. An x-ray shows a superficial enamel defect.
Spicy medium
This type of caries is characterized by complaints of local short-term pain associated with exposure to a temperature or chemical irritant. The enamel has already been destroyed, further degenerative processes occur in the deeper layer of the tooth, dentin. You can see a hole that has destroyed all the enamel and moved to the border with dentin or to the dentin itself, this can be seen on the x-ray.
Spicy deep
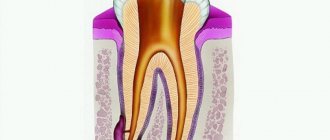
The most neglected option. Characterized by pain in response to chemical, thermal and mechanical stimulation. Upon examination, softened dentin is noticeable, which lines the resulting carious hole. The x-ray shows a significant defect in which the dentin layer is separated from the tooth cavity.
Classification and stages
The development of caries goes through several successive stages. The disease is classified not only by stage, but also by location and cause of occurrence. The stages of caries are of particular importance:
- Stage I. Formation of stains and clouding of the enamel layer. There are no visible destructions, the tissue structure is not changed. Sometimes the spot disappears on its own, which is associated with increased immunity.
- Stage II. Superficial caries. The enamel undergoes pigmentation, and when examined with instruments, a softening of the structure is felt. Often, superficial damage to a tooth covers all layers of enamel, but is limited. Dentin is still not involved in the pathological process. Visually, a carious defect looks like a dark gray spot with a rough base.
- Stage III. Average caries. The defect becomes pronounced, the lesion covers all layers of enamel and part of the dentin. Patients are increasingly noticing bad breath and discomfort when drinking or eating.
- Stage IV. Deep caries reaches the pulp membrane and is accompanied by tooth sensitivity, pain during chewing or at rest. The pain radiates to the temporal regions. The pain can be acute, throbbing, moderate, persistent. It intensifies and subsides involuntarily.
Typically, patients seek help from a doctor when symptoms worsen the quality of life and the dental-root system atrophies. When examining the oral cavity, caries is classified into:
- localized or generalized;
- acute or chronic;
- complicated or uncomplicated.
Carious lesions can be primary or secondary. In the first case, the disease occurs for the first time, in the second, caries develops again, under a filling, crown, bridge, or veneers. Clinically, there is another classification of caries according to Black:
- Class I or fissure caries - characterized by deepening of the natural grooves of the enamel on the chewing surface;
- Class II or carious defect of molars - the formation of defects on the contact surfaces of premolars, molars;
- Class III - damage to the canines and incisors without the defect extending to the cutting edge;
- Class IV - the edges of the canines and incisors are involved in the pathological process;
- Class V - the formation of cervical caries in any group of teeth.
Other types of caries are described in the international classification of diseases. There are unspecified or other caries, odontoclasia (atrophy of the root part of milk teeth), stopped caries after hygienic cleaning, preventive sanitation of the oral cavity.
How to distinguish between cervical caries and wedge-shaped defect
Wedge-shaped defect before and after treatment
These pathological processes are similar, but there are a number of significant differences between them. A wedge-shaped defect is a non-carious process. The main reason for its development is the incorrect distribution of mechanical load on the teeth due to occlusion pathology, periodontal disease and endocrine pathology. It is necessary to distinguish cervical caries from a wedge-shaped defect, since these diseases require different approaches to treatment.
Differences:
- wedge-shaped defect (CD) is localized more often on the lateral teeth (canines and molars), which have a high chewing load, and cervical caries (CC) - on the anterior ones;
- externally, the CD initially appears as a small yellowish area on the front surface of the neck of the lateral tooth under the gum; the enamel is not altered or rough; then a gradually deepening V-shaped defect appears; PC is first a white spot, then a black-brown carious cavity;
- CD lasts for years and decades, while cervical caries can reach a deep stage in a matter of weeks.
Causes
Caries is the result of the activity of pathogenic microflora in accumulated plaque or tartar. A person’s immune status plays a major role in the development of carious defects. At particular risk are persons with autoimmune pathologies, AIDS, HIV, metabolic disorders, diabetes mellitus, and those taking immunosuppressive therapy for organ or tissue transplantation for a long time. The following factors can contribute to the development of caries:
- smoking, alcoholism;
- inadequate oral hygiene;
- natural aging (decrease in the body’s defenses, changes in the biochemical properties of saliva);
- metabolic disorders;
- endocrine pathologies;
- lack of food discipline (including prolonged fasting, poor nutrition, anorexia, bulimia);
- gum recession of various nature;
- excessive consumption of sugar and carbonated drinks;
- gastroesophageal reflux;
- bite pathologies;
- violation of hygiene rules when wearing braces and other orthodontic structures for the treatment of pathological occlusion.
Despite the variety of causes, eating disorders, bad habits and organ pathologies are the main etiological triad leading to the development of caries. Caries is not an independent disease. The pathogenetic link in the demineralization of enamel and destruction of the tooth body is a violation of the body's defenses.
What to do if a tooth hurts after treatment of cervical caries
If a slight pain after removal of cervical tooth caries lasts 2–3 days and gradually subsides, then this is normal. If there is severe, increasing pain, as well as an increase in body temperature or malaise, you should immediately consult a dentist. Possible reasons:
- insufficiently thorough treatment of the carious cavity before filling led to the spread of infection and relapse of the disease, including perforation of the dentin barrier, penetration into the pulp and the development of a complication - pulpitis; the dentist will remove the filling, open the tooth cavity and treat pulpitis; and only then can it be re-sealed;
- periodontitis (inflammation of the periodontal tissues) – the gums become swollen, painful, their edges move away from the crown, and bleeding may occur; this condition also requires dental treatment.
Symptoms
Symptoms of caries are determined by its stage and location. Patients practically do not notice the initial stage of the disease, especially if the affected area is outside the smile line or on the inner surface of the tooth. However, pay attention to:
- enamel roughness;
- change in shade;
- minor defects (deepening of fissures, cavity fragments).
As the carious process develops, defects become noticeable upon visual inspection, and the cavities deepen. Patients note an unpleasant odor from the mouth, even stench, mainly in the morning. Pain appears. When the first signs of caries appear, you should consult a doctor.
Acute caries affects several teeth at once. The enamel softens, crumbles, and the focal fragment has an irregular asymmetrical contour. Soreness accompanies a person almost all day. There is an acute form of generalized caries, when almost all teeth or several units in the jaw row are involved in the pathological process.
In chronic cases, enamel pigmentation comes to the fore. Destruction is sluggish, pain occurs rarely.
Lack of treatment for chronic caries naturally leads to the destruction of the pulpous membrane and the pulp tissue itself, and the formation of a cystic component.
Diagnosis of multiple caries
If the above-described symptoms appear in a child’s oral cavity, parents should definitely visit a doctor with him. Even if the dark spot is small in appearance, there may be a large carious cavity underneath it.
The specialist will examine the dentition and take measures to confirm or deny the diagnosis. For this, a dental mirror and probe are sufficient.
If necessary, the doctor will order an x-ray or use the transillumination method: using bright light to highlight dark carious cavities inside the teeth. If multiple caries is confirmed in a child, a number of therapeutic measures are prescribed.
General recommendations for treatment
Traditional preparation of the defect is carried out using a drill. If the carious cavity is located within the dentin and does not affect the pulp, then after thorough cleaning, a filling is applied. However, sometimes with a small cavity, applying a multi-layer filling (insulating pad + filling material) is impossible. This feature is taken into account when treating caries on the contact surface of premolars and molars.
Another way to treat shallow caries in dentistry is to use a composite material with adhesive properties. In this case, extensive preparation and creation of a wide cavity is not required. Another method involves polishing a carious defect with remineralization of the enamel with medicinal applications, electrophoresis with a 1% sodium fluoride solution and other approved medications.
Medium caries is treated only by deep preparation and filling. In this case, the cavity is cleaned until the affected tissue is completely removed. High-quality sanitation ensures reliable fixation of the filling and increases its service life.
How is pulpitis treated?
Pulpitis can be treated biologically or surgically. The first is applicable if the disease is in its early stages. The dentist strives to preserve the pulp by eliminating only the inflammation. If possible, pulpitis of primary teeth is treated using a biological method, when it is especially important to preserve the tooth root. Treatment is carried out in several stages. First, the dentist prepares the carious cavity, opening it as wide as possible. Then he treats it with an antiseptic, puts a swab with an antibacterial agent and covers the tooth with a bandage. During the next appointment, if the patient has no complaints, the cavity is treated with medication, filled with a special composition that stimulates dentin production, and a temporary filling is placed for a period of 5 to 7 days. During the third appointment, the dental crown is filled.
When the biological method of treating pulpitis is ineffective, surgical treatment is used. In this case, the inflamed neurovascular bundle is removed completely or partially. Without a nerve, a tooth becomes unviable and its service life is reduced.
Surgical treatment is performed with local anesthesia. First, the carious cavity is prepared, the pulp is removed, the affected area is treated with an antiseptic, medication is injected, and first the root canals are filled, and then the dental crown. As with the biological method, surgical treatment is carried out over several visits to the dentist.
If pulpitis is not treated, it will progress and can lead to very serious complications:
- flux - inflammatory process in the periosteum;
- periodontitis - inflammation of the tissues surrounding the tooth;
- pulp necrosis - death of its cells;
- sepsis is a blood infection that can develop when an infection enters the bloodstream.
You can avoid such complications if you do not delay your visit to the dentist and begin treatment for the disease at the first symptoms.
Features of the treatment of deep caries
Removing a carious cavity with deep damage to dental tissue is fraught with difficulties, and the choice of method depends on the degree of destruction of your own tooth. Treatment tactics:
- With pulpitis. Pulp damage involves deep preparation and removal of the nucleus pulposus along with nerve endings from the root canals. An antiseptic is placed into the lumen of the root canal, and the cavity is closed with a temporary filling or medication. This is necessary for etching and eliminating a secondary infectious process. After 1-3 days, the root canals are filled, and the defect is covered with a composite material.
- No pulp damage. Sometimes, with deep damage, the pulp remains intact, covered by a small layer of intact dentin. Preparation is carried out precisely to this tissue in order to preserve the integrity and functionality of the root system. Often the therapist has to leave this part of the dentin, despite its softening, friability and pigmentation. In such cases, a pad based on paste-like calcemin is placed at the bottom of the defect for antiseptics and restoration of dentin. An insulating gasket and a permanent filling are also placed into the defect cavity.
In case of significant tooth decay, patients are recommended to restore the body of the unit with a composite material. This method is not considered durable due to abrasion, destruction, and the formation of new carious cavities. The only alternative in particularly difficult cases is implantation, microprosthetics or prosthetics with a bridge structure.
A dangerous complication of caries is pulpitis.
The most common consequence of untreated caries is pulpitis. It occurs when the infection extends beyond the tooth and spreads to the pulp - the neurovascular bundle, or dental nerve.
The pulp contains nerves and blood vessels and provides nutrition to the dental tissues. Therefore, with pulpitis, the tooth may lose vitality. In severe cases, inflammation spreads to neighboring tissues.
A characteristic symptom of pulpitis is acute, prolonged pain that is difficult to tolerate. It often has a pulsating nature and can radiate to the temple, ear, or throat. The peculiarity is that attacks of pain appear at certain intervals, last about 5 minutes, and can intensify when lying down. It is necessary to begin treatment of pulpitis as quickly as possible.
Rules for selecting and making a filling
The key to success when applying a high-quality and durable filling is to follow the technology of its preparation. Even when using high-quality materials, violation of the manufacturing and application protocol sharply reduces its performance characteristics.
The choice of filling depends on the location of the tooth in the dental system, the strength of the chewing load, and the characteristics of the bite. So, if it is necessary to treat teeth along the smile line, the filling should not only be durable, but also aesthetically pleasing and inconspicuous. Dentists choose composite materials, silicates.
Filling a carious cavity as the final stage is performed only after complete cleansing of the prepared area, removal of dentinal fragments, and drying. The absence of moisture and organic sawdust increases the contact of the filling with the natural tooth tissue. After the filling is fixed and completely hardened, the doctor grinds and adjusts it to the anatomical shape (removes excess material, shapes the edges). Once the filling is comfortable for the patient when closing the jaws, it is polished.
Special attention is paid to polishing. The better the filling is polished, the lower the risk of developing recurrent caries. The uniformity and smoothness of the coating prevents corrosion, accumulation of plaque and tartar, and further destruction.
The danger of decompensated form
Acute caries is dangerous for many reasons. The advanced form of the disease often leads to the following problems:
- development of pulpitis and periodontitis;
- development of periodontitis;
- tooth splitting;
- tooth loss.
In addition, the decompensated form is a signal of a disruption in the functioning of the entire organism. Untreated caries is often a consequence of decreased saliva production and a decrease in its bactericidal properties, which affects the general condition of the oral cavity as a whole. In pregnant women, this can affect the general physical condition of the expectant mother and the health of the fetus.
Modern methods of caries treatment
Modern technologies for the treatment of caries are based on reducing the invasiveness and aggressive effects of the drill and hard attachments and brushes. Minimally invasiveness and comfort during treatment are especially important in pediatric dentistry. Popular methods:
- ICON technology. Suitable for the treatment of caries at the chalk spot stage. Rehabilitation of the defect is carried out using the unique ICON resin, which has an antibacterial and regenerating effect. The component literally fills the pores in the enamel layer and prevents the further development of the pathological process. The procedure itself lasts no more than 20 minutes.
- Ozone therapy. Triatomic gas ozone is a natural oxidizing agent with high antibacterial properties. The substance removes pathogenic microflora and cleans the tooth surface of plaque. Ozone treatment is indicated for early stages of caries, as well as for superficial demineralization of enamel on molars and the cutting surface of teeth. In the treatment of complex cases, ozone treatment is auxiliary.
- Air abrasive processing. Dental sanitation is carried out using finely dispersed abrasive particles under pressure. This method eliminates the use of a drill and does not injure dead tooth tissue.
- Laser treatment. A minimally invasive treatment method that in most cases replaces a drill. The exclusion of traditional preparation of a carious cavity is possible only in case of superficial caries. Despite the fact that sanitation occurs with a laser beam, patients require anesthesia. During the removal of affected dentin, the laser somehow reaches the pulp and causes acute pain.
- Art methodology and artistic restoration. Non-traumatic cleaning of the defective cavity is performed mechanically, followed by filling with glass ionomer material. The method was developed in underdeveloped countries where it is not possible to open full-fledged dental clinics with a wide range of services. Manual cleaning helps to accurately remove affected tissue while preserving the thickness of the healthy part of the tooth as much as possible.
All methods of caries treatment are widely used in modern clinics, but are not advanced. Most often, dentists sanitize pathological cavities and remove dental defects using a drill.
Why is caries dangerous for the heart and blood vessels?
When brushing your teeth, there is a risk of injury to your gums. This can happen due to a brush that is too hard, careless use of dental floss, or sensitivity of the gums themselves. One way or another, cariogenic bacteria enter the resulting wounds, which can be carried throughout the body by the bloodstream. If they get into the tissue of the heart, inflammation of its valves may develop - infective endocarditis.
Studies show that with advanced caries, the risk of developing cardiovascular pathologies increases by 70%. When bacteria enter the blood, they settle on the vascular walls next to atherosclerotic plaques. As a result, the plaque begins to actively grow and can clog the vessel, disrupting normal blood flow. The most dangerous consequences can be thrombosis, stroke, heart attack, atherosclerosis.
Alternative medicine in the fight against caries
Caries can be eliminated at home only at the initial stage of destructive changes in the enamel. Non-traditional recipes can stop the progression of tooth decay, especially if treatment is currently difficult or impossible according to indications. Popular rinse recipes:
- Sage decoction. 1 tbsp. raw materials, pour 200 ml of boiling water, infuse until a bright amber-brown hue is obtained, filter and rinse your mouth throughout the day. The plant kills pathogenic microflora and is effective against stomatitis and periodontal disease. You can make lotions with a decoction of sage by applying a gauze pad to the affected area.
- Infusion of calamus roots. A steep tincture of calamus root helps relieve pain and slow down the development of superficial or medium caries. To prepare, you will need to pour 1 tbsp. crushed raw materials, 200 ml of vodka, alcohol solution of propolis. For greater effect, you can add 10 drops of tea tree ether. The resulting composition is placed in a dark place for 5-7 days. Before rinsing 1 tsp. alcohol infusion is combined with 100 ml of warm water.
- Mint based recipe. Fresh mint leaves are pounded in a mortar, poured with hot water (not boiling water!), and left for 30 minutes. Then add 1 tbsp. apple or wine vinegar and leave for 3 days. Mint essence prevents further destruction of dental tissue, removes plaque, softens tartar.
You can rinse your mouth with a solution of soda, sea salt, or an aqueous or alcoholic decoction of propolis. Camphor or fir oil, zinc-salicylic paste can be applied to the carious cavity.
Types of caries by location of the lesion
Fissure.
Occurs on grooves and fissures (indentations on chewing teeth).
Contact.
Appears between two teeth and affects both teeth at once. This area is the most difficult to clean.
Cervical.
It forms in the neck of the tooth, closer to the gum.
Circular.
Affects the upper part of the incisors. Caries seems to wrap around the tooth horizontally.
Multiple.
An acute form of caries, when lesions develop on several teeth at once.
Single.
The most popular type. Caries affects only one tooth, without affecting the surrounding tissue.
Decompensated.
A form of the disease in which carious lesions progress beyond established norms.
Preventive actions
Prevention of caries consists of high-quality removal of tartar and plaque using special means: toothpastes, rinses, flosses, irrigators. Prevention of caries in children comes down to early instillation of oral hygiene skills. Popular recommendations:
- annual dental examination;
- professional teeth cleaning to remove tartar and plaque at least once a year;
- taking vitamins and calcium-containing medications;
- normalization of diet;
- improving food quality, balanced diet;
- timely treatment of chronic diseases of internal organs and systems.
Persons with chronic diseases of the ENT organs, prone to colds and respiratory infections, should take immunomodulators in courses. In case of a burdened dental history or hereditary predisposition, special pastes with a high concentration of fluoride are recommended. For recurrent caries, periodic application of mineralizing, antiseptic and protective drugs and varnishes to the enamel is indicated.
If you have braces, orthodontic aligners or plates, you should use an irrigator and special brushes. However, even careful care does not exclude professional cleaning of the product and teeth from plaque 2-3 times a year.
Timely treatment of dental caries preserves the integrity of the unit, prevents its early loss and complications. Regular sanitation of the oral cavity improves the quality of life, the aesthetics of a smile, and self-confidence.
Prevention
Fighting soft plaque helps prevent tooth decay. For this it is important:
- use high-quality toothbrushes and toothpastes;
- use dental floss (removes food debris between teeth);
- When brushing, pay attention not only to the teeth, but also to the tongue, gums, and the inner surface of the cheeks;
- regularly undergo professional oral hygiene procedures;
- limit your consumption of sweets (it is better to replace sweets with dried fruits);
- pay close attention to the temperature of food and drinks (the enamel may not withstand it and become covered with microcracks from temperature changes, for example, when eating ice cream with coffee).
People often do not think that harmless caries leads to serious consequences (including tooth extraction). Going to the dentist for preventive examinations is faster and cheaper than delaying the “X moment” for several years, and then ending up straight in the surgical chair.
Back
Granuloma
Granuloma is advanced periodontitis. Symptoms of the process:
- A purulent sac in the periapical area, which is visible on x-ray.
- The process does not give a clearly defined clinical picture for a long time.
- If the process worsens, then unbearable pain is observed.
Treatment consists of delayed filling of the root canal with a temporary calcium-based filling material. This material in the canal used for filling is periodically renewed, usually after six months the granuloma resolves. If not, then a resection of the apex of the tooth root is performed, along with the granuloma.