Many people have faced this dilemma at least once in their lives. When making a decision, people base their decisions on personal experience, the opinions of friends and acquaintances, and actively search for information on the Internet. If you ask whether it is possible to treat teeth if your throat hurts badly , you get the following answers:
- yes, treat it, because the tooth hurts, and enduring pain is harmful;
- no, you will infect the doctor, and the recovery process after treatment will be delayed.
Interestingly, both sides can be equally right and wrong. Often a sore throat and toothache are related, being the root causes for each other. All that remains is to determine what started to bother you first—the throat or the teeth.
Are sore throat and dental treatment compatible?
Why can wisdom teeth hurt?
Currently, dentists consider the third molar to be a vestigial organ, which in the process of evolution has lost its functional load and relevance. For ancient man, it served to chew hard food, which is practically absent in the modern diet, which means there is no longer any need to use the wisdom tooth when chewing. This fact is supported by the presence of approximately 10% of the planet's population, whose representatives do not have eights at all, which is not a pathology. The remaining 90% of the population faces unpleasant wisdom tooth problems. The third molar can hurt and bother you for various reasons.
When teething
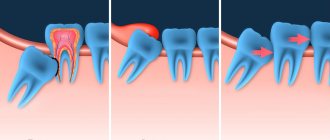
By the age of 18–25, a person’s jaw is already formed. And, naturally, when a wisdom tooth is cut, it may simply not have enough space in the dentition. The eight begins to put pressure on the seven in front, which in turn puts pressure on the sixth molar, etc. As a result, the entire jaw hurts and “aches.”
Often the third molar does not find a place for itself in the dentition and begins to grow dystopically - it deviates to the side, turns around its axis, moves forward or backward. In this case, the gums near the wisdom tooth hurt and inflammation may occur. Not to mention the fact that in adulthood the gums have a fairly dense structure, the resistance of which must be overcome by the figure eight. And in order to erupt safely, it literally tears the soft tissue. Naturally, this process is accompanied by pain and discomfort.
For dental disease
An already formed wisdom tooth will hurt if it is susceptible to any disease. The most common are caries, pulpitis and periodontitis.
- Caries is a pathological process that leads to the destruction of hard tooth tissues, which is initially accompanied by increased sensitivity of the enamel, and subsequently severe pain in the wisdom tooth.
- Pulpitis - inflammation of the internal tissue of the figure eight (pulp) is a consequence of untreated caries. In rare cases, infection enters the pulp through the apical foramen, which may be due to improper position of the molar. With pulpitis, the wisdom tooth hurts very much, since the pulp is penetrated by a large number of nerve endings.
- Periodontitis - inflammation of the periodontium (connective tissue surrounding the tooth) can be caused by injury to the gums or infection during the eruption of the figure eight. In this case, localized, constant pain is observed, which gradually increases and becomes pulsating, which indicates a purulent course of the process.
Important! If an already erupted wisdom tooth suddenly begins to hurt, then you need to show it to the dentist as soon as possible. Timely diagnosis will avoid infection of the pulp, periodontium and the development of complications.
For pericoronitis
Pericoronitis - inflammation of the soft tissue of the gums surrounding the erupting figure eight, is the most common. The problem is that when a wisdom tooth comes in, it first cuts through the mucous membrane with its tubercles, forming a so-called “hood” above itself - part of the gum. Thus, partly the third molar is already visible, and partly is still covered by the “hood” of the gums. Hanging over the figure eight, it creates favorable conditions for the accumulation of food particles, plaque, and microbes, which, sooner or later, leads to inflammation. The development of pericoronitis will also be accompanied by pain.
Important! If the gum above the wisdom tooth forms a “hood” and is inflamed, then it must be excised (removed). The procedure is carried out in the sterile conditions of a dental clinic.
How long will the cutting and toothache last?
The process of cutting through the figure eight is long and highly individual. In some patients it “appears” in 3–4 months, in others it may take 1–2 years, and in others it remains incompletely erupted. Quite often, a wave-like “appearance” of the third molar is observed - either it is intensively cut, or it freezes.
As for severe pain, as a rule, it is present only at the beginning of the process - at the stage when the figure eight cuts through the dense gum tissue. And again, this moment can happen quite quickly or drag on for a long time.
When the first signs of figure eight eruption appear, it is better not to postpone a visit to the doctor. Even if the process does not cause severe pain or discomfort, it is better to show it to the dentist. An experienced specialist will examine the condition of the third molar and provide assistance that will facilitate the process of “the birth of the tooth.”
Symptoms of wisdom tooth inflammation
To prevent a problem, you need to immediately notice the symptoms that cause it. To do this, special attention should be paid to the following points:
- there is a prolonged tugging pain;
- the gums become hard;
- the adjacent tooth becomes loose;
- body temperature rises;
- lymph nodes enlarge.
To alleviate his condition, the patient can take an analgin or paracetamol tablet at home before visiting a doctor, rinse his mouth with an antiseptic, and use only liquid food for nutrition.
If the pain is severe, you can take a painkiller pill, but you cannot suppress the pain with pills for a long time. You still need to go to the dentist.
How to understand that a wisdom tooth is cutting?
It's not difficult to understand. Normally, this process is accompanied by discomfort, engorgement and slight swelling of the gums in the place where the tooth is cut. At the moment of eruption, increased salivation, a feeling of fullness and tolerable pain will be observed. They can intensify during eating and hygiene procedures. Visually and by touching the tongue, you can see and feel the protruding tubercles of the figure eight.
In the pathological course of the process, the following symptoms may join the above-described symptoms.
- Redness and swelling of the gums indicate inflammation of the “hood”.
- It hurts to open your mouth - the inflammation process is progressing and has spread to the masticatory muscle.
- It hurts to swallow - a symptom indicates the presence of purulent inflammation of the soft tissues closer to the tongue.
- High temperature - the inflammatory process progresses.
- The third molar, the adjacent tooth and gums are very painful - most likely, the figure eight is growing in the wrong direction.
Additionally, symptoms may occur depending on the location of the wisdom tooth.
- The upper eights can erupt towards the cheek and injure its mucous membrane, causing pain.
- The lower molars often form a “hood” and grow with an inclination towards the seven, forming a gap. It is difficult to clean with a brush. Over time, a stable plaque and tartar form in it, which leads to the development of caries.
You should not trust various kinds of myths, they say, the appearance of a wisdom tooth is always excruciatingly painful, very problematic and you just need to endure it. It is not true! Normally, the process does not cause excruciating pain and passes with tolerable discomfort. On the contrary, problem eights hurt a lot, provoking the development of inflammation and complications. Therefore, it is better not to delay visiting the dentist.
What to do if your gums hurt
Treatment of inflammatory diseases of the gums and periodontium is one of the most pressing problems in dentistry10. Regardless of the diagnosis, thorough brushing of teeth and sanitation of the oral cavity are mandatory steps2.
If a patient has gum pain, the doctor determines how to treat it, depending on the cause of the disease: for candidiasis, antifungal drugs are used, and for a bacterial infection, antibiotics are used. Sometimes it may be necessary to remove tartar, replace fillings, or surgically repair the frenulum or vestibule2.
Since inflammatory diseases of periodontal and gums are classified as infectious, normalization of the microflora of the oral cavity is an essential element of treatment10.
Dental gel for gums with antimicrobial action METROGIL DENTA®11 can be used in therapy. The product is characterized by antiseptic and anti-inflammatory effects6. Indications for use11:
- Acute and chronic gingivitis.
- Acute ulcerative-necrotizing gingivitis of Vincent.
- Acute and chronic, as well as juvenile periodontitis.
- Periodontal disease complicated by gingivitis.
- Aphthous stomatitis.
- Cheilitis (inflammation of the lips).
- Inflammation of the oral mucosa due to wearing dentures.
- Alveolitis.
- Periodontitis, periodontal abscess (as part of complex treatment)11.
The effect of the gel is provided by a combination of 1% metronidazole and 0.25% chlorhexidine in stable concentrations10,11
According to studies, already 30 minutes after applying METROGYL DENTA®, the number of pathogenic bacteria significantly decreased10. It has been shown that with mild forms of gingivitis and periodontitis, the oral microflora is normalized after 2-3 applications of the gel, with moderate periodontitis - after 3-5 procedures, and with severe periodontitis - after 5-7 procedures10. According to the results of the study, after using the drug, most patients note the disappearance of pain and itching in the gums, and the absence of bleeding10.
Top
Does it make sense to treat wisdom teeth?
An experienced and self-respecting dentist will always fight for every tooth to the last. And wisdom teeth in this case are no exception. After all, no one knows how the patient’s life will turn out in the future. Perhaps in the future he will need prosthetics, and the figure eight will be used as a supporting tooth for installing a prosthesis. Therefore, if the appearance of a third molar does not pose a threat to neighboring teeth and oral health, the dentist will take actions aimed at facilitating the process and preserving the tooth. Well, unless, of course, the patient insists on its removal.
If the current situation is serious, then removal of the wisdom tooth is inevitable. Including in those cases when the figure eight does not hurt much (or does not hurt at all), but is covered with caries and is gradually destroyed. It is more rational and safer to remove such a tooth and forget about the problems.
Causes of gum disease
If your gums hurt, then naturally you want to know why this is happening. In the development of diseases of the oral mucosa, factors such as diet, smoking, drinking alcohol, and poor-quality orthopedic structures in the mouth play an important role1.
Another important point is the quality of dental care. Poor hygiene leads to the accumulation and attachment of pathogenic microbes to the gums, which penetrate the mucous membrane and trigger the inflammatory process1.
Causes of gum disease3:
- Injuries (exposure to mechanical and temperature factors, radiation, chemicals).
- Infections:
- general infectious diseases (syphilis, HIV infection);
- actually infectious and parasitic diseases of the mucous cavity
mouth (herpes virus, streptococci, staphylococci, candida).
- Allergies.
- Autoimmune diseases.
- Intoxication.
- Pathologies of organs and systems, metabolic disorders:
- diseases of the endocrine and nervous systems;
avitaminosis;
- diseases of the blood and hematopoietic organs.
- Treatment of oral diseases3.
Top
When do you need to see a dentist urgently?
Contacting a dentist is required in the following cases.
- Pericoronitis
– the “hood” will be excised. - The figure eight puts pressure on neighboring teeth
- it needs to be removed. - Initial caries
– treatment will be carried out. - Medium, deep caries or rotten tooth
- a clear removal of the figure eight. - The wisdom tooth is loose
- a diagnosis of its condition will be carried out, according to the results of which the molar will be treated or removed. - Pulpitis
– if the root canals are passable, they will be filled.
This list should also include the above symptoms of pathological teething - pain when opening the mouth, swallowing, high temperature. If they appear, you should contact your dentist immediately, since this is a serious inflammatory process, the localization of which requires adequate treatment.
The reason for contacting a specialist may also be the “normal behavior” of the number eight. In this case, the doctor will simply make a small incision on the gum, thereby facilitating the eruption of the wisdom tooth. After a simple procedure, the process will be less painful, and the incision site will heal quickly, after pain for 2 to 4 days.
When should a tooth be removed?
Direct indications for wisdom tooth removal are the following pathologies and conditions.
- There is no place in the dentition for a number eight.
- Dystopic tooth (molar occupies an anatomically incorrect position).
- The appearance of wisdom teeth threatens the molars in front.
- Severe forms of caries that destroy the tooth.
- The third degree of mobility of the figure eight.
- Upcoming installation of braces.
If removal is not carried out, the development of complications is inevitable. The number eight will destroy adjacent teeth and provoke the development of pulpitis, periodontitis, and extensive caries. Eventually it will fall out on its own, but at too great a cost to the patient.
There is no need to be afraid of wisdom tooth removal. Depending on the complexity of the problem, third molar extraction will last from 20 minutes to 2 hours. The operation is performed using local anesthesia or sedation, which ensures that the procedure is painless.
Diseases that cause gum pain
Stomatitis
Stomatitis is an inflammation of the oral mucosa, manifested in the form of redness, swelling, white lesions or ulcers.
The causes of stomatitis can be a local infectious process, systemic pathologies, the influence of a physical or chemical irritant, allergies4.
One of the most common dental diseases affecting the oral mucosa is chronic recurrent aphthous stomatitis3. According to WHO, this problem occurs in 20% of the population6. This form of stomatitis is characterized by alternating periods of remission and exacerbation with the appearance of aphthae on the mucous membrane and gums - round or oval lesions covered with white fibrinous plaque5.
The cause may be allergens (food, toothpaste components, dust, worms and their waste products, medications), disorders of the gastrointestinal tract, respiratory infections, pathologies of the nervous system, hypovitaminosis6.
There are two main forms of chronic aphthous stomatitis—mild and severe3,5,7.
The mild form begins with the appearance of swollen and reddened round or oval spots on the mucous membrane, which cause pain and burning. After 1-2 hours, these areas rise above the mucosa, and after a few hours, aphthae appear in their place, covered with a dense grayish-white fibrous coating. When you touch them, you feel a sharp pain3,5,7.
As a rule, with this form 1-2 aphthae appear, rarely more. Most often they are localized at 5:
- buccal mucosa;
- lips;
- the tip of the tongue and its lateral surfaces.
The occurrence of aphthae may be accompanied by inflammation of the lymph nodes and fever7.
After 2-4 days, the rashes are cleared of plaque, and within another 2-3 days they heal. Recurrence of aphthae is possible either 1-2 times a year or more often, depending on the severity of the disease3,5,6.
Exacerbation can be triggered by factors such as:
- local trauma;
- stress;
- overwork;
- previous viral infection;
- premenstrual syndrome.
Top
Gingivitis and periodontitis
Inflammatory or destructive processes in the tissues surrounding and holding the tooth in the jaw (gums, periodontium, bone, cement), as a rule, begin with gingivitis - inflammation of the gums, which can develop into periodontitis - inflammation of the gums and periodontium with further destruction of the bone of the interdental septa2.
Gingivitis causes swelling and bleeding of the gums; they hurt and ache when eating and brushing teeth2,3. In the absence of proper treatment, gingivitis turns into periodontitis - periodontal pockets deepen, bad breath appears, and teeth begin to loosen. At a later stage, tooth loss may occur2. The cause of the development of gingivitis and periodontitis in most cases are microbes that attach to the surface of the tooth above and below the gum, forming the basis of plaque3. Bacterial waste products - toxins and enzymes - cause inflammation in the gums3.
Top
Alveolitis
Alveolitis is a common complication after tooth extraction, when the bone socket is not filled with a blood clot, but remains empty, and infection penetrates there8. The main causes of development are pathogenic microbes that live in periodontal tissues and trauma associated with complex tooth extraction9.
With alveolitis, 1-3 days after tooth extraction, the gum under its socket becomes red, swollen and painful. The pain may radiate to the temple and ear areas. General manifestations are also possible - increased body temperature, sleep disturbances, enlarged and painful lymph nodes9.
Top
How to relieve pain?
When visiting the clinic, the attending physician gives valuable recommendations that will help relieve the process of the “appearance” of the figure eight. If you decide to act on your own, you can use the following medicines and folk remedies.
Pills and medicines
- Tablets: “Nimesil”, “Analgin”, “Solpadein”, “Tempalgin”, “Ketanov”, “Paracetamol”, “Ibuprofen” are used according to the instructions.
- Gels and ointments: “Cholisal”, “Kamistad”, “Kalgel”, “Metrogil Denta” are applied to the site of tooth eruption.
- Solutions: “Chlorhexidine”, “Miramistin” and “Furacilin” are used for antiseptic treatment of the oral cavity.
Folk remedies
- Soda, saline or soda-salt solution - 1 teaspoon of product for 1 glass of warm water, stir until completely dissolved, rinse the problem area every 2 - 3 hours.
- Sage, calendula, plantain, St. John's wort - to prepare a decoction, pour 1 tablespoon of the product into 1 glass of boiling water, leave for 20 - 30 minutes, use for rinsing every 2 - 3 hours.
Home methods of pain relief will be effective if there are no serious problems with the eruption of the figure eight. If inflammation occurs, the tooth is rotten or very loose, then they will not help, but will only aggravate the problem, which will lead to the development of complications.
Wisdom teeth removal with 20% discount
Moscow
Which doctor should I contact?
Only a dentist can accurately answer the question of what to do if your gums hurt. Many people, faced with gingivitis, periodontitis, diseases of the oral mucosa and even injuries, self-medicate12. The source of information about medications in most cases is not the attending physician at the appointment, but the Internet, television, radio, as well as advice from relatives and friends12. It is important to understand that self-medication can lead to the development of a number of complications12.
Top
The information in this article is for reference only and does not replace professional advice from a doctor. To make a diagnosis and prescribe treatment, consult a qualified specialist.
Bibliography
- The state of the dental status of the adult population depending on the presence of diseases of the oral mucosa / Mama before in R. M., Alizade A. R., Ibragimova L. K., Gamzaev B. M. // Problems of dentistry. - 2013. - No. 5. - P. 18-20.
- Prevention and treatment of diseases of the oral mucosa. Omarova K.V. // Bulletin of Surgery of Kazakhstan. - 2011. - No. 4. - P. 128.
- Therapeutic dentistry. Textbook / Borovsky E. V. Ivanov V. S., Maksimovsky Yu. M., Maksimovskaya L. N. / Moscow, 2011.
- Stomatitis. MSD Handbook. Professional version - URL
- Main diseases of the oral mucosa. Borodovitsina S.I. et al. /Ryazan: Atlas, 2022.
- Chronic recurrent aphthous stomatitis. Maltabarova B. A. // Bulletin of Surgery of Kazakhstan. - 2011. - No. 3. - P. 106.
- Chronic aphthous stomatitis in the practice of a dental therapist (literature review). Kosaeva Sh. K. // Bulletin of the Kazakh National Medical University. - 2014. - No. 1.
- A new word in the treatment of alveolitis. Shlegel Yu. V., Hartman R. V. // Medico-pharmaceutical journal “Pulse”. - 2007. - No. 4. - P. 412-413.
- Prevention and treatment of alveolitis / Rodionov N. T., Andreeva E. P., Dobrorodova S. V., Stoletnaya T. P. // Bulletin of the Smolensk Medical Academy. - 2010. - No. 2. - P. 110-111.
- Dental gel for gums “Metrogil Denta®” in the treatment of periodontal diseases and oral mucosa // Practical Medicine. - 2009. - pp. 105-106.
- Instructions for medical use of the drug METROGYL DENTA®.
- Self-treatment of periodontal diseases and oral mucosa. / Tsepov L. M. et al. // Bulletin of the Smolensk State Medical Academy. — 2022.
Where can the pain go?
Quite often, the process of growth of eights is accompanied by uncharacteristic symptoms. Moreover, some of them are due to the growth of the molar itself, and the other part indicates the development of complications. Let's take a closer look - can a wisdom tooth give into...?
- Head
- in case of complicated teething it can. - Eye
– with complicated eruption of the upper molars and the development of an abscess, it can. - Tongue
- a symptom indicates the presence of purulent inflammation of the soft tissues closer to the tongue. - Ear
– indicates the development of inflammation, pulpitis or dental cyst. - Throat
- most likely we are talking about pulpitis. - Jaw
- a symptom characteristic of complicated teething and inflammation. - The neck
is unlikely, unless we are talking about the spread of infection and inflammation of the lymph nodes. - Temple
– Clicking and pain in the temple may be present due to tension in the temporomandibular joint, which occurs from constant pain. - The teeth are nearby
- of course, because the figure eight can put pressure on them.
Important! The above list is a serious signal to contact a dentist. Don't delay your visit to the clinic!