Causes
In many cases, the formation of ulcers in the facial area contributes to the appearance of inflammatory processes. Staphylococci and streptococci are among the most common pathogens. In accordance with the cause of development, specific and nonspecific lymphadenitis are distinguished. The development of the former can be caused by serious diseases such as tuberculosis. The second form develops due to direct penetration of infection into the lymph node. Entry may occur through lesions in the neck. Those people who are at risk include: patients with weak immunity; people whose field of activity is related to animals, dirty waters, etc. As a rule, people over 18 years of age experience this disease.
What contributes to the development of the disease?
There are several factors that contribute to the spread of lymphadenitis in children and adults:
- infection of the nasal and oral cavities,
- dysfunction of the endocrine system,
- HIV,
- severe allergies,
- metabolic disorder,
- excessive consumption of alcoholic beverages.
Cervical lymphadenitis is not transmitted from one person to another, since it is only an additional process that appears as a complication. In accordance with the diseases occurring against the background of this pathology, treatment is prescribed by a certain specialist in his field (surgeon, infectious disease specialist, and so on). Initially, lymphadenitis occurs in an acute form, gradually turning into a chronic form.
causes of cervical lymphadenitis
Varieties
Types of cervical lymphadenitis:
- Penetration of infection into the lymph node (quickly cured, practically does not lead to complications).
- Presence of serious illnesses. In this situation, diagnosis is carried out in the acute form of the pathology.
There are several stages of the disease in acute form:
- Serous. Does not cause intoxication or severe fever. The initial stage of penetration of harmful organisms into the lymph node.
- Purulent. Indicates bacterial infection. Promotes the appearance of high temperature. In this case, surgical intervention is a necessary condition.
- Complicated. In this situation, we are talking about immediate surgical intervention, since the disease can cause infection of the entire body. The disease occurs along with the spread of infections through the lymph nodes. It is worth noting that this form is highly curable and does not cause complications. The development of pathology in other nodes can cause the spread of a serious disease, which is called generalized lymphadenitis.
Why is lymphadenitis dangerous?
{banner_banstat10}
If the infection is not treated, it will continue to spread throughout the body. Prolonged inflammation of the lymph nodes can lead to tissue necrosis, destruction of the lymph nodes, sepsis and serous purulent pathologies.
Complications arising from lymphadenitis:
- thrombophlebitis;
- lymphostasis;
- osteomyelitis;
- encephalitis and meningitis;
- abscesses.
Important! Serious consequences of the disease can include purulent pathologies, disability and even death.
Symptoms
The main symptoms that indicate the presence of lymphadenitis are the following: increased body temperature, insomnia, fatigue, nervous system disorders; indifference to life, poisoning, etc.
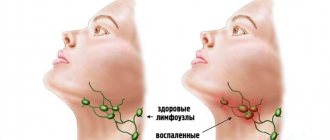
In the initial stage of acute lymphadenitis, thickening of the lymph nodes can be observed. When pressed, discomfort and pain occur. Such signs are considered dangerous, so patients should immediately consult a doctor for advice. Otherwise, further development of a dangerous disease may occur.
Symptoms of the chronic form of the studied lymphadenitis in adults and children include: hardening of the lymph nodes, high body temperature, weakness and fatigue, insomnia, pain when pressing the lymph nodes.
At the stage of the chronic form of the disease, the symptoms become somewhat muted. This is due to the fact that the body reduces the number of mechanisms spent on fighting pathology. As a result, the body is poisoned. Purulent inflammation leads to an increase in the number of external symptoms of the disease, which leads to exacerbation. Purulent inflammation is indicated by intense pain and swelling of the lymph nodes. A similar condition is life-threatening and requires urgent intervention.
lymphadenitis symptoms
Prevention
To prevent inflammation of the lymph nodes, preventive measures should be followed.
These include:
- Timely treatment of bacterial and viral diseases.
- Treatment of purulent skin lesions of any origin.
- Oral care: routine dental consultations, hygiene.
- Breast hygiene, especially during breastfeeding.
- Protection during sexual intercourse to avoid STDs.
- Antiseptic treatment of cuts, abrasions and wounds.
- Correction of immunity with vitamins, diet and special medications.
Inflammation of the lymph nodes is not a full-fledged disease, but an unpleasant symptom that indicates a serious pathology in the body. If not treated on time, lymphadenitis can lead to serious complications and consequences.
Diagnostic methods
neck lymphadenitis detected ? During the examination, the doctor presses on the lymph nodes to determine the cause. A general blood test will provide the necessary information about the course of pathological processes, which are characterized by an increase in the number of lymphocytes.
If the diagnosis is established without the presence of certain complications, the doctor immediately prescribes therapy. However, in cases where the doctor notes disturbances in other systems, it is necessary to conduct additional examinations, which include:
- general and biochemical blood test,
- histology examination,
- x-ray of the chest area,
- Ultrasound of the abdominal cavity,
- immune system examinations and blood tests to check for hepatitis.
In any case, consultation with a specialist is mandatory. An exacerbation of the disease can occur at any time.
Lymphadenitis is inflammatory changes in one or a group of lymph nodes. Lymphatic formations of all areas of the body can be affected. Lymphadenopathy of the cervical and submandibular region is most often observed in medical practice. This disease usually has a secondary genesis. If the inflammation becomes purulent, then the infection may break through with the development of abscesses and phlegmons. From the submandibular region, inflammation can move along anatomical formations to various sections. Such situations can be life threatening.
A huge number of diseases can indirectly or directly lead to inflammation of the lymph nodes, especially infectious diseases. The human lymphatic system belongs to the body's immune system and is represented by lymphatic vessels and lymph nodes. Immune cells circulate in this system. Lymph (fluid that flows from organs and tissues through lymphatic vessels to the lymph nodes) carries particles of pathogenic microorganisms for recognition by immune cells. In the lymph nodes, preparation and activation of immune cells (mainly lymphocytes) take place, which migrate to the pathological focus, destroy bacteria and other pathogens, resulting in recovery. There are other possible causes of lymphadenopathy: tumors of the immune system, systemic diseases, helminthic infestations, tumor metastases and others, but they are much less common and their main symptoms dominate over enlarged lymph nodes (which, by the way, is not always inflammatory in nature). Most often, inflammation of the regional lymph nodes of the submandibular region is odontogenic. This means that the main source of infection is the inflammatory process in the oral cavity. These are most often dental problems - periostitis, periodontitis, periodontitis, pulpitis. Inflammatory diseases of the respiratory system lead to enlargement of the lymph nodes in the cervical region - parotid, tonsillar, occipital and others. There are catarrhal and purulent forms of inflammation. Depending on the type of process, treatment tactics will change.
Having discovered such changes, patients usually first turn to a therapist. However, as mentioned earlier, if the inflammation is localized specifically in the submandibular nodes, one should assume an odontogenic nature and consult a dentist.
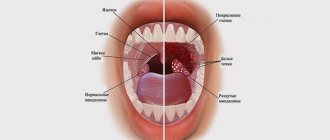
The clinical picture may differ depending on the location of the primary lesion. Lymphadenitis itself is accompanied by palpable formations in the submandibular region. They will have an elastic consistency, and painful sensations occur upon palpation. There may be discomfort while eating, but the general condition usually does not change. Such symptoms are characteristic of the catarrhal (serous) process. If inflammation progresses, the lymph node can be completely destroyed by a purulent process. In this case, the skin over the node becomes hot to the touch, turns red, and body temperature rises depending on the type of inflammation (an abscess or phlegmon develops). strong painful sensations of a tugging or pulsating nature occur already at rest.
Lymphadenitis can be diagnosed by inspection and palpation of the affected area. Depending on what the doctor suspects as the cause of the inflammation, appropriate diagnostic methods will be prescribed. Be sure to conduct an examination of the oral cavity: inflammatory changes in the teeth, oral mucosa, tonsils, pharynx, larynx and other organs can be noted. The dentist may prescribe a panoramic X-ray or an X-ray examination of the sinuses. All patients are shown a general blood test. In the absence of pathology on the part of the dentofacial apparatus, a consultation with a therapist or otolaryngologist is indicated. In some situations, consultation with an oncologist is required.
Additional methods include smears from the oropharynx to determine the causative agents of the infectious process, biochemical blood tests, ultrasound of regional areas (will reveal an increase in nodes inaccessible to palpation), various methods of visualization of the head and neck organs (for the presence of oncological pathology), puncture biopsy of the affected lymph node with cytological and histological examination and other methods.
Treatment depends on the type of inflammation. In the case of a purulent process, surgical treatment is indicated - opening and draining the lesion. If the inflammation is catarrhal, then a dentist or otolaryngologist treats the underlying disease (pharyngitis, tonsillitis, laryngitis, periodontitis, periostitis, pulpitis and others). In such a situation, the lymph nodes are not opened under any circumstances, but conservative therapy is carried out: UHF therapy, ointment dressings, heating using a dry heat source.
Possible complications
This diagnosis is a good reason to consult a doctor and carry out urgent treatment. In the worst case, dangerous consequences may occur through:
- purulent pimples,
- thrombophlebitis,
- septicopyemia.
When purulent fluid is released into the esophagus or bronchi, then there is a high risk of the spread of dangerous complications (for example, fistulas in the esophagus).
As a result of the chronic form of the disease, inflammatory processes in the form of sepsis or adenophlegmon are often observed.
Therapy
Lymphadenitis is treated in an adult using traditional methods. These include:
- bed rest,
- treatment with antibiotics,
- UHF,
- electrophoresis,
- galvanization,
- no impact on damaged areas of the body,
- vitamin complexes.
Among other things, they may also prescribe special products and ointments.
Importance is attached to lymphadenitis treatment with antibiotics . Before prescribing this type of treatment, the specialist is obliged to conduct an examination to determine whether harmful organisms have reacted to such drugs. It is clear that the doctor prescribes to the patient those medications to which the pathogens give a reaction.
When it comes to urticaria lymphadenitis with purulent processes, then to cure it is necessary to open the purulent pimples and remove all the liquid from them.
If a tuberculosis bacillus is detected, the patient is transferred to hospital treatment. Within the clinical center, strict monitoring of the patient’s condition is carried out, as well as his isolation from healthy people to prevent the development of infection.
treatment of lymphadenitis
To treat chronic lymphadenitis, it is necessary to detect and eliminate the main factor of lymph node compaction. Only this will allow you to get rid of the pathology 100% forever.
Treatment of inflammation of the lymph nodes
The symptoms of pathology can be eliminated with the help of medications, traditional methods of treatment and physiotherapy.
Medicines
| Group name | Effect on lymphadenitis | Representatives |
| Antibacterial drugs | Antibiotics destroy the cell membrane of bacteria, which leads to their death. Used for bacterial infections. | Amoxiclav, Clindamycin, Azithromycin |
| Antiviral drugs | They inhibit the development of the virus by suppressing DNA replication or inhibiting neuraminidase. Used for viral lymphadenitis. | Amantandine, Remantandin, Tamiflu |
| Antifungal drugs | Drugs that increase the permeability of the fungal membrane, which prevents their reproduction and destroys the fungus from the inside. | Fluconazole, Amphotericin B |
| Antiseptics | Prevent the development of infection that occurs when the skin is injured. | Vishnevsky ointment, |
| Nonsteroidal anti-inflammatory drugs | Medicines that suppress the formation of prostaglandins and have a strong anti-inflammatory effect. | Ibuprofen, Ketorol, Nimesil |
| Antispasmodics | They are used for mesenteric lymphadenitis of viral, bacterial or tuberculous origin. Relieves pain. | No-Shpa, Drotaverine |
| Antihistamines | They constrict blood vessels at the site of inflammation, reduce capillary permeability, weaken and nullify the inflammatory process. | Cetirizine |
How to treat with folk remedies at home
If an accurate diagnosis has not been established and there are no medications at hand, you can use traditional methods of treatment. They include compresses and drinks made from vegetables, herbs and herbs, as well as echinacea tincture.
Uses of Echinacea
To get rid of lymphadenitis, a compress is made from echinacea - an effective remedy that resolves inflammation:
- 50 ml of tincture is mixed with 100 ml of water. The mixture is infused for half an hour.
- Gauze or a napkin is moistened with the solution and applied to the inflamed area.
- A small layer of cotton wool or soft cloth is laid on top.
- The compress is secured to the area with a bandage and held until it dries.
Beet juice
Beetroot juice, obtained from the vegetable or its tops, has a strong cleansing effect and also improves the functioning of the lymphatic system.
To cure lymphadenitis, it should be consumed as follows:
- Extract juice from beets using a juicer. It is advisable to pre-cut it into pieces.
- Let the juice steep for half a day.
- Drink 100 ml of the drink on an empty stomach, morning and evening.
If the product is given to a child, the volume of juice should be reduced by half. It is also advisable to add a little carrot juice to make the drink more palatable.
Anti-inflammatory collection
Herbal infusions that relieve inflammation - you can use either ready-made pharmaceutical ones or mix the following ingredients yourself:
- peppermint;
- raspberry leaves and berries;
- dandelion root;
- Linden blossom;
- wormwood grass.
The components must be dried and mixed in equal proportions. 4 tbsp. l. the resulting collection is poured with 1 liter of boiling water, the infusion is allowed to brew for half a day, and then drunk half a glass 3-4 times a day.
Celandine compress
Celandine is an effective disinfectant and anti-inflammatory agent. To combat lymphadenitis, it can be applied to fresh leaves; they must be scalded with boiling water, cool slightly and applied to the affected area for 30-40 minutes.
A celandine compress is made as follows:
- 25 ml of celandine is diluted in 100 ml of water. The mixture is infused for half an hour.
- Gauze is soaked in the solution and applied to the lymph node.
- The compress is covered with cotton wool or a soft cloth, secured with a bandage and left for an hour.
Horsetail infusion
{banner_banstat9}
Horsetail is a blood purifier that improves the functioning of the lymphatic system.
An infusion of it is taken orally and prepared as follows:
- A tablespoon or 1 pharmaceutical bag of herbs is brewed in 250-300 ml of boiling water.
- The mixture is infused for 20-30 minutes, then filtered.
- Take 3 times a day, half an hour before meals.
To enhance the effect, it is worth making a decoction of knotweed herb according to the same recipe. Taking infusions should be alternated at intervals of 2 days.
Physiotherapy
Physiotherapy is the use of physical factors on the body to treat a disease. The use of the method for lymphadenitis reduces inflammation, accelerates tissue regeneration, and also alleviates the patient’s general condition.
Physiotherapeutic methods used for inflammation of the lymph nodes:
- Ultra-high frequency or UHF therapy. It affects the body with a high-frequency electromagnetic field, increasing temperature and dilating blood vessels. This helps leukocytes quickly reach the site of inflammation, which speeds up recovery.
- Laser therapy. It affects the body's tissues with light waves, improving microcirculation, analgesically and relieving inflammation in the lymph node. Accelerates regeneration, helps with all types of lymphadenitis.
- Galvanization. It affects the body with a weak low-voltage electrical tone, relieving pain, restoring tissue and nerve fibers, stimulating microcirculation inside the lymph node.
When using these methods, lymphadenitis goes away faster, but they cannot completely replace drug therapy. Physiotherapy should be used as an adjuvant and only under the supervision of a physician to avoid complications.