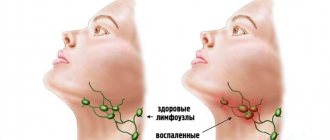
What is submandibular lymphadenitis
Submandibular lymphadenitis is an inflammatory disease of the submandibular lymph nodes, which can take an acute and chronic course. Lymphadenitis of the submandibular lymph nodes is very often odontogenic (when the infection spreads from periodontal tissues (apical or marginal periodontitis), with pericoronaritis of the lower wisdom teeth, with suppuration of a radicular cyst, alveolitis). Also, the cause of an inflammatory process in the lymph node can be an infection in the tonsils, ear, throat and oral mucosa. Acute lymphadenitis can occur in serous and purulent forms.
Acute process
The serous form of this disease is characterized by a slight impairment of the general condition. The submandibular lymph nodes are painful on palpation, enlarged, elastic in consistency, oval in shape, not fused with the surrounding tissues. The skin over them is not changed. Usually, when the process that led to lymphadenitis is eliminated, the inflammatory phenomena subside.
However, in some cases, the serous process can turn purulent, in which case acute purulent lymphadenitis develops.
It begins with severe spontaneous pain in the lymph node, and the patient also notes fever, chills, headache and insomnia. Redness of the skin over the node and adhesion to the surrounding tissues are determined. Palpation reveals a round, painful infiltrate.
Treatment of acute lymphadenitis can be conservative (for the serous form, when physiotherapeutic methods are prescribed) and surgical (for the purulent form), the essence of which is the primary surgical treatment of the lesion, installing a drainage for the purpose of drainage of purulent exudate. But these measures will not bring effective long-term results if the cause that caused the disease is not eliminated. Therefore, it is extremely necessary to remove the causative tooth (or open its cavity), treat the tooth socket (for alveolitis), and also treat infections of the tonsils and ear. For purulent lymphadenitis, the following is indicated: antibiotic therapy, the use of desensitizing agents, rinsing the mouth with antiseptics.
Cervical lymphadenitis - symptoms and treatment
Elimination of the primary source of infection
Cervical lymphadenitis is often caused by acute or aggravated periodontitis and complications of advanced caries, such as acute purulent periostitis.
If the tooth can be saved, the root canals are cleaned and filled. If it is impossible to restore a tooth, it is removed. When a purulent focus has formed, the diseased tooth is treated or removed, and the abscess is opened. If cervical lymphadenitis has developed due to a disease of the ENT organs, the source of acute inflammation should also be eliminated.
Drug therapy
- Antibacterial therapy. Broad-spectrum antibiotics are usually used, mainly with a bactericidal effect. The components of such drugs destroy the cell wall of the bacterium or disrupt its metabolic processes, which leads to the death of the microbe. If the patient's condition does not improve, biological material obtained from the lymph node is examined and the sensitivity of microorganisms to drugs is determined.
- Antiviral drugs are used for viral origin of lymphadenitis, for example, herpes.
- Anti-inflammatory drugs suppress inflammation at the cellular level, reduce pain and reduce fever.
- Antihistamines reduce capillary permeability, which prevents the development of edema and congestive processes. They also prevent leukocytes from penetrating into the lesion and inhibit the production of substances that contribute to the development of inflammation.
Physiotherapeutic treatment
- UHF (ultra-high frequency therapy) is aimed at reducing swelling, inflammation and pain.
- Ultrasound is used to speed up the resolution of the inflammatory process.
- UVR (ultraviolet irradiation) is indicated to reduce inflammation.
- Laser therapy is aimed at reducing pain, improving nutrition and blood supply to the affected area.
- Electrophoresis is a method in which a medicinal substance penetrates tissue using a direct electric current. For lymphadenitis, electrophoresis with potassium iodide and proteolytic enzymes is usually performed.
- Magnetic therapy is aimed at reducing pain, inflammation, swelling and congestion in tissues.
Physiotherapeutic methods are used in Russia to reduce the duration of drug treatment, but there is insufficient scientific evidence of their effectiveness.
Surgical intervention
Opening a purulent focus is indicated for purulent forms of lymphadenitis and adenophlegmon. Depending on the size of the lesion, the operation is performed under local or general anesthesia. During surgery, the purulent contents and tissue of the disintegrated lymph node are removed.
After surgical treatment, a drainage is placed in the wound, which ensures the drainage of pus and prevents the edges of the wound from healing. Then the wound is treated, its edges are renewed and sutured.
Detoxification therapy
Reduces the level of toxins in the body by diluting them, absorbing breakdown products and increasing diuresis. To do this, drink more fluid, and in severe cases, Hemodez and Reogluman are administered intravenously.
Diet
It is recommended to eat a balanced diet and consume enough vitamins, macro- and microelements.
Features of treatment of lymphadenitis
Treatment of cervical lymphadenitis directly depends on the stage and form of the disease.
In acute serous lymphadenitis, special attention is paid to the primary source of inflammation: inflammatory diseases of the teeth, oral cavity and ENT organs. If the primary inflammatory process is stopped in the early stages, then the symptoms of acute serous lymphadenitis also become less pronounced.
In almost 98% of cases with acute lymphadenitis, it is possible to identify the primary lesion [10]. It is eliminated and antibacterial, antiviral, anti-inflammatory or antihistamine therapy is prescribed.
When a purulent form develops, the primary focus is eliminated, the abscess is opened and the tissue of the disintegrated lymph node is removed. The patient is usually kept in the hospital under 24-hour observation. Daily dressings are performed, antibacterial, anti-inflammatory, antihistamine and detoxification therapy is prescribed.
In case of chronic hyperplastic lymphadenitis, the affected lymph node is removed, and treatment is also carried out in the hospital. Tissue fragments are sent to the laboratory, processed and examined under a microscope. This procedure allows you to exclude cancer and prevent its development.
Basic treatment methods and contraindications
Treatment is carried out using an integrated approach and conservative methods of therapy.
The following medications are prescribed:
- antibiotics of narrow or broad spectrum of action;
- probiotics - to preserve intestinal microflora;
- antihistamines - to prevent allergic reactions and reduce tissue swelling.
Physiotherapeutic methods are represented by UHF and EHF therapy, which has an anti-inflammatory and antiseptic effect.
Severe infections may require surgery.
Contraindications:
- suspicion of the presence of a tumor formation;
- Do not apply warm compresses or heat areas of swelling.
WHAT DOES LYMPHADENITIS THREATEN?
22.Mar.2021
The infection can enter the lymph node from a wound, boil (boil), panaritium, diseased tooth and other sources. The inflammatory process is accompanied by pain and enlargement of the lymph node, headache, weakness, general malaise, and increased body temperature.
In the case when suppuration of the lymph nodes themselves occurs, the symptoms become more pronounced: intense pain appears, the skin over the lymph nodes becomes red, the previously clearly defined nodes merge with each other and the surrounding tissues, and become immobile.
Of practical importance are primarily superficial and deep lymphadenitis of the face and neck. In the facial area, there are buccal, parotid and mandibular lymph nodes.
In the tissue on the outer surface of the body of the lower jaw and in front of the place of attachment of the masticatory muscle, the so-called supramillary or mandibular lymph nodes are located. The deep nodes are located between the lobules of the parotid gland, corresponding to the level of the earlobe.
Acute inflammation begins with a feeling of some awkwardness when moving the head, dull pain in the area of the affected node or group of nodes. Enlarged lymph nodes are clearly visible on palpation, but they are somewhat painful and have a dense elastic consistency. General disturbances at the beginning of inflammation may be absent or mild.
If the course is unfavorable, the inflammation can turn purulent: the node becomes inactive, “fused” with others, forming a group. Body temperature rises to 37.2-37.8 °C. Changes characteristic of ulcers appear in the blood. The patient becomes unwell, weak, loses appetite, etc. In turn, the inflamed lymph node gradually melts and leads to the formation of a fistula tract (with the disease becoming chronic).
Chronic specific lymphadenitis, as a rule, affects the mandibular, submandibular, premaxillary and cervical nodes. Sometimes it is combined with damage to the lymph nodes in other parts of the body, including bronchial and retroperitoneal. The course of chronic lymphadenitis is very diverse, which depends on the stage of the disease, the number of affected lymph nodes, the reaction of the tissues surrounding the node, etc. The diagnosis of inflammation of the lymph nodes is established only during a medical examination. Self-treatment is also contraindicated.
Elena Averkina
, oncologist, Nyagan City Clinic
M.S. Savenkova, A.A. Afanasyeva, A.K. Abdulaev, L.Yu. Nizhko Department of Clinical Functional Diagnostics with a course in Pediatrics, State Educational Institution of Higher Professional Education, Russian State Medical University of Roszdrav, Morozov Children's City Clinical Hospital, Moscow
In recent decades, one cannot fail to note the significant progress that has occurred in the field of diagnosing various infectious diseases in children, thanks to which the clinical features of the course of infections such as chlamydia, mycoplasmosis, toxoplasmosis, bartonellosis, borreliosis, as well as herpesvirus infections (EBV, CMV) have become more clear. and others. One of the important symptoms of the above diseases is lymphadenopathy - enlarged lymph nodes of varying severity. Unfortunately, the symptom of enlarged lymph nodes is not always assessed in a timely manner by pediatricians and is not given due attention. The structure of lymph nodes Lymph nodes are peripheral lymphoid organs, consisting of cells of various types, connected to the circulatory system by afferent and efferent lymphatic vessels and postcapillary venules. Fibroblasts and their derivatives, reticular cells, form a supporting structure. Tissue macrophages, dendrites and Langerhans cells are important antigen-bearing cells. Lymphoid follicles consist mainly of B lymphocytes. Primary lymphatic follicles are populated by IgM and IgD-bearing B cells and helper T lymphocytes (inducers) even before the antigenic stimulus. Secondary lymphatic follicles are formed as a result of antigenic stimulation and contain an internal zone (germinal center) consisting of activated B cells, macrophages, follicular dendrites and helper cells. The areas between follicles and paracortical areas consist mainly of T lymphocytes. The co-location of a large number of macrophages, dendrites, Langerhans cells and lymphocytes allows the lymph node to perform the main function of a specialized structure that integrates all these cell types to create an effective cellular and humoral immune response of the body. Enlargement of the lymph node may be due to: 1) an increase in the number of benign lymphocytes and macrophages during the immune response to the antigen; 2) infiltration by inflammatory cells during infections affecting the lymph node (lymphadenitis); 3) proliferation in situ of malignant lymphocytes and macrophages; 4) infiltration of nodes with metastatic malignant cells; 5) infiltration by macrophages loaded with metabolic products in various storage diseases.
Pathogenesis of lymphadenopathy Back in 1980, the term lymphadenitis was commonly used to mean “inflammation of the lymph nodes that occurs as a complication of various purulent-inflammatory diseases and specific infections (tuberculosis, plague, actinomycosis). In previous years, pyogenic cocci were considered the main etiological causative agents of the development of lymphadenitis. Later, different types of microorganisms (bacteria, viruses, fungi) were described as pathogens. There is acute inflammation of the lymph nodes, which is characterized by a short prodromal period, fever, local pain on palpation, and chronic, which is usually characterized by a longer duration, absence of pain or its low severity. In chronic inflammation, unlike acute inflammation, the lymph nodes are usually separated from the surrounding tissues. Lymphadenitis can be local, regional, generalized. Regional lymphadenitis has been described in streptococcal and staphylococcal infections, tularemia, tuberculosis, syphilis, and genital herpes. Generalized enlargement of lymph nodes is described in infectious mononucleosis, cytomegalovirus infection, toxoplasmosis, brucellosis, tuberculosis, AIDS, storage diseases, etc. Enlargement of lymph nodes occurs as a result of the accumulation of microbes or viruses and their toxins in them by lymphogenous, hematogenous and contact routes. In acute lymphadenitis, serous edema is observed, and inflammatory phenomena do not extend beyond the capsule of the lymph node. During destructive processes, inflammation can spread to surrounding tissues and, by the nature of the inflammation, be serous and/or purulent.
Clinical picture and diagnosis The clinical symptoms of lymphadenitis are the same and are characterized by pain on palpation, an increase in size, and an increase in body temperature. Hyperemia of the skin over the lymph node appears later, as the process progresses and the serous transition to the destructive stage. For the convenience of assessing the inflammatory reaction of the lymph nodes, we have identified three degrees of their enlargement: (Sav 2003):
I degree – from 0.5 to 1.5 cm in diameter; II degree – from 1.5 to 2.5 cm in diameter; III degree – from 2.5 to 3.5 cm in diameter and more.
Lymphadenopathy is characterized, as a rule, by an enlargement of a number of groups of lymph nodes without signs of hyperemia of the skin over them. However, palpation often reveals not one enlarged lymph node, but several, or a conglomerate consisting of lymph nodes of different consistency and size. In this regard, the group of lymph nodes (cervical, axillary, inguinal, etc.) should be indicated. To clarify the nature of the damage to the lymph nodes, determine their quantitative and qualitative characteristics, it is advisable to conduct an ultrasound examination. Ultrasound examination of lymph nodes makes it possible to clarify their size and determine the duration of the pathological process and its severity. In acute inflammation, the hypoechogenicity and homogeneity of the lymph nodes is determined. Adhesive lymph nodes suggest a disease duration of more than 2 months. With the chronic course of the process, their echogenicity increases. In practice, pediatricians have repeatedly encountered underestimation of the symptom of enlarged lymph nodes. Unfortunately, children do not always arrive (apply) for examination in a timely manner; as a result, a chronic course of the infectious process is formed, and often transformation into hematoblastosis. Considering the increase in the number of lymphadenopathy in recent years, we examined children admitted to the hospital or outpatients with the main complaint of enlarged lymph nodes for the period from 2004 to 2008. to determine the predominant pathology and select adequate antibacterial therapy. The examination plan for children with lymphadenopathy (Fig. 1) must be comprehensive. You should start by assessing changes in the peripheral blood test: leukocytosis and a shift of the formula to the left indicate the course of a bacterial process (staphylococcal, streptococcal, Pseudomonas aeruginosa, hemophilic etiology). The predominance of lymphomonocytes in the blood count is usually characteristic of diseases of herpetic and intracellular etiology. To clarify the etiology of the disease, a complex of serological and microbiological examinations is required, which includes the most common diseases in children. The main diseases that occur with enlarged lymph nodes include: chlamydia, mycoplasmosis, toxoplasmosis, Epstein-Barr virus (EBV) infection, cytomegaly, as well as herpes types I, II, VI. If negative results are obtained, the examination is further carried out to exclude less common diseases: listeriosis, bartonellosis, borreliosis, parasitic diseases (toxocariasis, echinococcosis, opisthorchiasis, giardiasis, etc.). Microbiological examination should be carried out in children with a history of frequent respiratory diseases, sore throats, inflammatory diseases of the oropharynx, croup, and bronchitis. As a rule, with a localized process in the oropharynx, the regional group of cervical lymph nodes increases in the clinic. Polyadenopathy is characteristic of a generalized infection. One of the objective auxiliary methods for additional assessment of enlarged lymph nodes is ultrasound. If a generalized reaction develops, it is recommended to test the blood for sterility and conduct an ultrasound examination of the intra-abdominal lymph nodes. In children with respiratory pathology, an X-ray examination of the chest organs is performed. If hemoblastosis is suspected, a consultation with a hematologist is necessary, who will indicate the indications and the need for a puncture biopsy.
Research Based on the main purpose of the work, 164 children (101 boys and 63 girls) aged from 6 months to 16 years were examined. The age of the children is shown in Fig. 2. The largest number of children (76.8%) with lymphadenopathy were admitted to the hospital or were treated as outpatients at the age of 1-9 years. The maximum occurred at the age of 3-9 years. The etiology of the disease was confirmed by a comprehensive examination of patients, which included: microbiological examination of microflora from the oropharynx (before treatment); serological blood test using ELISA and PCR (at the G.N. Gabrichevsky Moscow Research Institute of Epidemiology and Microbiology, NPF "Litekh" for the following diseases: chlamydia, mycoplasmosis, toxoplasmosis, herpes group viruses (I, II, IV, V, VI types) A serological examination was carried out in 164 children, a microbiological examination (throat cultures) in 93 (Fig. 3, 4). Today, knowledge of the prevailing pathogens is fundamentally important. Based on the results of the examination, 2 groups of etiologically significant pathogens were identified - herpes viruses and intracellular. In the herpetic group, Epstein-Barr viruses (61.8%) and cytomegaloviruses (54.9%) predominated; in the intracellular group - chlamydia (49.5%). In the majority of children, lymphadenopathy was of a mixed nature - 126 (76.8 %), while monoinfection was detected in 38 (23.2%). It should be noted that with mixed variants, a combination of 2-4 pathogens was noted: • mixed herpesvirus (EBV, CMV, herpes types I, II) – 30 (18.2%); • mixed intracellular (chlamydia, mycoplasmosis) – 11 (6.7%); • 2 pathogens each: herpes viruses + intracellular – 19 (11.5%); • 3 pathogens each: herpeviruses + intracellular – 34 (20.7%); • 4 pathogens each: herpes viruses + intracellular – 27 (16.5%). “Pure” bacterial lymphadenopathy was detected in only 5 (3%) people.
However, as a result of a comprehensive examination, a combination of positive serological and microbiological markers was revealed - as a result of a mixed course of the disease in 3/4 of the children. It turned out that some pathogens in the same child can simultaneously be in different forms. Table 1 presents the main (predominant) pathogens depending on the severity of the disease. In the acute form of the infectious disease, chlamydia, mycoplasma and EBV predominated in 5.8-11.6% of children. During exacerbation of the chronic course (11.6-21.5%), the same pathogens predominated. A persistent course was identified in most children, especially with CMV, EBV, and chlamydia. Among the predominant pathogens in acute and chronic forms, intracellular pathogens - chlamydia and mycoplasma - stand out. In persistent cases, CMV and EBV predominated. Thus, both in frequency and severity of the disease, chlamydia and Epstein-Barr viruses predominate. When determining cultures from the throat, the main pathogens in the majority were gram-positive cocci: streptococci, Staphylococcus aureus and Neisseria. Considering the presence of a number of pathogens, pharynx dysbiosis can be diagnosed in 82.8% of children. By the number of pathogens: 1 pathogen – in 17.2%, 2 pathogens – in 35.5%, 3 pathogens – in 21.5% (see Fig. 4). It becomes obvious that due to the mixed course of a number of diseases, the children’s history revealed frequent diseases of the ENT organs and lungs: respiratory diseases and bronchitis - in 51 (31.0%), tonsillitis, adenoiditis, otitis - in 21 (12.8%) , past pneumonia – in 5 cases (3%). 11 (6.7%) children were previously hospitalized. Most children from the group with lymphadenopathy are often ill children. The reason for this is the unfavorable course of pregnancy in 16 (9.7%) mothers, due to the presence of various infectious diseases (CMV, chlamydia, ureaplasmosis, herpes, toxoplasmosis, rubella), diagnosed during pregnancy in 17 (10.4%), pyelonephritis - in 10 (6%), ankylosing spondylitis – in 1 (0.6%) and lymphogranulomatosis – in one mother (0.6%). In general, we can distinguish four main groups of children in whom the disease manifested with the following clinical symptoms:
• with respiratory disease, cough – 65 (39.6%); • with enlarged lymph nodes – 60 (36.7%); • with prolonged low-grade fever – 21 (12.8%); • with sore throat 18 (10.9%).
Enlarged lymph nodes were detected both during examination by a doctor and by the children’s parents themselves. Attention should be paid to the fact that 17 (10.6%) children with symptoms of enlarged lymph nodes were not examined for a long time (from 6 months to 2 years). The explanation for this circumstance was a misunderstanding on the part of both doctors and parents that enlarged lymph nodes are not always a “normal phenomenon”, and even more so when its duration is obvious. The majority of children had grade I (50%) and II (48.2%) enlarged lymph nodes, and only 1.8% had grade III enlargement. As a result of the examination, the following clinical diagnoses were established (Table 2). In the table presented, the main diseases include lymphadenopathy and lymphadenitis (37.8%), bronchopulmonary diseases (40.9%), lesions of the oropharynx (18.2%), hematological diseases (3.0%). In recent years, knowledge about the etiology of lymphadenopathy and lymphadenitis has expanded significantly. In previous years, the history of studying the problem of enlarged lymph nodes was closely connected, first of all, with the most studied disease - Epstein-Barr viral infection, which has an acute and chronic course, can occur in the form of infectious mononucleosis or mononucleosis-like syndrome, and is accompanied by a significant increase in parenchymal organs. However, in our study, infectious mononucleosis in only one of 22 children was caused by the Epstein-Barr virus. For all the rest, the etiology was mixed herpetic (herpes types 1, 2 + CMV, EBV + herpes types 1, 2, etc., in combination with chlamydia - in 3 children). As our studies have shown, along with herpes viral infectious agents, one of the main pathogens for lymphadenitis today are chlamydia and mycoplasma.
Specificity of lymphadenopathy of chlamydial etiology The study of lymphadenitis and lymphadenopathy of chlamydial etiology revealed the following features: the disease began with respiratory symptoms. Catarrhal symptoms preceded enlarged lymph nodes 1-2 weeks before presentation. Hyperthermia was observed only in the case of the development of lymphadenitis, i.e., a suppurative process. With chlamydial infection, along with catarrhal symptoms, children (1/3) were identified with mononucleosis-like syndrome. At the same time, the onset of the disease was acute, with a rise in temperature to 38 ° C with moderately severe catarrhal symptoms, difficulty in nasal breathing due to adenoiditis. During this period, children complained of weakness and pain when swallowing. The development of sore throat with plaque on the tonsils after 7-12 days was caused by mixed microflora (strepto- and staphylococci). In 1/3 of the patients with chlamydial infection, the blood count showed monocytosis of more than 15% with an average number of monocytes of 9.2 ± 0.038%. Thus, mononucleosis-like syndrome due to chlamydial infection is practically indistinguishable from that of other etiologies; its etiology can only be determined on the basis of a comprehensive examination. On palpation, the majority of children detected enlarged lymph nodes of grade I - in 82 (50%), grade II - in 79 (48.2%) and grade III in only 3 (1.8%). With grade III lymph node enlargement (polyadenopathy), the lymph nodes were palpated in the form of lymph nodes fused to each other. Conglomerates of lymph nodes of the cervical group were palpated more often during infection associated with disease of the oropharynx. At the beginning of the disease, the consistency of the lymph nodes was elastic. With late admission to the hospital (3-4 weeks of illness), the consistency of the lymph nodes changed - from elastic (at the beginning of the disease) they became denser and more painful. The most accurate examination of lymph nodes (size, consistency, echo density) can only be determined by ultrasound examination. Ultrasound examination of lymph nodes was carried out using an Aloca 2000 device (Japan) with a 7.5 MHz linear sensor and was performed in 54 children. At the same time, conglomerates of cervical lymph nodes of different sizes were determined in 27 (50%), chains of enlarged lymph nodes in the abdominal cavity - in 16 (29.6%), less often - small multiple ones - in 11 (20.3%). The presence of lymph nodes in the abdominal cavity indicates a generalized infection. When analyzing the patient data, a mixed infection was identified in all children. On average, the duration of the disease ranged from 18.5 to 27.5 days (for polyadenopathy). Treatment of children with lymphadenopathy requires a thoughtful attitude and a mandatory comprehensive examination. As shown above, the main pathogens are intracellular pathogens (chlamydia) and herpes viruses (EBV), and various combinations of them. Taking into account the analysis performed, as well as the results of serological and microbiological examinations, the treatment of lymphadenopathy was as follows.
Principle of treatment of lymphadenopathy The main drugs for the treatment of lymphadenopathy in children should be etiotropic drugs that are effective and safe: macrolide antibiotics, aminopenicillins, cephalosporins, antiviral and immunomodulatory ones. The principle of treatment is as follows. If there are pronounced changes in the oropharynx or mild, as well as severe forms, treatment with protected aminopenicillins or cephalosporins should be started without waiting for the test response. After receiving serological and microbiological results (after 5-7 days) and determining the etiology of the disease, treatment with etiotropic drugs (macrolides and antiviral drugs) continues. In mild and moderate forms of the disease, macrolides may be the drugs of choice from the first days of the disease.
Experience in the use of josamycin for the treatment of lymphadenopathy Over the past years, some experience has been accumulated in the use of josamycin in its various forms: suspension in children, tablets in adults. The complexity of treatment also lies in the fact that 25.6% of children before admission to the hospital received: penicillins, cephalosporins, macrolides and antibiotics of other groups. This circumstance should also be taken into account because it is known that dysbiosis develops during antibiotic therapy. In this regard, there is an active search for drugs that minimally affect the normal intestinal microflora. The main groups of antibacterial drugs in the treatment of lymphadenitis were macrolides. In total, 79 children received drugs from the macrolide group: josamycin - 26, midecamycin - 25, roxithromycin - 23, other groups - 4 people. 25 children received cephalosporins, 21 children received aminopenicillins, 39 children received antiviral drugs (33 acyclovir and 6 arbidol). We conducted a comparative study of the effectiveness of the therapy in groups of children receiving macrolides: josamycin (group I), midecamycin (group II), roxithromycin (group III). The duration of the course of antibacterial therapy was 10 days. The effect of the treatment was assessed using a combination of serological and clinical indicators. When assessing clinical data, we took into account the dynamics of lymph node shrinkage, the degree of intoxication, improvement of condition, normalization of blood counts, and the development of dysbacteriosis. The dynamics of serological parameters were assessed before treatment and after 1.5 months by the presence or absence of serological markers. After antibacterial treatment, a positive result was achieved in all groups (Table 3). In the group of children receiving josamycin, only one child on the 3rd day of treatment developed complaints of abdominal pain, which went away on their own and did not require additional prescriptions. The effect of treatment in the other two groups was slightly lower. In each of the other two groups, 2 children had longer persistence of enlarged lymph nodes and persistence of positive serological markers, which required a repeat course of treatment. In case of mixed lymphadenopathy and the presence of herpes viruses, a long course of therapy is recommended with the simultaneous administration of the following drugs: acyclovir, arbidol. Comprehensive therapy should also include immunomodulator drugs: lykopid, viferon, cycloferon. Thus, the diagnosis of lymphadenopathy in children requires the mandatory exclusion of a group of intracellular and herpetic diseases, which are the main ones today. Given the mixed nature of lymphadenopathy in most children, complex treatment is necessary. This group of children requires dynamic observation and control, since 3% of children may have a manifestation of hemoblastosis. The success of treating children with lymphadenopathy will depend on the timely administration of etiotropic therapy in combination with antiviral drugs and immunomodulators.