Sialadenosis is a non-inflammatory disease of the salivary glands, leading to enlargement and/or disruption of their function. The lesion is dystrophic in nature and is not associated with the appearance of tumors. Structural changes in gland tissue usually appear against the background of other systemic pathologies. Dentists quite often encounter this phenomenon: 1 case out of 10 pathologies of the salivary glands is represented by sialadenosis.
The disease usually occurs in middle-aged people. Since it often accompanies endocrine, allergic, dysmetabolic and other systemic diseases, the approach to treatment should be carried out not only from the dental side.
Types of sialadenoses
Based on the location of pathological changes, the following types of sialadenoses are distinguished:
- interstitial;
- parenchymal;
- ductal
Pathological areas can be located both in the tissues of the gland itself and in the ducts.
There are several stages based on severity:
- First. The salivary glands are of normal size and are faintly palpable.
- Second. There is a slight enlargement of the glands, which is not noticeable during visual inspection, but is palpable.
- Third. Enlargement of the glands, which is noticeable both during visual inspection and palpation.
According to the nature of origin, neurogenic, allergic, endocrine sialadenoses are distinguished, as well as nutritional ones - associated with dietary habits.
Ask a Question
Material and methods
In the specialized department of the Department of Maxillofacial Surgery (MCS) at the Dentistry Center (DC) of the Moscow State Medical and Dental University (MGMSU) named after. A.I. Evdokimov examined and treated 25 people aged 25 to 50 years with chronic parenchymal sialadenitis. The criterion for inclusion in the study was the presence of chronic parenchymal sialadenitis. The criterion for non-inclusion was the presence of concomitant pathology in the acute or exacerbation stage. The exclusion criterion was the refusal of patients to further participate in the studies. To make a diagnosis, all patients underwent a clinical examination, which included examination and palpation of the altered salivary gland, determination of its size and amount of secretion, and collection of anamnesis about concomitant diseases.
All patients also underwent high-resolution ultrasound (US) in B-mode and color Doppler mapping mode on a Philips iU-22 ultrasound scanner using linear scanning sensors with a frequency of 5-17 MHz. Additionally, mixed saliva was collected from patients for 5 minutes into a sterile plastic tube with a tightly screwed cap. The samples were centrifuged and the content of albumin protein (in mg/ml) was determined in the supernatant of saliva using the spectrophotometric method and the amount of immunoglobulin (Ig) G using the enzyme-linked immunosorbent method. The initial data of ultrasound Dopplerography and mixed saliva were compared with the results of the study on the 7th day and 1 month from the beginning treating patients.
According to the method of the proposed treatment, the patients were divided into two groups. Patients of group 1 ( n
=11) carried out standard antibacterial and antispasmodic therapy
per os
for 5 days with the following drugs: enhanced amoxicillin 625 mg, 1 tablet 3 times a day, drotaverine 1 tablet 2 times a day.
Patients of the 2nd group ( n
= 14), along with standard therapy, were prescribed
per os
complex antihomotoxic therapy with Traumeel S, 1 granule 3 times a day and lymphomyosot, 15 drops 3 times a day for 24 days, spascuprel, 1 tablet 2 times a day for a course of 5 days. All manipulations were carried out only after the informed consent of the patient, signed by him and the attending physician in duplicate. The rationale for the use of these homeopathic drugs was that Traumeel S is a highly effective remedy for inflammatory processes, the drug spascuprel has an antispasmodic, analgesic, sedative and anticonvulsant effect, the drug lymphomyosot improves the microcirculation of peripheral vessels. All obtained digital values were processed by the method of variation statistics using the Statistica 8.0 program.
Why does sialadenosis occur?
Sialosis can develop against the background of underlying diseases or be caused by certain physiological reasons. For example, pathology occurs in women during pregnancy and lactation. Pathological changes are often provoked by autoimmune diseases - systemic scleroderma, rheumatism, psoriasis, etc., as well as metabolic and endocrine disorders.
Eating disorders that lead to sialosis include strict long-term diets and restrictions, and anorexia. In general, the most common causes are diabetes mellitus, menstrual dysfunction and thyroid dysfunction, chronic pancreatitis and other gastrointestinal pathologies.
The allergic nature of the disease may be associated with drug allergies. In some cases, sialosis of the salivary glands develops after surgery or trauma in the area of the dental system.
Reasons for the development of sialadenoses
Sialadenosis can be caused by both physiological reasons and the pathological condition of the patient, namely:
- pregnancy;
- breastfeeding;
- alcohol abuse;
- endocrine system disorders;
- diabetes mellitus;
- menstrual irregularities (hypermenstrual syndrome);
- prostatitis;
- chronic pancreatitis;
- autoimmune diseases (rheumatoid arthritis, systemic lupus erythematosus, scleroderma, psoriasis, Sjogren's disease, Mikulicz's disease, etc.);
- decreased nutrition due to anorexia nervosa.
Patients may also develop allergic sialadenoses when taking certain medications. Sialadenosis may occur after surgery on the salivary gland or after injury to it. The main and most common cause of sialadenosis in patients who suffer from alcoholism is liver cirrhosis. There are also frequent cases of the development of sialadenoses of unknown origin in patients who do not have any systemic diseases. In this case, the patient undergoes an examination to identify a general disease. The mechanism of development of this pathology in medical practice is not entirely clear. But in medicine there are such factors for the manifestation of this disease as:
- neuropathy, which is accompanied by the destruction of nerve fibers;
- disturbances in the microcirculatory system and lipid oxidation, which leads to damage to cell tissue;
- congenital expansion and violation of the architectonics of the ductal system.
These processes cause functional failure and replacement of glandular tissue with adipose tissue.
Symptoms of the disease
Sialosis most often affects the parotid glands, rarely - the submandibular and sublingual glands. Usually we are talking about a bilateral pathological process. The picture of the disease is nonspecific - painful swelling appears in the area of the affected glands, their increase in the 2nd and 3rd stages. The increase persists over time.
One of the manifestations of the disease is dry mouth. This is due to the fact that salivation during illness may be insufficient.
During the examination, the doctor will determine the characteristic swelling of the soft tissues. Palpation does not cause severe pain; sometimes discomfort or mild pain appears. The nearby lymph nodes are not changed, and there are no restrictions in opening the mouth. During a massage of the salivary gland, clear saliva is released without external features.
It is worth noting that specific symptoms may accompany sialosis, occurring with decreased or increased salivation without an increase in the glands themselves. For example, this is observed with stomatitis, duodenal ulcers, parasitosis, neurasthenia, etc.
Diagnostic features
Examination of a person with suspected sialadenosis may include the following methods:
- survey, examination, palpation of the glands;
- laboratory tests - general and biochemical blood tests, clinical urine tests, assessment of carbohydrate metabolism (glucose test);
- Ultrasound of the salivary glands and soft tissues is necessary to confirm the non-inflammatory nature of the disease and exclude tumors.
It is important for the doctor to exclude other possible pathologies characterized by enlargement of the salivary glands: inflammatory diseases, infectious diseases, cysts and tumors, the formation of calculi (stones).
Sialography is prescribed to determine dilated or narrowed salivary ducts; it involves the administration of a contrast agent. A radiosialogram may also be required to assess the secretory capacity of the glands. Using a CT scan, the doctor can see a bilateral increase in tissue size and density and rule out malignant and benign formations.
As an additional method, sialometry, cytological studies of secretions (salivary fluid), as well as biochemical studies of saliva can be used. The final diagnosis can be made after aspiration or another type of gland biopsy. Histological study allows us to establish dystrophic changes.
To find out the exact cause of the disease, it is important to assess your overall health. Therefore, the patient often needs to be examined by another specialist: an endocrinologist, gynecologist, urologist, allergist, etc. In some cases, the involvement of a rheumatologist is required.
Treatment methods
Treatment of sialadenosis is a multi-step process. The main condition is effective therapy for the underlying or concomitant disease, although this will not help solve the problem completely. Symptomatic therapy is possible using novocaine blockades. Physiotherapy will help cope with unpleasant symptoms; electrophoresis, galvanization, magnetic and laser therapy are widely used. The impact is carried out on the area of the cervical nerve tissue in order to improve the conductivity of impulses.
Drug therapy consists of the use of vitamin E, drugs to stimulate salivation, as well as colloidal solutions to correct blood viscosity and improve blood flow in small blood vessels. Surgical treatment may be indicated in the absence of a positive response to conservative therapy. It consists of partial or complete removal of the salivary gland or its duct.
Results and discussion
As can be seen from the data in table. 1, with a long course of T2DM, an increase in the level of IL-2 and a decrease in IFN-γ in the GC was noted. The level of IL-1β was highest in the group of patients with a duration of T2DM ≤5 years.
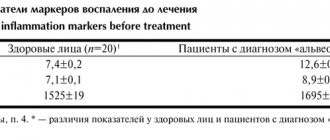
Table 1. Cytokine content in gastric mucosa in patients with sialosis and diabetes mellitus-2 of varying duration (M±m)
Table 1. Cytokine content in the oral fluid of patients with sialosis and type 2 diabetes (M±m)
| Index | Practically healthy (n=10) | All patients (n=40) | Duration of SD-2 | |
| ≤5 years (n=15) | >5 years (n=25) | |||
| IL-1β, pg/ml | 42,3±3,7 | 45,3±1,0 | 46,7±1,5 | 44,5±1,4 |
| IL-2, pg/ml | 11,4±2,1 | 15,2±0,4 | 11,5±0,7 | 13,8±0,3** |
| IFN-γ, pg/ml | 8,8±0,8 | 6,9±0,2* | 7,2±0,4 | 6,7±0,2* |
Note. The differences are statistically significant (p<0.05) *—compared to the data in practically healthy people; ** — between groups of patients.
According to the data presented, the content of IL-1β, IL-2 in patients with diabetes is higher, and INF-γ is lower than in practically healthy individuals. Our results indicate a change in the local cytokine status in patients with different durations of T2DM (>5 years) and sialosis. Statistically significant differences between groups of patients in the duration of T2DM were noted in the level of IL-2 (p<0.05)
The level of glycemia based on HbA1c content ≤8% was determined in 22 patients with sialosis and T2DM and on average in the group was 7.2±0.1%. Insufficient glycemic control (HbA1C >8%) was detected in 18 patients and their HbA1c level was 9.0±0.2%. Statistically significant changes between groups were noted in the content of cytokines IL-1β and IL-2 (p<0.05). The most pronounced increase in the level of IL-1β was detected in the group with an HbA1c level >8.0% - the average content of this cytokine was 51.6±1.1 pg/ml and was 1.2 times (p<0.05) higher, than in the group with HbA1c level ≤8.0%. An increase in IL-2 levels was observed with the same trend, i.e. There was an increase in this indicator simultaneously with an increase in the level of HbA1C in the blood. At the same time, the concentration of IL-2 in saliva in the group with an HbA1C level >8.0% was 16.7±0.7 pg/ml, which is 1.2 times higher than in the group with an HbA1C level ≤8.0% and this change was statistically significant (p<0.05; Table 2 ) The level of IFN-γ in the group with HbA1C >8.0% was 7.1±0.2 pg/m, which was 4.2% higher, than in the group with HbA1C ≤8.0%, but not statistically significant.
Table 2. Comparison of the average levels of IL-1β, IL-2 and IFN-γ with the level of glycated hemoglobin in patients with sialosis and T2DM (M±m)
Table 2. Comparison of mean IL-1β, IL-2 and FNO-γ with glycated hemoglobin level in patient with sialosis and type 2 diabetes (M±m)
| Index | Practically healthy (n=10) | HbA1c level | |
| ≤8.0% (n=22) | >8.0% (n=18) | ||
| IL-1β, pg/ml | 42,3±3,7 | 42,3±1,1 | 51,6±1,1* ** |
| IL-2, pg/ml | 11,4±2,1 | 14,1±0,3 | 16,7±0,7* ** |
| IFN-γ, pg/ml | 8,8±0,8 | 6,8±0,3 | 7,1±0,2* |
Note. The differences are statistically significant (p<0.05) * - compared with data in practically healthy people; ** — between groups of patients.
Thus, the studies have shown that insufficient glycemic control in patients with type 2 diabetes and sialosis is accompanied by an increase in the level of proinflammatory cytokines in the stomach.
Very important for patients with T2DM is the possibility of correcting immune disorders using systemic enzyme therapy drugs that have anti-inflammatory and immunomodulatory properties.
A decrease in the level of IL-1β in the GC after treatment was observed in two groups of patients with sialosis. However, in patients of the main group after enzyme therapy, the content of IL-1β in the GC was the lowest (45.0±0.4 pg/ml) and in the control group it was 46.2±2.3 pg/ml.
After treatment, the level of IL-2 in the GC of patients in the control group decreased slightly from 13.6±0.3 to 13.3±0.3 pg/ml, in patients of the main group - from 13.9±0.4 to 11. 9±0.2 pg/ml. In the main group, a statistically significant (p<0.05) decrease in the level of IL-2 in the GC was detected compared with the data before treatment. In patients of the main group, the level of IL-2 in the GC after treatment reached almost the same values as in practically healthy ones (11.4±2.1 pg/ml).
In patients with sialosis against the background of T2DM, before treatment there is a decrease in the level of IFN-γ in the GC and an increase to 7.3±0.2 pg/ml after treatment by 1.1 times (Table 3) .
Table 3. The content of cytokines in the gastric mucosa in patients with sialosis and diabetes mellitus-2 in the dynamics of treatment (M±m)
Table 3. Cytokines oral fluid content in patients with sialosis and type 2 diabetes before and after treatment (M±m)
| Index | Practically healthy (n=10) | Comparison group (n=20) | Main group (n=20) | ||
| before treatment | after treatment | before treatment | after treatment | ||
| IL-1β, pg/ml | 45,2±4,8 | 46,3±2,5 | 46,2±2,3 | 48,4±0,8 | 45,0±0,4** |
| IL-2 pg/ml | 11,4±2,1 | 13,6±0,3 | 13,3±0,3 | 13,9±0,4 | 11,9±0,2** |
| IFN-γ pg/ml | 8,8±0,8 | 6,9±0,3* | 7,3±0,2 | 6,7±0,2* | 8,3±0,1** |
Note. The differences are statistically significant (p<0.05) * - compared with data in practically healthy people; ** — between groups of patients after treatment.
At the same time, when enzyme therapy was included in the treatment regimen, the increase in the level of IFN-γ in the main group was more pronounced and averaged 8.3±0.1 pg/ml, which was 1.2 times higher than the initial level (p<0. 05).
An objective analysis of the clinical picture in patients of the main group revealed an improvement in general well-being, increased salivation and the disappearance of a feeling of dryness on the 7th day, and in the control group - on the 9th day. Positive dynamics of clinical signs by the end of treatment was observed in all patients of the main group (receiving enzyme therapy) and in 14 (70%) patients in the control group (on the background of traditional therapy).