Indications and contraindications Advantages Disadvantages Types of sinus lifting Preparation for surgery How the operation is performed Is it painful Restrictions after surgery Bone material and membranes Is sinus lifting dangerous Price in Moscow Where is the best place to do it?
Almost the entire body of the maxillary bone is occupied by the maxillary sinus - a large cavity, the lower wall of which is adjacent to the roots of the teeth. The inside is lined with a thin mucous membrane. When assessing the prospects for implantation, the implant surgeon measures the height of the bone from the lower border of the jaw to the bottom of the maxillary cavity in order to understand whether an implant of the correct length will fit there and whether this bone will withstand the implant under active chewing load. If the bone volume is insufficient, the doctor must carefully restore the lost bone along the border of the maxillary sinus before implantation. This microsurgical operation is called sinus lift.
Important! Due to the anatomical structure of the skull bones, the operation is performed only on the upper jaw from 4 to 7 teeth. In the lower jaw, only classical bone reconstruction is performed.
What is a sinus lift in dentistry?
Indications and contraindications
The absolute indication is a lack of bone tissue in the upper jaw, bone atrophy after traumatic tooth extraction in the past, and the impossibility of implantation with root-shaped implants according to the classical protocol.
This treatment is also indicated for patients at risk for osteoporosis of the jaw bones and patients with metabolic disorders in menopause or its excessive fragility.
Contraindications as for any surgical operations:
- Acute immune diseases;
- Oncological diseases in the stage of decompensation or earlier than 6 months after chemotherapy;
- Uncontrolled bleeding disorders;
If the patient has ARVI, sinusitis, sinusitis or other diseases of the ENT organs, then the procedure should be postponed until complete recovery. Previously performed sinus lifting, trauma to the maxillary sinus, surgery in the area of the maxillary sinuses in the past are not contraindications; after consultation, we will select the optimal treatment algorithm for you.
Literature
- Ziccardi V., Betts N. Complications with increased bone volume in the maxillary sinus. Perio IQ. – 2005. – No. 1. – P.93-102.
- Fabbro MD, Testori T, Franchetti L, Weinstein R. Systematic review of the survival of sinus implants after sinus lift. Perio IQ. – 2005. – No. 4. – P.54-66.
- Sharan A., Majar D. Pneumatization of the maxillary sinus after extraction of the upper teeth. Perio IQ. – 2010. – No. 15. – P.93-106
- Jensen T. The sinus bone graft / edited by Ole. Chicago: Quittessence, 1999: 201-208
- Boyne PJ, James RA Grafting of the maxillary sinus floor with autogenous marrow and bone. J Oral Surg 1980:38:613-617.
- Triplett RG, Show SR: Autologous bone grafts and endosseous implants: Complementary techniques. J Oral Maxillofac Surg 1996;54:486-494.
Types of sinus lift
Open
It is performed to build up a large amount of lost bone. Requires serious training of the surgeon. The waiting period between surgery and implantation is several months.
More details
Closed
If the patient’s bone is high and does not require volumetric augmentation, then a closed technique is used (soft or BIO sinus lift). Also carried out through a small hole.
More details
Modified
The balloon method allows you to combine augmentation and implantation, including on thin bone. The formation of a cavity in the maxillary sinus occurs using a special disposable balloon.
More details
Differences between open and closed techniques
Objectively, these are two similar operations, the purpose of which is to form new bone tissue in the patient’s upper jaw by filling the defect in the lower border of the maxillary sinus with a special bone material or a bone growth stimulator. They differ in the volume and time of surgical intervention.
When open, manipulations are carried out quickly through a standard 5 mm hole in the bone. For a closed, rather narrow channel, which is formed not by ultrasound, but by osteotomes, and into which the implant is then inserted.
Simultaneous implantation is another pseudo-difference between closed lifting; often with open sinus lifting, implants are also installed simultaneously; the timing of regeneration does not depend on the name of the operation and depends only on the complexity and size of the bone defect being restored. You still have to wait several months for the bone to mature.
Rehabilitation period
Compared to an open sinus lift, a closed sinus lift is a less traumatic operation associated with a lower risk of complications, as well as a shorter recovery period. But if you strictly follow all the doctor’s recommendations, then the risk of their development is minimal:
- Eating is possible only 2 hours after surgery. All dishes should be liquid, semi-liquid and at medium temperature.
- You need to brush your teeth with a soft brush, but carefully in the area of the operation.
- For 2-3 weeks, avoid long trips, flights, alcohol intake, and intense physical activity.
- It is important to take the recommended medications: antibiotics, vasoconstrictor drops, etc.
- It is forbidden to sneeze with your mouth closed.
Our doctors monitor the rehabilitation period of patients at all stages. This is why it is so important to come for preventive examinations.
Tell us about us:
Preparing for surgery
Before the operation, the surgeon carefully examines the bones of the upper jaw on a CT scan and the location of the maxillary sinus on an X-ray. Before the operation, dental plaque is cleaned and sometimes, if chronic sinusitis is suspected, antibiotics are prescribed two days in advance to avoid cross-infection during the procedure. Smokers are given replacement therapy (the operation does not require a temporary cessation of smoking, but life is more comfortable with replacement therapy).
Read more about preparation here.
Clinical case
A 38-year-old man with no significant medical history presented with missing chewing teeth on the left side of the upper jaw. Preliminary radiographic assessment showed bone thickness of 3–4 mm in the corono-apical and 6–7 mm in the bucco-palatal direction. After a preliminary assessment, planning for the operation began. It was decided to carry out rehabilitation using an orthopedic structure supported by three implants with simultaneous sinus lift without the use of a graft.
In this case, three 3.75 x 11.5 implants (MIS Seven; MIS, Barlev, Israel) were placed for immediate loading. Preoperative cone beam computed tomography determined the diameter and location of the AAA in the anterolateral sinus wall (Fig. 1). The course of the vessel was determined to be intraosseous, and CT images made it possible to correctly plan the bone windows. The course of the vessel was marked with a surgical pencil on the side wall of the sinus after making an incision and folding back the mucoperiosteal flap.
Rice. 1. Preoperative CBCT scanning allowed us to study the location of the AAA in the anterolateral wall of the sinus and the variability of its diameter.
Is it painful to do?
The procedure in most Russian clinics is performed under local anesthesia.
In our Center we use short-term combo sedation
This is not anesthesia and does not require tests or long preparation. This is a modern and safe sleep treatment, but without complete immersion.
Levin Dmitry Valerievich
Founder and Chief Doctor of the Center
The use of drug sedation is the best option - the patient is in a calm, half-asleep state and can easily tolerate treatment procedures. The operation is not accompanied by unpleasant sensations, and to relieve pain during rehabilitation, the doctor prescribes analgesics; all medications will be given to you immediately after the operation; you do not need to go to the pharmacy. If recovery proceeds without complications, long-term use of painkillers will not be required, usually no more than three days.
In clinical practice, a situation often occurs when the volume of bone tissue is insufficient for ideal placement of a dental implant. In these cases, additional structural support is required, which is provided by bone grafting.
Sinus lift and alveolar ridge augmentation are procedures with the highest success rate and are used in 10-20% of patients requiring dental implants. Since the 1980s, treatment has been carried out using various natural or synthetic bone materials, the range of which is expanding.
Bone regeneration procedures are becoming increasingly important with the acceptance of the concept of dental implantation as an ideal option for dental rehabilitation.
These procedures are critical to the success of dental implantation in cases where there is a significant deficiency in bone height or width. The cornerstone of successful treatment is considered to be the correct choice of bone material to form a bone mantle that securely covers the implant.
The effectiveness of bone material for sinus lift is a decisive factor in the stability of the dental implant and the final treatment result. To do this, the material must be osteogenic, osteoinductive, osteoconductive and biodegradable.
Anatomical Basics
The alveolar process of the maxilla has a compact, high-density cortex and internal porous cancellous bone filled with bone marrow.
The bone is pierced by cylindrical canals called Haversian canals and contains blood vessels that supply it with nutrients and oxygen.
Bone cells include osteogenic cells and osteoclasts, which vary in structure and function. Osteogenic cells are divided into osteoprogenitor cells, prosteoblasts, osteoblasts and osteocytes. Mesenchymal cells first turn into osteoprogenitor cells, and then into preosteoblast cells, which, in turn, transform into osteoblast cells.
Osteoblasts produce what is called osteoid, a non-calcified matrix that contains collagenous and non-collagenous protein bone matrix. Osteoblasts also secrete several cytokines and bone morphogenetic proteins (BMPs).
Cytokines and hormones play an important role in bone regeneration. When osteoblasts stop producing matrix, they turn into osteocytes and sink into calcified bone.
Sinus lift techniques
Lack of bone volume can be treated with various bone grafting techniques before implant placement. Boyne and James (1980) were the first to propose augmentation of the maxillary sinus floor using autologous bone graft.
The technique was significantly modified and improved by Tatum (1986), who introduced a lateral approach by fenestration of the buccal wall of the maxillary sinus, with elevation of the Schneiderian membrane. This method was modified by Wood and More in 1988.
The maxillary sinus floor augmentation procedure can be divided into two techniques. The first is called the osteotomy technique and is performed using osteotomes to create a controlled incision in the floor of the maxillary sinus.
This technique creates space by lifting the mucosa, which provides enough space for the dental implant and bone graft material.
The advantage of the technique is that it is less invasive and therefore reduces operative time and reduces the risk of complications. This technique is recommended when the vertical bone height exceeds 4-6 mm.
The second technique is the lateral window method, which is performed by surgically preparing the bone lateral to the maxillary sinus. During the procedure, the Schneiderian membrane is exposed, which will be lifted during the operation.
The bone material for sinus lift is carefully placed at the bottom of the sinus. This technique is more invasive than using an osteotome due to the fenestration of the lateral wall of the maxillary sinus.
The side window technique is preferred when the residual bone height is less than 6 mm.
Bone healing process
Bone healing after filling with bone material occurs in two stages: regeneration with an inflammatory response and subsequent bone remodeling.
In the first stage, a blood clot forms in the damaged area, where the outer part of the bone becomes necrotic. Capillaries begin to form, and further migration of inflammatory cells - lymphocytes, granulocytes, monocytes - is observed.
This process is accompanied by restoration of blood flow, and after 1-3 days the inflammatory reaction is activated with the formation of granulation tissue. The latter turns into a collagen matrix, and mesenchymal stem cells begin to differentiate into osteoblast cells, forming new bone.
During the second phase, the bone is remodeled, replaced by more mature lamellar bone. Complete healing of the defect occurs when the entire bone undergoes remodeling.
Bone materials for sinus lift
An ideal bone material (graft) should have osteoinductive and osteoconductive properties, as well as the ability to integrate with the surface of the implant. These properties in modern materials are expressed to varying degrees.
Osteoinductive properties are provided by primitive, undifferentiated pluripotent cells, which transform into osteogenic cells and are responsible for the process of osteogenesis. Osteoconductive properties refer to the ability of a material to promote bone growth on its microrelief surface.
It is assumed that the ideal bone material for sinus lift allows the induction of new bone formation through capillary infiltration and provides support for dental implants with a sufficient amount of intact bone tissue.
For this purpose, autologous bone, allogeneic, xenogeneic and synthetic bone materials are placed in the maxillary sinus. Let's take a closer look at these groups.
Autogenous bone material
Autogenous material, or autograft, is bone tissue obtained and implanted back into the same person. Therefore, the autograft must be taken from one part of the body and transplanted to another, performing additional surgery.
The cellular component of a cancellous bone graft contains a small number of osteoblasts and many progenitor cells that survive grafting. These progenitor cells explain the high osteogenic potential of the autograft.
Autogenous bone material for sinus lifting is rightly considered the gold standard, since it has the listed osteoinductive, osteogenic, osteoconductive properties, as well as the ability to osseointegrate.
However, autografts have significant disadvantages that limit their practical use. Firstly, there is the need to perform two interventions with associated risks of complications and pain. Secondly, there is a limitation on the number, shape and size of the grafts obtained.
Autogenous bone material is divided into two groups - cancellous and cortical.
After transplantation, most of the cells present in the cancellous autograft die due to ischemia. Mesenchymal stem cells present in the bone marrow are resistant to ischemia and are able to survive the procedure.
The ability of stem cells to survive and proliferate after detrimental changes in oxygenation, pH, and cytokine milieu is the primary reason for the reliability of trabecular bone autotransplantation interventions.
Incorporation of cancellous bone occurs rapidly, within approximately 8 weeks.
Cortical autografts are segments of compact cortical bone that provide osteoconductive support for new bone formation but do not provide significant numbers of viable osteogenic cells.
For this reason, revascularization and integration of cortical autografts is slow. Their main advantage is mechanical support.
Allogeneic bone material
Allogeneic bone material, or allograft, is tissue collected from one individual and implanted into another within the same species.
The use of cadaveric bone tissue to obtain an allograft is considered a more affordable alternative to autografts due to similar biological characteristics.
Despite the superior properties of autograft, allogeneic material is usually preferred by patients who do not wish to undergo additional surgery.
Lyophilized bone allograft (FDBA) and demineralized freeze-dried bone allograft (DFDBA) for dental use are prepared in special jars.
The source of FDBA and DFDBA is the cortical bone tissue of long bones, which is characterized by an increased content of bone morphogenetic proteins and lower antigenic activity compared to cancellous bone.
Bone allografts are produced in a variety of forms and types, including powder, cortical chips, cancellous bone cubes, and cortical granules.
Granular bone material is produced by grinding cortical bone under sterile conditions to produce particles ranging in size from 250 to 750 micrometers.
Currently, different forms of bone blocks for sinus lift are available, the mechanical properties of which are slightly inferior compared to bone blocks of cortical autogenous bone.
After harvesting the allograft, it is processed in several ways:
- physical treatment to remove soft tissue and reduce cellular load
- ultrasonic washing to remove cell and blood residues
- ethanol treatment to denature proteins and inactivate viruses
- Antibiotic flush to kill bacteria
- sterilization with gamma radiation and ethylene oxide to eliminate spores.
The FDBA is washed in antibiotic twice for an hour, frozen at -700C and dried until it reaches about 5% moisture.
Mineralized bone matrix does not have active bone morphogenetic proteins (BMPs). Therefore, it lacks osteoinductive properties, although it has osteoconductive properties.
Incorporation is qualitatively similar to an autograft, but occurs more slowly.
Cortical allografts ultimately resemble an autograft counterpart, although the former will have more necrotic bone tissue present.
Ground bone materials have an “open” structure that promotes blood cell penetration, improves graft incorporation, and allows mixing with blood, platelet concentrates, and other materials to form composites.
DFDBA is subjected to acid demineralization in 0.5-0.6 molar hydrochloric acid, resulting in 40% of the mineral content being removed, leaving the organic matrix intact. The technology preserves the BMPs present in the bone and therefore maintains its inherent osteoinductive properties.
In addition, the collagen matrix present in DFDBA acts as a scaffold that provides the material with pronounced osteoconductive properties.
The osteoinductivity of DFDBA was first described by Urist et al., who observed endochondral bone formation on a graft when placed in soft tissue. It was then discovered that bone morphogenetic proteins are key factors responsible for the formation of new bone.
BMPs are bound to the organic bone matrix and incorporated into the mineral content, so the demineralization process increases bioavailability. Bone morphogenetic proteins attract numerous mesenchymal stem cells and cause them to differentiate into chondrocytes, which form endochondral bone.
Endochondral ossification is associated with an osteoinductive response, while intramembranous bone formation indicates an osteoconductive response.
However, the osteoinductivity of DFDBA has recently been questioned because this property is highly dependent on manufacturing procedures.
The main advantages of allografts are availability, no need to obtain tissue from the patient, reduced need for anesthesia (general anesthesia is not required) and reduced surgical time.
However, many specialists avoid using cadaveric bone for transplantation due to the possible risk of transmitting infectious diseases.
Allogeneic bone materials are available in the form of granules and blocks.
The appearance of allograft granules is similar to other bone substitute granules; They are ideal for filling the bone cavities of defects of the alveolar process and maxillary sinus.
On the other hand, allogeneic bone blocks are particularly useful in both vertical and horizontal augmentation of areas of atrophied bone.
Xenogeneic bone material
Xenogeneic bone material for sinus lift is obtained from organisms other than humans. One of the most common xenografts is pure skeletal hydroxyapatite (HAP), or inorganic bovine bone.
Skeletal hydroxyapatite has ultrastructural features similar to human bone. Hydroxyapatite undergoes special treatment to remove any organic components, so it can be used in dental practice without the risk of an immune response on the part of the recipient.
Thanks to multi-stage chemical and thermal treatment, hydroxyapatite is practically devoid of antigenic activity and does not cause an inflammatory response.
The structure of inorganic bovine bone is a system of wide interconnected pores with a diameter of 0.25-1 millimeters, which can be easily penetrated by blood vessels. This structure promotes the migration of osteoblast cells, ensuring the fastest possible treatment results.
Bovine hydroxyapatite can be 75% micropores with a total surface area of up to 100 square meters per gram. Such high porosity of the bone material should create optimal osteoconductive conditions for bone growth.
On the other hand, the increased porosity of HAp sometimes degrades the mechanical properties of the material and the initial stability. Hydroxyapatite lacks osteoinductive properties, and the use of granules can be technically difficult.
Moreover, bovine hydroxyapatite is not resorbable in vivo. HAP can be detected in the operated area 3-6 years after implantation, which confirms extremely slow resorption.
According to Skoglung et al., hydroxyapatite granules in sinus lift are detectable even after 44 months after surgery. The presence of unresorbed material particles within new bone tissue is undesirable because it can affect the quality of the formed bone and its remodeling.
Although skeletal hydroxyapatite is usually used in the form of granules, blocks of HAP are available. In general, HAP is suitable for vertical and horizontal augmentation of the maxillary alveolar ridge.
The disadvantage is the fragility of the material, which not only complicates the surgical procedure, but also interferes with the bone healing process.
Other varieties of xenogeneic bone blocks (porcine) show conflicting results and different mechanical properties.
Xenogeneic bone material continues to be intensively studied in the context of dental use, but there are currently significant gaps in the scientific literature in understanding its behavior in vivo.
Given the unlimited sources and accessibility, it remains the focus.
Synthetic calcium phosphate
Biomaterials based on synthetic calcium phosphate chemically resemble natural bone mineral. Calcium phosphate has a number of advantages during sinus lifting, including biocompatibility, osteoconductivity and osseointegration.
The material contains a high concentration of calcium ions with an alkaline pH, as a result of which it exhibits low resorption, although Ca2+-rich materials with a more acidic pH have higher resorption (dicalcium phosphate).
Synthetic calcium phosphates can be divided into high-temperature (tricalcium phosphate ceramics, hydroxyapatite, biphasic calcium phosphate) and low-temperature (so-called cements).
Such bone materials vary in their in vivo resorption rate, strength, alkalinity and acidity, and crystallographic structure.
As a rule, they are brittle materials and therefore should only be used in areas that do not bear high mechanical loads.
Hydroxyapatite (HAP) and beta-tricalcium phosphate (beta-TCP) are ceramics that are used primarily to treat bone defects and cavities.
Biological stoichiometric hydroxyapatite, with a Ca/P ratio of 1.67, is very stable and its very slow degradation is mediated by phagocytosis. Such deficiency is corrected by introducing impurities such as carbonate ions, silicon ions and other ionic species present in bone mineral.
There is also porous hydroxyapatite with native bone architecture and high resorption, which significantly enhances the tissue response of angiogenesis and new bone formation.
Discoveries in this direction led to the creation of apatite and calcium carbonate of artificial origin, preserving the architecture of living sources. For example, organic ox bone, coral apatite, some seaweed apatite.
Biphasic Calcium Phosphate is formulated to combine the benefits of both hydroxyapatite and beta-TCP. The ratio of 60% hydroxyapatite and 40% beta-TCP is the most common among commercial biphasic calcium phosphates.
Calcium phosphate cements are classified according to the end product of the reaction into hydroxyapatite and brushite cements.
Hydroxyapatite cement was first developed by Brown and co-workers, but since that time various compositions have been prepared and patented. These formulations include the anhydrous tetracalcium phosphate/dicalcium phosphate (DCPA) system, as well as the well-known beta-tricalcium phosphate system.
The setting reaction of hydroxyapatite cement occurs with a neutral reaction of the environment, which is a biologically favorable property.
Hydroxyapatite is low crystalline and the stoichiometry can be varied to produce hydroxyapatite with lower calcium content (Ca/P ratio up to 1.67).
These features and the development of carbonate apatite cement make it possible to regulate the biodegradation of hydroxyapatite cement.
Since the development of brushite cement by Mirtchi et al., these products have attracted interest as bone substitutes. They come in different formulations, including beta-TCP + monocalcium phosphate monohydrate (MCPM) and beta-TCP + phosphoric acid.
The setting reaction of brushite cements is a continuous dissolution/precipitation mechanism at low pH, since brushite precipitates at pH<6.
The relatively short setting time of brushite cements compared to hydroxyapatite-forming pastes depends both on the higher solubility of the raw material and on the higher rate of growth of brushite crystals compared to hydroxyapatite.
The main advantage of brushite is its higher biodegradability compared to hydroxypatite, due to its higher solubility under physiological conditions encountered during sinus lifting.
However, the in vivo conversion of brushite to hydroxyapatite is kinetically unfavorable, so special additives have been patented to inhibit this conversion.
This fact attracted attention to the anhydrous form of brushite, monetite, which is obtained by drying brushite. Monetite, due to its low solubility, is more stable than brushite and has not been reported to convert in vivo to hydroxyapatite. This allows for much more predictable biodegradation in clinical settings.
Biologically active glass
Among modern materials for sinus lifting, bioactive glass, or bioglass, occupies an important place. This is the commercial name of the first calcium-substituted silica that was proposed for bone regeneration more than 30 years ago.
Bioglass emerged as a result of many years of work by American researchers during the Vietnam War. The US government has set a goal to develop a new biomaterial for bone grafting in wounded soldiers.
Bioglass has a large surface area, which is alkaline and actively interacts with blood plasma ions. This feature allows hydroxyapatite to be rapidly deposited on the surface after implantation in vivo.
This phenomenon is called biological activity and is one of the unique characteristics of bioglass, which allows it to quickly integrate into bone tissue.
Bioglass is suitable for bone regeneration in dental implantology. The material is 100% synthetic, so it does not pose problems associated with the transmission of infectious diseases or limited fabric sources.
However, the granules are difficult to process due to the repulsive charges between their highly charged surfaces. This makes its clinical handling more skill-demanding than other biomaterials.
The most important component of bioglass is silicon dioxide SiO2, which accounts for 45-60% of its mass. The first biologically active glass created for bone regeneration consisted of four components: SiO2, Na2O, CaO and P2O5.
However, the original composition was prone to crystallization, so it was modified to a more stable composition of Na2O, K2O, MgO, CaO, B2O3, P2O5 and SiO2.
In vivo experiments show that implanting bioglass into bone defects suppresses new bone formation in the early stages, but ultimately doubles the amount of bone tissue formed compared to other biomaterials.
Moreover, bioglass undergoes significant resorption within the first two weeks after implantation. After this point, the resorption rate stabilizes.
Upon implantation, the smaller ions present in the bioglass (i.e. Na+ and K+) tend to leach into the extracellular fluids. This results in the formation of a rich Si layer covering the biomaterial. Calcium and phosphate ions from body fluids react and precipitate in the silicon layer, forming hydroxyapatite.
Subsequently, the calcium phosphate layer adsorbs proteins on the surface. These extracellular entities attract macrophages, stem cells and osteogenic cells.
Bioactive glass can be used in the form of granules or preformed cones designed to be placed in fresh sockets to support the alveolar bone. This synthetic material has demonstrated clinical success in vertical augmentation and regeneration of intraosseous defects.
Despite the fact that bioglass is resorbed and promotes bone formation, the results of its use in maxillofacial surgery, as shown by numerous studies, are lower than those of calcium phosphate biomaterials.
Other sinus lift materials
An important role in the success of the procedure is played by platelet-rich plasma, which is obtained by centrifuging the patient’s blood. This product is mixed with calcium chloride, which has an anticoagulant effect and results in a high-tech mass with high stability.
Platelet-rich plasma delivers angiogenic growth factors to the lesion, which are designed to accelerate the process of bone tissue regeneration.
Conclusion
The materials described in the article simplify dental implantation when bone height is limited, increase the primary stability and survival of implants in the upper jaw, making treatment more successful and well tolerated.
Since the advent of dental implants, bone grafting has become an important procedure needed to treat patients with insufficient bone tissue.
Autologous bone graft, alone or in combination with other bone materials, is considered the biomaterial of choice for physicians around the world.
However, various xenogeneic, allogeneic, and synthetic biomaterials have shown promising results in bone tissue augmentation.
The basis for the success of dental implantation lies in proper treatment planning. It is important that a thorough examination of the patient tells the doctor the optimal choice of material for a particular clinical case.
The intervention technique and bone material should be selected depending on individual characteristics. Factors such as the osteogenic potential of the host's residual bone, the health status of the patients, and the morphology of the defects will determine the ideal bone substitute for each situation.
Restrictions after surgery
- You can't blow your nose;
- It is forbidden to drink through a straw;
- It is worth refraining from air travel;
- Food should be soft or semi-liquid; cold, hot, and spicy foods are prohibited;
- You cannot chew on the side where the operation was performed;
- During the first nights, it is recommended to sleep on high pillows with your head elevated so as not to provoke swelling;
- You cannot visit the bathhouse, swim, dive, you should exclude any physical activity, you need to rest;
- You need to take the medications prescribed by your doctor.
Read more about restrictions and recommendations here.
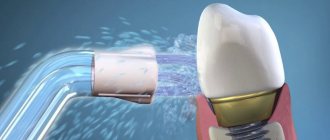
Bone material and membranes for sinus lift
Own bone
In the first case, the donor of the bone material is the patient himself - bone chips are taken from the chin or lower jaw area. Previously, it was believed that such a graft survives with minimal risk of rejection. However, the 30% risk of proven self-dissolution of the transplanted block forced us to abandon block transplantation many years ago. The second reason why we do not use this is that autogenous transplantation is more traumatic for the patient, since it involves surgical intervention in two places at once; rehabilitation is very memorable, especially in older patients.
Donor and artificial bone
An alternative material is donor bone taken from another person or animal, as well as artificial substances. In this case, the risk of rejection is higher, although the materials are always processed to improve survival rate. There are observations that prove that when using donor blocks it is impossible to guarantee the ideal biological purity of samples. Difficult choice for hygienic and ethical reasons.
Osteoplastic stimulators of bone regeneration
The best option, but the most expensive. There is no need to transplant a bone from a leg, and there is no need to transplant foreign bones either. A very quiet and honest bone growing technology. Genuine American growth stimulants cost from 22,000 rubles per mini bottle. Such stimulants are not found in network clinics or “promotional implantation” clinics. There are a lot of Russian and Asian analogues, I can’t comment on the results of their use, I haven’t tried them.
Membranes
Resorbable membranes during sinus lifting perform an important barrier function - they separate the space in which new bone is formed from the rest of the cavity of the maxillary sinus. Over time, the membrane dissolves. The membrane is necessary to keep the osteoplastic material stationary.
conclusions
When performing a sinus lift, it is necessary to maintain the integrity of the mucous membrane of the maxillary sinus, however, due to the anatomical features and atrophy of the fundus of less than 1 mm, perforations of more than 5 mm occur and a bone autograft from the branch of the mandible is the optimal solution for restoring the integrity of the Schneiderian membrane, regardless of what bone material was used for augmentation maxillary sinus (autogenous, xennogenous or allogeneic). The advantages of this method: regardless of the size of the perforation, the surgeon can continue the planned manipulations (sinus augmentation and installation of dental implants). The method in which autologous bone graft was used for the purpose of primary stability of the implant is an alternative to the two-stage sinus lift technique. This method has the advantages of being one-step and reducing the integration time of bone material and dental implants.
Is sinus lift dangerous?
If the operation is performed efficiently, the doctor is competent and mentally healthy, and the patient follows the recommendations, then sinus lifting is not dangerous and this adventure will quickly be forgotten. After surgery, the most common complications are damage to the sinuses and perforation of the mucous membrane of the maxillary sinus, which can lead to severe inflammation and chronic rhinitis. Another complication is perforation of the installed implant into the maxillary sinuses. This happens if the young surgeon has not sufficiently studied their structure, and will definitely require removal of the implant and a new operation.
In the case where the operation was performed in a specialized clean surgical department, these are impossible, fantastic situations.
Sinus lifting is a frequent and effective operation for increasing the bone tissue of the upper jaw.
There are no real alternatives to it. Sometimes instead, as an alternative, they resort to basal implantation - a technique in which non-root-shaped implants are installed in deeper and denser bone layers that are not suitable for axial biomechanical overloads. A basal implant never “grows” into the bone, like a root-shaped implant, but is held in it by a special shape and thread. Therefore, over time, it loosens and becomes unstable, which has a bad effect on dental health, not to mention what a living person experiences when he finds out that all the suffering was in vain, he will have to remove the dental crowns and everything again for the second round. The use of short implants to avoid a sinus lift is considered unacceptable by reputable doctors. There is no guarantee of the quality of the implantation performed, the patient runs the risk of complications, but if the clinics have good lawyers, then in Russia they do whatever they want.
Levin Dmitry Valerievich
Founder and Chief Doctor of the Center
Possible complications
The outcome and success of the operation is determined by the clinical picture and the qualifications of the doctor. The likelihood of complications increases if you do not follow the dentist’s recommendations after surgery.
Possible complications include:
- Sinus damage. But they are immediately eliminated by the doctor.
- Infection of the surgical site. The first signs may appear during the operation or later, and the reason is a violation of recommendations for hygienic oral care.
- Displacement of the installed material, which occurs when the doctor’s recommendations are violated.
- In some cases, bleeding, swelling, and pain may occur in the area where the sutures are applied. In this case, you need to consult a doctor.
Price in Moscow
The cost of a sinus lift depends on several factors:
- sinus lift techniques;
- type, volume and authenticity of consumables;
- the number of membranes used, reinforcing pins;
- the presence of a special surgical operating unit;
- disposability of instruments
- qualifications of the anesthesiologist performing sedation;
- additional possibilities (probability of immediate implantation).
It is beneficial in a batch calculation, when implantation is immediately included and combined with a sinus lift operation in one visit. Thus, the complex includes all services for preparation for operations and their implementation, in one visit. Prices for sinus lifting in Moscow in all clinics are approximately the same, the work performed on average costs about 50,000 rubles per side, radical differences are determined only in additional consumables.
The main problem of choosing a comfortable price is that the harmony of cost is always regulated by savings on consumables and at the level of the work performer, the doctor’s competence is the main factor in explaining the price, the pretentiousness of the clinic has nothing to do with it.
Sign up for dental implantation at a discount:
— Can there be complications after an open sinus lift?
Yes. First of all, this is the appearance of sinusitis. If perforation of the mucosa occurs, sinusitis (inflammation of the maxillary sinus) will develop: the mucosa becomes inflamed, swells, begins to produce fluid, and accordingly, what was implanted under it enters the sinus through this hole. In another flora, the material introduced by the implantologist begins to become inflamed. Frontitis (inflammation of the frontal sinus) is the next complication that can occur after open sinus lift surgery. In the specialized literature, otitis media is also described as a complication.
— How do complications happen?
Not often today. Modern diagnostic methods make it possible to prevent troubles even before the procedure. For example, to diagnose a patient with chronic sinusitis, a thin mucous membrane in the sinus or its almost complete absence due to work in hazardous work or due to bad habits (heavy smokers). Also at the diagnostic stage, the degree of elasticity and thickness of the membrane is recorded so that it can be lifted and material placed under it.
— What does diagnostics include before sinus lifts?
A computed tomography scan of the jaws is required. It shows all the signs of chronic sinusitis, polyps, cysts or fluid in the sinus, the thickness of the mucous membrane (for a resident of any metropolis, moderate hypertrophy of the mucous membrane of 4 to 4 mm is normal. Products of dirty city air settle on the mucous membrane as a protective mechanism, and additional fluid begins to be released , to remove all settled harmful substances), polypous growths.
Computed tomography of the jaws before sinus lift is mandatory!
— What do you do after receiving this information?
If there are contraindications, the phase must first be sanitized.
— Do you do this on your own or together with the ENT?
Either independently or together with an ENT doctor. As a rule, patients with chronic sinusitis have ENT doctors whom they visit regularly. After sanitization of the sinuses by an ENT doctor, sinus lifting for the purpose of further restoration of lost teeth can be carried out after at least 5 months.
— What therapy is necessary after sinus lift?
Antibacterial therapy, vasoconstrictor nasal drops, antiseptic anti-inflammatory therapy (oral treatment) are required.
— What class of antibacterial drugs are used?
At the discretion of the doctor. Basically, these are drugs of the fourth generation of penicillin groups. They are most suitable for diseases of the nose and mouth area.
— What kind of rehabilitation is necessary after a sinus lift?
You cannot play sports, including dynamic sports, for at least three weeks. You can’t visit baths or saunas for three to four weeks. Nutrition in the postoperative period should be gentle. Smoking should be reduced to a minimum. Alcohol is also prohibited during this period. After a sinus lift, you should not go diving or fly in an airplane for the first month after surgery. Due to the pressure difference, the implanted material can move along the sinus, interfering with osseointegration.
— Do these restrictions apply equally to patients who have undergone open or closed sinus lift?
Yes. If the mass of the embedded material is more than 1.5 grams (this is a fairly large amount). I recommend not flying or playing sports for up to two months, because 1.5-2 grams of bone tissue is a lot. The larger the volume of embedded material, the more time is needed for its integration.
— What symptoms should alert a patient after a sinus lift? What is normal and what should alert the patient?
In the first week - ten days, the norm includes swelling (in any case, it will appear and will last about five to six days), bruising on the skin, minor nasal discharge (especially in the morning after sleep), minor bloody discharge from the nose, temperature up to 38C within 3-4 days after surgery. The degree of swelling depends on the volume of intervention, on the skill of the dental surgeon: the smaller the incision, the area of intervention, the less swelling. Also, in women, swelling is greater due to the larger volume of subcutaneous adipose tissue. Signs of inflammation (fever after 4 days from surgery), aching, unpleasant pain, and suppuration from the nose are not normal. If these signs appear, you should immediately consult your doctor.
— What does a doctor do when a patient presents with similar symptoms after a sinus lift?
Sometimes you have to prescribe antiseptic drugs, antibiotic drops, and observe for several days. If there are no serious ruptures of the mucous membrane, then everything will return to normal. Not often, but it happens that you have to sanitize and wash everything. But such cases are extremely rare.
— Does sinus lift always involve simultaneous implantation?
This operation is performed for the further installation of a dental implant. There are cases when this happens in one operation (most often), but it happens that the installation of the implantation system is carried out as a second stage after some time.
Open bilateral SINUS lift. Video
— In what cases are procedures performed separately?
This depends on the extent of the bone tissue defect. First, you can do a sinus lift, wait until the bone tissue volume reaches the required level, and then carry out implantation.
— How long can the wait take?
Six to nine months. But, I repeat, in most cases it is possible to immediately install implants after a sinus lift. I think that for every 10 operations there are 2 where it is impossible to install implants at once.
Thank you very much!