Toothache is a problem that almost every person is familiar with. It signals existing pathologies of the dental system, but not all people immediately turn to dentists. This is due to patients’ fear of the painful sensations associated with visiting the dentist’s office. These fears are completely unfounded, since the anesthesia used in dentistry allows for high-quality anesthesia of the area in the oral cavity where manipulations will be performed.
Local anesthesia in dentistry: types and preparations
In dentistry, both therapeutic and surgical, different types and techniques of anesthesia are used, for example, conduction, infiltration, intracanal, intraosseous, intraligamentary (intraligamentous), tuberal and others. Their differences lie in the place of application and in some features of their effects. As a rule, modern dental clinics in Moscow use carpule anesthesia. This means that the anesthetic is supplied in disposable carpules - a kind of cartridges with an anesthetic solution that are inserted into syringes with screw-on disposable needles. Due to this, the carpules remain sterile, since the dentist does not have to open them, thereby eliminating contact of the medicine with air.
What to do if you are afraid of anesthesia -
Indeed, an anesthetic injection can be painful. The pain will depend both on the patient’s pain sensitivity threshold and on the doctor’s anesthesia technique. According to the rules, a solution of one anesthetic carpule (1.7 ml) is excreted into the tissue within 40-45 seconds. If the doctor saves time, then it is logical that rapid administration of the solution will cause pain.
To reduce the discomfort from an anesthetic injection, you can ask the doctor to first use a gel or spray with lidocaine to conduct topical anesthesia at the site of the future injection. You can also ask your doctor to administer the anesthetic slowly.
Drugs to relieve fear and anxiety – There are also drugs that can reduce fear and anxiety before an upcoming trip to the dentist. At the same time, there are drugs with a sedative effect such as (Persen forte), and there are drugs only for relieving anxiety, for example, Afobazol. The latter does not have a sedative effect, and it makes sense to start taking it only 10 days before going to the dentist, because... the drug has a cumulative effect (24stoma.ru).
In a number of large clinics, as a premedication, you can also be given an intramuscular injection of diphenhydramine 30 minutes before the start of treatment. You can also use tinctures of valerian, motherwort, Corvalol, valocardine. However, it is also advisable to take these drugs in a course (at least a few days before visiting the doctor), because they also have a cumulative effect. But you need to take into account that these drugs also have a hypnotic effect, which is not very good for motorists and working people.
Conduction anesthesia
Conduction anesthesia is aimed at blocking the nerve through which the pain signal is transmitted. In this way, it is possible to “turn off” a significant area of the jaw associated with the nerve that was exposed to the drug for a fairly long time - from an hour to an hour and a half. As a rule, conduction anesthesia is prescribed if extensive intervention is required on several molars and adjacent soft tissues. With the conduction method, the anesthetic is administered in close proximity to the nerve, and it is very important to correctly calculate this location, since if it is too far from the nerve, pain relief may not occur, and if it gets into the nerve itself, a complication such as neuropathy may develop . According to statistics, neuropathy occurs in 1% of cases and most often completely recedes within a year. By the way, when conducting conduction anesthesia in dentistry under ultrasound guidance, its safety and effectiveness are significantly increased.
Topical anesthesia in dentistry and drugs
Infiltration or application anesthesia in dentistry is carried out by soaking soft tissues with an anesthetic solution, as a result of which the nerve endings located in the treated area are blocked. With topical anesthesia, the anesthetic is applied without the use of a syringe. Using a cotton swab or your fingers, apply a small amount of the product, which subsequently penetrates approximately 3 mm inside and numbs the selected area. In dentistry, it is used to perform simple and quick operations associated with anesthesia of the oral mucosa, since it lasts, on average, from 10 to (in rare cases) 25 minutes. It is often preceded by subsequent injection anesthesia, especially if the patient is a child or is afraid of injections. There are also preparations for topical anesthesia in the form of aerosols. They are not widely used in dentistry due to difficulties in calculating dosage, as well as easy penetration into the respiratory tract and bloodstream, which increases the risk of complications.
Using a vasoconstrictor
The choice of dilution of the vasoconstrictor depends on the expected duration of the intervention and the presence of concomitant pathology in the child. As a rule, the duration of treatment for a child does not exceed 20-30 minutes. Longer intervention negatively affects the child’s psyche and his attitude towards dental treatment. In particular, fatigue increases, attention decreases, and the need for physical activity arises. All this disrupts cooperation between the doctor and the child, which is sometimes achieved with great difficulty.
In most cases, when treating caries and its complications, removing temporary teeth, there is no need to provide long-term anesthesia with anesthetics with a high content of epinephrine (1: 100,000) (Rabinovich S. A., Zoryan E. V., 2006).
After dental treatment, it is important to warn parents that the child can injure the tissues of the lips and cheeks without feeling them after local anesthesia. The duration of the “numbness” period is on average 2 hours for anesthetics 1:200000 and 5-6 hours for anesthetics 1:100000. Naturally, a long period of “numbness” of soft tissues is unfavorable and can lead to injury (the child, without feeling pain, bites the “numb” tissue), which in some cases can lead to extensive wound defects and subsequent deformation of the red border of the lips.
The doctor must be aware of the full extent of responsibility when using anesthetics 1:100000, which provide unreasonably long anesthesia. When administering anesthesia to children, especially for the first time, it is imperative to warn parents and talk with the child about the possibility of self-injury of soft tissues that are “numb” from anesthesia.
ANESTHETICS WITH HIGH VASOCONSTRICT DILUTION 1:100000
In pediatric practice, they are used only for a number of surgical interventions for the purpose of hemostasis. The duration of anesthesia is 75 minutes for dental pulp and 360 minutes for soft tissues.
Such outpatient interventions include the removal of an impacted, supernumerary tooth, apperculectomy, cystectomy, plastic surgery of the frenulum and vestibule of the oral cavity, and removal of a tumor. The use of anesthetics with high dilutions of epinephrine for other types of dental interventions is unjustified and disproportionate to the volume of intervention.
ANESTHETICS WITH LOW VASOCONSTRICT DILUTION 1:200000
Indicated for most outpatient interventions in pediatric dentistry. 4% articaine 1:200000 provides anesthesia for soft tissues for 180 minutes and dental pulp for 45 minutes, which satisfies the protocol for most outpatient interventions.
Currently, anesthetics based on 4% articaine with epinephrine 1:400000 have appeared in European countries. They provide anesthesia for dental pulp tissue for 20 minutes and soft tissue for 1 hour. This anesthetic provides the duration of anesthesia required by the doctor and a short period of “numb” tissue, which is so important for pediatric patients. Currently, these anesthetics are not certified in the Russian Federation, but work is underway to introduce them into domestic dentistry.
It is also worth noting that there is no difference in the depth of anesthesia and effectiveness between anesthetics with vasoconstrictors 1:100000, 1:200000 and 1:400000. There is a difference only in the duration of local anesthesia of the dental pulp: 25, 45 and 75 minutes, respectively. Many dentists mistakenly divide anesthetics into “strong” (1:100,000) and “weak” (1:200,000). This statement is misleading.
For short-term interventions in children with concomitant pathologies, the use of anesthetics without a vasoconstrictor is indicated. However, their use does not guarantee complete safety and does not reduce the risk of complications. It is worth noting some of their pharmacological features. Vasoconstrictors are added to the local anesthetic solution not only to increase the duration of pain relief, but also to reduce their toxicity.
The fact is that all anesthetics have a vasodilating effect and undergo fairly rapid absorption into the bloodstream. The addition of a vasoconstrictor slows the absorption of the anesthetic and prolongs its action. When using an anesthetic without vasoconstrictors, this effect does not occur. The anesthetic is forced into the blood, which can lead to a toxic reaction. This complication is possible if the permissible dosage is exceeded, which is different for anesthetics with and without a vasoconstrictor. In summary, it should be noted that anesthetics without a vasoconstrictor do not affect the functioning of the cardiovascular system, are less allergenic since they do not contain preservatives, but due to accelerated absorption they are toxic and safe to use only if the dosage is observed.
ANESTHETICS WITHOUT VASOCONSTRICTER
Provide varying durations of pain relief for dental tissues. In particular, 2% lidocaine provides anesthesia of the dental pulp within 5 minutes, while the rate of onset of anesthesia is also 5 minutes, which is unsatisfactory for the doctor. Therefore, the use of 2% lidocaine without a vasoconstrictor is inappropriate for dental anesthesia.
3% mepivacaine, in comparison with other anesthetics, has a less pronounced vasodilator effect, which makes it possible to use it without adding a vasoconstrictor. The anesthetic provides pain relief for 10-20 minutes, while treatment must be carried out from the 5th to 20th minute during therapeutic interventions and from the 10th to 20th during tooth extraction surgery.
Articaine 4% is currently available in the Russian Federation. This anesthetic is short-acting: anesthesia of dental pulp for 6 minutes, soft tissue for 45 minutes. Its widespread use in pediatric dentistry is limited due to its short action, which is not suitable for most interventions.
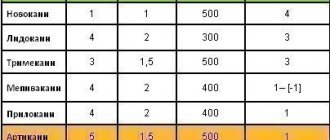
DOSAGE
In all cases of local anesthesia, it is necessary to calculate the dosage of the administered anesthetic in terms of the child’s body weight. For articaine preparations with a vasoconstrictor, the recommended dosage is 5 mg per 1 kg of weight. Before performing local anesthesia, the child’s weight is checked with the parents. In clinical practice, it is convenient to use a table with weight and the maximum permissible dose of the administered anesthetic (Table No. 1, 2).
Table No. 1
| WEIGHT | MG | ML | CARPOOLS |
| 10 | 44 | 1.5 | 0.8 |
| 15 | 66 | 2.2 | 1.2 |
| 20 | 88 | 2.8 | 1.4 |
| 25 | 110 | 3.6 | 1.7 |
| 30 | 132 | 4.4 | 2.4 |
| 35 | 154 | 5.1 | 2.9 |
| 40 | 176 | 5.9 | 3.2 |
| 45 | 198 | 6.6 | 3.6 |
| 50 | 220 | 7.3 | 4.0 |
| Mepivacaine 3% without vasoconstrictor. Maximum dose 4.4 mg/kg. 3% solution in 1 carpule 1.8 ml (54 mg). | |||
Table No. 2
| WEIGHT | MG | ML | CARPOOLS |
| 10 | 50 | 1.2 | 0.69 |
| 15 | 75 | 1.9 | 1.0 |
| 20 | 100 | 2.5 | 1.4 |
| 25 | 125 | 3.1 | 1.7 |
| 30 | 150 | 3.7 | 2.1 |
| 35 | 175 | 4.4 | 2.4 |
| 40 | 200 | 5.0 | 2.8 |
| 45 | 225 | 5.6 | 3.1 |
| 50 | 250 | 6.2 | 3.4 |
| Articaine 4% with a vasoconstrictor. Maximum dose 5 mg/kg. 3% solution in 1 carpule 1.8 ml (72 mg). | |||
Quite often, at outpatient dental appointments we encounter children suffering from obesity and metabolic syndrome, which is largely due to changes in the nutritional culture of the population. The dosage of the administered anesthetic in these cases has some peculiarities. In particular, if the doctor is going to administer anesthesia to an overweight child, the dosage of the administered anesthetic is calculated without taking into account adipose tissue.
Infiltration anesthesia
This is one of the most common methods of anesthesia in modern dentistry. There are two types of infiltration anesthesia: direct and indirect. Direct anesthesia is injected directly under the mucous membrane near the teeth that require treatment, and acts at the injection site. Indirect spreads to surrounding tissues and covers a larger area, while its prevalence depends on the type of surrounding tissues. For example, on the upper jaw the alveolar process is more porous, while on the lower jaw it is denser, which means that the effect of infiltration anesthesia on the upper jaw will be more effective.
Intraligamentary anesthesia
Intraligamentary anesthesia is also called intraligamentous and intraperiodontal. Its difference is in higher pressure when administering an anesthetic, which ensures uniform spreading of a small amount of the drug in the periodontal space, as well as its penetration into the intraosseous space. Drugs should be administered very slowly. When using this type of anesthesia, significantly less drug is required than with conventional infiltration; it occurs within 15-45 seconds and lasts for 20-30 minutes. For intraligamentary anesthesia, special syringes are often used, which make it possible to administer the drug under the required pressure without unnecessary effort and thus achieve the best result.
Intraosseous anesthesia
Intraosseous anesthesia in dentistry is chosen when infiltration or conduction anesthesia is ineffective. It is usually performed in the area of the lower molars and is indicated for treatment, tooth extraction and operations on the alveolar process. However, it is rarely used due to the complex technique of execution: it is necessary to dissect the mucous membrane, then make a hole in the bone with a special bur with a diameter equal to the size of the syringe needle in order to direct the syringe directly to the spongy substance. The drug should be administered slowly, under high pressure.
Among the advantages of this type of anesthesia is significant efficiency; a small amount of even a weak anesthetic is sufficient. Among the disadvantages are the complexity of implementation, as well as serious risks of complications if the drug enters the bloodstream, which is likely due to accidental damage to a vessel.
FEATURES OF PAIN RELIEF OF TEMPORARY TEETH
Of course, the choice of pain relief method depends on the planned intervention.
In the treatment of caries and pulpitis of temporary teeth, preference is given to infiltration methods carried out from the vestibular (buccal/labial) side, and there is no need for lingual or palatal anesthesia. This is explained by the predominance of spongy substance and a large number of nutrient openings in the structure of the jaw bones, facilitating the diffusion of local anesthetic.
In order to reduce the degree of pain of the injection and increase the level of comfort for the child, the following recommendations for local anesthesia should be followed:
- A preliminary distracting preparatory conversation with the child is necessary, during which the doctor uses terms that the child understands. In this case, the words “injection”, “syringe”, “anesthesia”, “removal”, “needle” are not pronounced.
- The child should not see (look at) the injection equipment. All instruments are presented by an assistant out of sight of the child.
- Application anesthesia should be performed so that the child does not feel the puncture stage of the mucous membrane.
- The rule must be observed: “one needle, one injection.” If the needle accidentally comes into contact with the bone tissue of the jaw, its tip is deformed; as a rule, it bends in the direction opposite to the bevel. A repeated injection with the same “dull” needle in another segment will involve applying pressure that is unpleasant for the child.
- The anesthetic should be injected slowly, 1 ml/min. Forced administration of the anesthetic leads to hydrodynamic tissue trauma, which causes pain.
- Two-stage injection of a portion of anesthetic. When performing infiltration anesthesia, the doctor initially injects a small amount of anesthetic? 0.1 submucosally, while a zone of tissue infiltration the size of a millet grain is visually determined. Next, the doctor talks with the child for 2-3 minutes.
- The subsequent administration of the main portion of the anesthetic is painless.
- The temperature of the anesthetic solution should be close to the child’s body temperature. To do this, do not store anesthetic carpules in the refrigerator. Before the injection, the doctor can “warm” the carpule in his hand or in running hot water.
The volume of injected anesthetic for infiltration anesthesia of temporary incisors and canines is on average 0.3 ml; for anesthesia of temporary molars, 0.5-0.6 ml is used. Subperiosteal anesthesia should not be performed as this will cause pain to the child and will not increase effectiveness. The needle should move submucosally towards the apexes of the roots of the teeth. In the upper jaw, when performing infiltration anesthesia, one should not insert a needle into the area of the frenulum of the upper lip, mucous strands in the area of temporary canines. These areas have an extensive network of nerves, providing hypersensitivity in these areas.
When performing an operation to remove temporary teeth of the upper jaw with a diagnosis of periodontitis, various combinations of infiltration methods are used. In the upper jaw, when removing incisors and canines, infiltration vestibular (0.5 ml) and incisal anesthesia (less than 0.2 ml) is used. In this case, classical conduction anesthesia with the advancement of the needle into the incisive canal is not carried out, but a certain amount of anesthetic is injected on the side of the incisive papilla, until signs of ischemia appear. If possible, painful incisal anesthesia should be avoided, which can be replaced with topical anesthesia or by inserting a needle into the vestibular interdental papilla and then moving it to the palatal side with a continuous supply of anesthetic.
When anesthetizing the first and second temporary molars, infiltration vestibular (0.5-0.6 ml) and palatal (0.2 ml) anesthesia is used. Palatal anesthesia can be replaced by the above-described approach through the interdental papilla. To reduce the degree of pain of local anesthetic injection into the hard palate, preliminary application anesthesia should be used.
When removing temporary teeth of the lower jaw with a diagnosis of periodontitis, a combination of conduction and infiltration methods is used. When removing incisors and canines, infiltration vestibular (0.3 ml) and lingual (less than 0.2 ml) anesthesia is used. Lingual infiltration anesthesia is performed in the area of the transition of the attached gum to the mobile mucosa of the floor of the mouth. The anesthetic is injected into the submucosal layer; the needle is not advanced to prevent intravascular injection.
You can anesthetize the lingual mucosa by inserting a needle into the interdental papilla from the vestibular side and then moving it towards the lingual mucosa. When removing temporary first molars of the lower jaw, the above-described technique is used with the only difference that 0.5 ml of anesthetic is injected from the vestibular side of the tooth being removed. In the presence of local inflammation, it is necessary to perform conduction mental anesthesia. When removing the second temporary molars of the lower jaw with a diagnosis of periodontitis, either mandibular anesthesia (1 ml) or a combination of mental anesthesia (0.6 ml) and lingual infiltration (0.2 ml) is performed.
During the period of physiological change in occlusion, the removal of temporary teeth for orthodontic indications has some features. The most common mistake is removing a “moving” tooth under application anesthesia. The depth of application anesthesia is 2-3 mm of the mucous membrane, and the roots of the tooth may not be completely resorbed, and their removal will be painful. Application anesthesia can be used as an independent method only if the tooth is fixed by mucous membrane on one edge. In other cases, infiltration anesthesia should be performed. The anesthetic is administered before signs of gum ischemia appear; its volume is minimal.
Intracanal anesthesia
The intracanal method of pain relief speaks for itself. Typically, intracanal anesthesia in dentistry is carried out in this way: using a drill, a hole is made in the tooth corresponding to the diameter of the needle, and the drug is injected directly into the pulp or deeper into the canal. Sometimes the carious cavity itself is used for this. If we are talking about the intraligamentary technique, then we mean the introduction of a local anesthetic solution into the space at the root of the tooth (periodontal), and the tuberal technique means the introduction of a substance into the posterior alveolar branches of the upper jaw.
Tuberal anesthesia
Tuberal anesthesia is so named in connection with the injection site - the tubercles of the upper jaw, which are called tuber in Latin. The posterior alveolar nerves are located here, innervating the area of the alveolar ridge from the third to the first molar. This type of anesthesia is the most dangerous in terms of possible complications due to individual differences in the structure of this area and the location of nerves and blood vessels in it. There are intraoral and extraoral methods of administering tuberal anesthesia. It is believed that the intraoral method is more likely to cause injury, while the external method is safer and it is also easier to ensure adequate antiseptic treatment of the surface before injection.
What are the indications for tooth extraction?
Before tooth extraction surgery, the doctor prescribes an x-ray examination; the resulting images help assess the condition of diseased teeth.
- Detection of chronic periodontitis at the acute stage, when it is impossible to eliminate the source of inflammation in the area of the apex of the tooth using therapeutic methods
- In order to prevent the development of more serious complications
- Diagnosis of basal (near-root) tooth cyst
- Presence of inflammation or trigeminal neuritis
- If a problematic tooth constantly injures the mucous membrane of the tongue or cheeks
- If a tooth puts pressure on adjacent teeth, injuring their roots, which leads to bone resorption
- If a problematic tooth disrupts the normal bite and displaces neighboring teeth
- Multi-rooted teeth that have caused odontogenic osteomyelitis must be removed
- Sometimes the doctor prescribes tooth extraction to fit a removable denture
- With severe destruction by carious lesions
- If the tooth has not fully erupted and has an incorrect angle
- Due to progressive periodontal disease
- Due to an injury that resulted in a tooth fracture beyond repair
- If the teeth are in an incorrect position in the dentition (this situation is often detected during the eruption of wisdom teeth)
Subsequently, the removal of a tooth causes a gradual displacement of adjacent teeth; with prolonged absence of a tooth, this can lead to significant impairment of chewing function and noticeable deformation of the entire dentition. In order to prevent such complications, it is recommended to restore the extracted tooth by replacing it with an artificial one.
Modern dental practice has wide capabilities in the field of operative surgery and implantology, due to which replacing a defect in the dentition by installing a dental implant is the most natural and preferable; depending on the clinical situation, the modern patient has access to the latest technologies for the manufacture of dental bridges or removable partial dentures.
Computer anesthesia
Computer anesthesia allows dentists to calculate more accurate doses of the drug, administer it at the desired speed, pre-selected by the computer, and painlessly guide the syringe needle, which has a special cutting edge. Anesthesia administered with high precision can last longer - up to 40 minutes, and visual and audio signals provided by the device allow the doctor to position the needle as needed, without the risk of tissue damage, introducing anesthetic into the bloodstream or placing the needle too far from the nerve.
Ultrasound anesthesia
When performing anesthesia, it is very important to choose the right injection site, since a mistake can lead to serious complications. This is especially true for conduction anesthesia, where the drug must be in close proximity to the nerve, but the needle cannot touch it. Ultrasound successfully helps determine the site of anesthetic injection. Under the control of an ultrasound machine, it is possible to calculate down to the millimeter the location of the needle and its proximity to the nerve, thereby ensuring the most effective and safe anesthesia of the desired area.
General anesthesia in dentistry
In some cases, the patient may require dental treatment under general anesthesia. As a rule, it is used when serious and long-term treatment is necessary, for example, the removal of several teeth at a time or complex operations on the jaw. An indication for the use of general anesthesia in dentistry may also be serious dental phobia or a disease in which a person cannot adequately communicate with the doctor, or he may have unexpected reactions to the doctor’s actions, as, for example, with epilepsy.
As an alternative to general anesthesia to correct mood and relieve fear of dental treatment, there is sedation in dentistry. It does not “turn off” consciousness, but puts you into half-asleep and calms you down, helps you relax, and perceive what is happening in a positive way. However, sedation is not anesthesia, so it is used in combination with local anesthesia.
Deep sedation with Propofol - drug-induced sleep
During dental treatment, anesthesia for children or deep sedation may be used. These concepts are often confused, since in both cases the child is immersed in medicated sleep. But the difference is significant:
- General anesthesia in dentistry is given to children through a mask. Artificial sleep is as deep as possible, with complete loss of sensitivity.
- Sedation with Propofol involves intravenous administration of the drug and requires additional pain relief.
Propofol guarantees:
- natural physiological state of sleep;
- falling asleep in 1-2 minutes;
- exceptionally high safety for the child;
- simple awakening and rested state;
- extremely low risk of allergic reactions and side effects.
The quality and depth of sleep is controlled by an anesthesiologist. At this time, dentists treat and save teeth, remove completely destroyed units, and install prosthetic structures.
When is anesthesia used in pediatric dentistry?
Most adults have a fear of dental treatment left over from childhood, so today one of the tasks of a pediatric dentist is to prevent the occurrence of dental phobia or get rid of fears that have already formed in the child. General anesthesia is often the only way to solve dental problems in children under three years of age, as well as in children with developmental disabilities, in particular with autism, Down syndrome, cerebral palsy or epilepsy.
It is not always necessary to carry out dental treatment in children under anesthesia. A small patient who comes to a kind and open doctor will be able to perform most of the manipulations while conscious. The main condition is that these manipulations must be painless. According to some studies, today the most painful procedure for a child is the anesthetic injection itself. That is why in pediatric dentistry, before an injection, topical anesthesia is used, the preparations for which have a pleasant taste, which contributes to a good mood in children and their cooperation with the doctor.
In addition, today in dentistry it is no longer uncommon to have a device for computer anesthesia, which allows painless administration of medicine and clearly measuring its correct dosage.
Modern anesthesia in dentistry: contraindications for use
The main contraindication to anesthesia in dentistry is an allergy to its components; side effects should also be taken into account, which are most often associated with the presence of additional substances in the anesthetic solution: vasoconstrictors, preservatives and stabilizers. In particular, it is necessary to especially carefully select drugs for patients with cardiovascular diseases, arterial hypertension, and decompensated forms of endocrine diseases (diabetes mellitus, thyrotoxicosis, and others). To determine which substances a person has a negative reaction to, the doctor sends him to the Institute of Allergology to perform tests. In accordance with these data, a safe drug for local anesthesia is selected, and in case of reaction to all groups of anesthetics, general anesthesia is used.
If you are planning a visit to the doctor, we advise you to observe a number of points:
- do not drink alcohol the day before, this may worsen the effect of the anesthetic;
- if you have a cold, cough, or runny nose, it is better to postpone your visit until you have fully recovered;
- Women and girls are not recommended to visit the dentist during menstruation, because... during this period, blood clotting worsens (by the way, do not be surprised if the anesthesiologist asks you this question before surgery; operations are not performed during menstruation.
- choose your clinic carefully! Now their choice is very large, but very few comply with important requirements and all antiseptic requirements!
What are the features of anesthesia in dentistry for pregnant women?
It is also important for pregnant women to ensure pain-free dental treatment. However, conventional painkillers are not suitable for them, since vasoconstrictors (also known as vasoconstrictors) are usually added to the anesthetic solution in order to keep it in the right place and prolong its effect. Vasoconstrictors also reduce potential common side effects and reduce bleeding. For example, adrenaline added to a four percent solution of articaine can extend its analgesic effect from three to forty-five minutes.
Only mepivacaine can be used without adrenaline, since, unlike other drugs for local anesthesia used in dentistry (articaine, which is considered the best option today, novocaine and lidocaine), it does not have the ability to dilate blood vessels at the injection site, which means it can be recommended for pregnant women, children, and other categories of patients who should not be administered adrenaline. These include, for example, those suffering from cardiovascular diseases, arterial hypertension, severe forms of diabetes mellitus, and severe thyrotoxicosis.
Sedation or anesthesia?
Sedation and anesthesia are two different things. Sedation does not disconnect consciousness from the outside world. It is more like a state of light dozing. However, it is also a medical exposure to the body that should be avoided. It is quite possible to manage only with anesthesia. If you are very nervous, you can do a breathing practice that will help you calm down.
Anesthesia is a more serious manipulation. It has a number of side effects:
- dizziness, nausea;
- severe thirst after the end of the effect, but you can’t drink;
- weakness;
- chills or, conversely, high temperature.
In addition, after recovering from anesthesia, you need to remain in bed for some time and limit physical and thermal stress.
The worst thing that can happen during anesthesia is cardiac arrest. This happens with incorrect diagnosis and incorrect selection of the dosage of the drug. However, it is best to avoid additional procedures beyond local anesthesia.