9151
This term originates from Latin and means “closure.”
Central occlusion is a state of evenly distributed tension of the jaw muscles, while ensuring simultaneous contact of all surfaces of the elements of the dentition.
The need to determine central occlusion is to correctly manufacture a partial or removable denture.
Main features
Experts have determined the following indicators of central occlusion:
- Muscular. Synchronous, normal contraction of the muscles responsible for the functioning of the lower jaw bone.
- Articular. The surfaces of the articular heads of the lower jaw are located directly at the bases of the slopes of the articular tubercles, in the depths of the articular fossa.
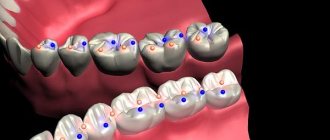
- Dental:
- full surface contact;
- opposite rows are brought together so that each unit is in contact with the same and the next element;
- the direction of the upper frontal incisors and the similar direction of the lower ones lie in a single sagittal plane;
- the overlap of the elements of the upper row of fragments of the lower one in the front part is 30% of the length;
- the anterior units contact in such a way that the edges of the lower fragments abut the palatine tubercles of the upper ones;
- the upper molar comes into contact with the lower one so that two-thirds of its area is combined with the first, and the rest with the second;
If we consider the transverse direction of the rows, then their buccal tubercles overlap, while the tubercles on the palate are oriented longitudinally, in the fissure between the buccal and lingual of the lower row.
Signs of correct row contact
Are common:
- the rows converge in a single vertical plane;
- incisors and molars of both rows have a pair of antagonists;
- there is contact between units of the same name;
- the lower incisors do not have antagonists in the central part;
- the upper eighths have no antagonists.
Applies to anterior units only:
- if we conditionally divide the patient’s face into two symmetrical parts, then the line of symmetry should pass between the front elements of both rows;
- the upper row of fragments overlaps the lower one in the anterior zone to a height of 30% of the total crown size;
- the cutting edges of the lower units are in contact with the tubercles of the inner part of the upper ones.
Applies only to lateral ones:
- the buccal distal cusp of the upper row is based in the space between the 6th and 7th molars of the lower row;
- the lateral elements of the upper row close with the lower ones in such a way that they fall strictly into the intertubercular grooves.
Let's find out together how dental impressions are made and what modern material is used.
Read here about the purpose of filing the front teeth.
At this address https://orto-info.ru/ortodonticheskoe-lechenie/podgotovitelnyiy-period/separatsiya-zubov.html we will talk about the consequences of teeth separation.
Signs of occlusion
The main signs of central occlusion are:
- muscular;
- articular;
- dental
In the latter case, it is necessary to determine what the surface contact will be and whether it is complete. It is necessary to determine how exactly the opposite rows are brought together, if there are any violations, what kind of overlap is for the top row. Also, when determining occlusion, the specialist looks at whether the upper molar comes into full contact with the lower molar, whether there is a coincidence or displacement.
Methods used
Central occlusion is determined at the stage of manufacturing prosthetic structures when several units are lost.
This is necessary to ensure the normal functioning of the product and eliminate the occurrence of deviations and problems in the functioning of the temporomandibular joints.
In this case, the height of the lower third of the face is of great importance. However, in the absence of a large number of units, this indicator may be violated and must be restored.
If the patient has partial adentia, several options for determining the indicator are used.
The presence of antagonists on both sides
The method is used when antagonists are present in all functional areas of the jaws.
In the presence of a large number of antagonists, the height of the lower third of the face is maintained and fixed.
The occlusion index is determined based on as many contact zones as possible of the same units of the upper and lower rows.
This option is the simplest, as it does not require the additional use of occlusal ridges or specialized orthopedic templates.
Presence of three occlusion points between antagonists
This method is used if the patient still has antagonists in the three main contact zones of the rows. At the same time, the small number of antagonists does not allow normal positioning of plaster casts of the jaw in the articulator.
In this case, the natural height of the lower third of the face is disrupted, and occlusal ridges made of wax or thermoplastic polymer are used to correctly match the casts.
The roller is placed on the bottom row, after which the patient brings his jaw together. After the roller is removed from the oral cavity, imprints of the antagonist contact zones remain on it.
These prints are subsequently used by technicians in the laboratory to position the casts and create a fully functional and correct, from an orthopedic point of view, prosthesis.
Absence of antagonistic pairs
The most labor-intensive scenario is the complete absence of the same elements on both jaws.
In this situation, instead of the position of central occlusion, the central relationship of the jaws is determined .
The procedure includes the following steps:
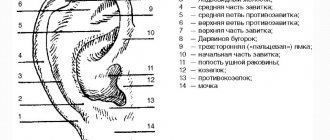
- Work on the formation of a prosthetic plane , which is positioned along the chewing surfaces of the lateral units and is parallel to the beam. It is built from the lower point of the nasal septum to the upper edges of the ear canals.
- Determination of the normal height of the lower third of the face.
- Fixation of the mesiodistal relationship of the upper and lower jaws using wax or polymer bases with occlusal ridges.
Checking central occlusion with existing pairs of elements of the same name is carried out by closing the teeth and is carried out as follows:
- a thin strip of wax is placed on the already prepared and fitted contact surface of the occlusal roller and glued;
- the resulting structure is heated until the wax softens;
- heated templates are placed in the patient’s oral cavity;
- After bringing the jaws together, the teeth leave imprints on the wax strip.
It is these fingerprints that are used in the process of modeling central occlusion in the laboratory.
If, during the process of determining occlusion, the surfaces of the upper and lower rollers close, the specialist adjusts their contact surfaces.
Wedge-shaped cuts are made on the upper one, and a certain amount of material is cut off from the lower one, after which a wax strip is glued to the treated surface. After the rows are brought together again, the strip material is pressed into the cutouts.
The products are removed from the patient’s mouth and sent to the laboratory for subsequent production of a prosthesis.
Central relation and central occlusion: analysis of relationships
Key concepts for applying occlusal knowledge to clinical practice include the ability to identify common occlusal problems and abnormalities, as well as associated changes in the temporomandibular joint (TMJ), which can then be used to inform patient care. In the presence of muscle pain, patients can be treated through the use of full or partial plates, which help to deprogram the muscles. At the same time, it is important to understand when and what types of devices are best to use. This article will describe the main approaches to the analysis and analysis of occlusion parameters, and methods for their implementation in clinical practice.
Introductory Occlusion Concepts
When applying occlusal concepts during restoration, the difference between centric relation and maximum fissure-tubercle position (MIP) must be clearly understood. In some cases, the doctor is able to identify the so-called “guide” tooth. This tooth allows the jaw to adapt and guides it into the desired position for closure when in contact with it in the stage of central occlusion. If during treatment a given tooth changes in some way, the occlusion is no longer stable and the complete rehabilitation procedure is noticeably worse. It is logical that it is best to avoid any iatrogenic interventions in the area of the “guide” tooth, since the chain of changes can lead to a change in the position of the joint and the location of the disc. In such cases, to restore occlusion, it is necessary to collect the entire set of additional diagnostic data, which will be extremely useful during further rehabilitation.
Determination of Central Ratio
The centric relation is the position of the joint in which it is in the most superior and anterior position in the glenoid fossa. Central relation should not be confused with centric occlusion, maximal intercuspation, adaptive centric posture, centric sliding, or centric stopping. The Glossary of Orthopedic Terms defines the centric relation as the relationship of the upper and lower jaws, in which the articular process interacts with the thinnest avascular part of the disc, and this complex of components is in an anterosuperior position opposite the corresponding form of the articular tubercle. Thus, the centric relation is in no way affected by tooth contact. Essentially, the joint should be in an anterior position, and how the teeth close together is the second question. Frank Spear defines centric relation as the position of the condyle in which the lateral pterygoid muscle is relaxed and the levator muscles are aligned with the properly positioned disc. The muscles try to pull closer and closer to the center, which in principle is quite normal and correct, if no disturbances are observed in the area of the joint as a whole, or the disc specifically. The centric relation is a position that is self-centering. For example, if a marble ball falls somewhere inside a cup, it will eventually roll into the center of the cup. If the patient has inflammation of the pterygoid muscle, which prevents the centering of the condyle, then this is the same as replacing the ball in the cup with a metal one, and attaching a magnet to the bottom of the cup - thus the position of the ball in the cup is predisposed. Similar processes occur in the area of the inflamed lateral pterygoid muscle.
Finding the central relation
The centric relation can be defined in several different ways.
The simplest, but least accurate method is for the patient to place his tongue on the back of the roof of the mouth and bite. This approach is useful for quick analysis, but in the author's opinion, its accuracy may leave much to be desired.
Another method for determining centric relation is to manipulate the jaw bilaterally (bilateral guide). This technique is very sensitive to perform. You need to create a C-shape between the thumb and other fingers, placing them on the lower jaw and chin. The patient is then asked to gently open and close his mouth, thereby allowing him to adapt to the movement. After several cycles of opening and closing, the dentist asks the patient to relax and, being careful not to provoke muscle activation, repeats the movements. At the same time, it is also important not to provoke distal positioning of the condyle, because the goal of this manipulation is to achieve its anterior and superior medial position.
The third method of finding the centric relation involves the use of an anterior deprogrammer. An instrument, such as a Lucia or quicksplint, is placed in the mouth with bite registration material. It is attached to the central incisors. The patient begins to move the lower jaw back and forth in a Lucia jig, relaxing the muscles. Once the muscles are relaxed, the patient is guided to bite on the distal plane. When the patient's jaw returns to its starting point, the condyle should sit strictly in the fossa. A similar technique to this approach is using a sheet calibrator. The sheet calibrator allows you to open the jaw by different amounts by removing or inserting one or more sheets of equal thickness between the teeth. Whether the sheet calibrator can actually provide jaw distalization is not yet known, but its very use is already more than useful. If the joint is healthy, the disc does not move and the muscles do not hold it in place. Therefore, the muscles can independently center the joint. A well-adjusted mouth guard that promotes muscle relaxation also helps to find centric relation. After recording the centric relation, it is important to determine the point of first contact. It is inherently a starting point for further treatment, but it cannot be detected in all patients. This point always needs to be marked, but not always in the literal sense (not always with a pencil, in other words). Photo 1 shows teeth No. 2 and No. 3. In this situation, the point of first contact is on the mesiolingual cusp of tooth No. 2, which has the strongest mark. However, a small but significant mark is also visualized on the distal buccal cusp of tooth No. 3. Let us repeat that the centric relation is the position of the joint and does not depend on the contact of the teeth. However, when the antagonist teeth are in contact in a state of centric relation, then this position is already called central occlusion.
Photo 1. First contact points.
Search for central occlusion
Maximum intercuspidation is the term used for habitual occlusion when the patient experiences the maximum number of opposing tooth contacts. Central occlusion can be determined using bilateral manipulation, a bilateral guide (Figure 2), or a sheet calibrator (Figure 3).
Photo 2. Bimanual direction.
Photo 3. Sheet calibrator.
Determined in this way, the central occlusion may or may not coincide with the position of maximum contact of the antagonist teeth. When planning treatment of a tooth in the area of which the first contact is observed, it is necessary to determine the presence or absence of a sliding effect. The author's preferred technique for determining the sliding effect is to have the patient clench the teeth together at the position of maximum intercuspidation, while the clinician determines whether the jaw moves significantly in any direction when reaching this position. Before determining the slide, the dentist must measure the level of vertical and sagittal overlap, for which a periodontal probe can be used. If the level of sagittal (horizontal) overlap is greater than the level of vertical overlap, considerable care must be taken during further treatment (Figure 4).
Photo 4. Determination of vertical and sagittal (horizontal) overlap.
For patients with sliding in central occlusion, changes in the vertical parameters of the overlap are more typical than in the horizontal ones. In this case, in most patients, sliding will be noted to the right, left, vertically, forward or backward. Sliding of more than 1.5-2 mm with a predominant horizontal component compared to the vertical component indicates a potential problem that may be associated with the “guide” tooth. The term "guide tooth" is used because its presence is the key to achieving arch relationship stability and is a significant determining factor in existing occlusal function. Restoration of this tooth can lead to unexpected changes in occlusion. The only way to understand the possible consequences of such interventions is to establish changes in the centric relation to determine what changes are noted in the occlusion after the occlusion in the region of the “guide” tooth has been changed. Due to the unique properties of physiology, once the patterns of (1) what partially held the occlusion, (2) the direction in which the patient was biting, and (3) what held the disc in place are forgotten, movement begins in a reverse loop: from teeth to muscles, from muscles to teeth. If the feedback chain is interrupted, it will no longer be possible to return the patient to his usual bite. Therefore, it is important to determine the possibility of developing such a problem before fixing the crown. No modifications should be made to the tooth structure until its full role in the occlusal process has been determined. If the teeth continue to maintain good contact after treatment and there is no change in centric relation, then there is nothing to worry about. But if new points of first contact are discovered that articulate “not quite well,” or there is a deficiency of occlusal space between the “guide” tooth and the antagonist, it is necessary to explain the possible consequences of such violations to the patient. At the same time, it is impossible to determine whether the restoration will provoke a problem that the patient cannot tolerate, or whether it will be within the limits of compensatory potential. But it is definitely necessary to warn the patient about the possible consequences.
Thorough diagnosis before starting treatment
Before the clinician begins the treatment process, it is necessary to conduct a complete diagnosis of the patient. The clinician must take the time to understand the specifics of occlusion, bite, muscle interactions, and the TMJ. Ideally, the doctor should identify all possible risk factors that may compromise the outcome of treatment in the future. The goal of diagnosis is to clearly categorize patients in whom treatment should not provoke significant changes from those in whom treatment may trigger the development of potential complications. A comprehensive diagnostic process begins with an analysis of the medical history, including the collection of data on the facts of prior injury, or the occurrence of pain symptoms. It is also necessary to familiarize yourself with the general somatic condition of the patient, confirm or exclude the presence of obstructive sleep apnea, snoring, gastroesophageal reflux disease, the fact of taking antiangiotic/antidepressant drugs, and the presence/absence of headaches. Patients with sleep apnea may not be aware that they have sleep apnea, so the Epworth score or similar diagnostic classification algorithms should be used to determine the likelihood of risk.
Modifying the degree of invasiveness of interventions
After collecting anamnesis, the doctor begins a thorough clinical diagnosis. The dentist should interview patients regarding his own attitude towards occlusion: for example, the patient may have signs of pathological abrasion, but he does not complain about a change in their shape. In this case, diagnosis should be carried out from the outside to the inside, starting from the assessment of less personal areas of the maxillofacial apparatus and moving towards more personal ones. In this case, it is necessary to diagnose all eight muscles of the study area, namely a pair of masticatory muscles (photo 5), a pair of temporal muscles (photo 6), a pair of medial and a pair of lateral pterygoid muscles (photo 7).
Photo 5. Chewing muscle.
Photo 6. Temporalis muscle.
Photo 7. Medial and lateral pterygoid muscles.
The causes of disorders in the TMJ area can also be the digastric muscle, the sternocleidomastoid muscle, the trapezius muscle and the splenius capitis muscle, however, it is not necessary to diagnose these in the absence of visible dysfunctions of the TMJ. The first step in the diagnosis is to palpate the masseter muscle with a pressure of about 3-5 pounds. In order to determine the strength of palpation, you can test it on a scale in a regular store. By palpating the entire length of the masticatory muscle, the doctor can easily determine in which area pain is observed. A similar palpation technique is used for the temporal muscles. Both pterygoid muscles are usually palpable intraorally, but this diagnostic process may be difficult for the lateral pterygoid muscle. A simpler method of assessment is to evaluate muscle activity while the dentist's hand is placed on the chin, after which he asks the patient to bring it forward, resisting pressure. After this, the doctor instructs the patient about the need to move the jaw to the left and right.
Joint condition and range of motion
It is also extremely important to collect information about the joint by assessing its range of motion and palpation data. To do this, the dentist places his finger on the side and then asks the patient to open and close his mouth. The patient should continue to do this movement until the doctor feels his finger move slightly to the right in front of the ear. After this, the doctor must apply some pressure to the joint area, determining the threshold of pain sensitivity. This technique can also be performed directly in the patient’s ear in the absence of any hearing aid disorders. After the doctor has already felt the specifics of the movement of the joint when opening and closing the mouth, the dentist can press his finger slightly down and forward, as if going behind the joint, assessing the patient’s pain reaction. If there is pain, the patient should rate it on a numerical scale. Range of motion can be measured using a ruler, a triangle, or any other tool designed specifically to vary distances. The range of motion should be determined with the mouth open and closed, taking into account the parameters of the vertical overlap. In addition, the range of motion of the jaw to the left and right must be assessed.
Load test and joint response
After diagnosing the muscles and joint, they begin to analyze occlusion, centric relation and central occlusion. A stress test is used to check the condition of the joint. This test is performed by placing an object in the mouth, similar to a leaf calibrator, after which the patient moves the jaw back and forth and then bites. If during the diagnosis it is painful for the patient to move the jaw forward, then the problem is not in the load, but in the muscles and tissues behind the articular disc. After the patient moves the jaw back and bites, the presence or absence of pain allows the doctor to assess the degree of disc displacement. The dentist can conclude whether the patient has only lateral displacement, or whether there is also medial displacement, which is much more difficult to treat. The clinician then moves from the stress test to an examination of the oral cavity itself. The presence of signs of wear, vibration and tooth fracture are signs that may indicate problems with occlusion. To evaluate the analysis of their etiology, it is important to analyze the specifics of articulatory excursions and interaction of teeth in the distal area. To perform this procedure, articulating paper of two different colors can be used. First, the doctor uses very thin paper and instructs the patient to move his jaw left and right, forward and back, chew the paper, and then move his jaw in any direction he can. At this stage, if there are violations, most patients already show signs of clenching or bruxism. After the patient has “chewed” the previous piece of paper, he should bite in the maximum fissure-tubercle ratio, using articulating paper of a darker color. Thus, by analyzing the light markings on the teeth, the doctor can assess the interference with articulatory movement, and the darker markings can assess the contact in a state of maximum intercuspidation. But such an approach does not help the doctor determine existing TMJ pathologies. On the other hand, the results obtained can be used in planning restoration treatment and prognosis of the functional state of the periodontium. An alternative to the above technique is the use of new T-scan technology.
Methods for studying the condition of the articular disc
The gold standard for examining the disc is magnetic resonance imaging (MRI), which can visualize various positions of the structural element of the joint. But given that MRI is not a routine diagnostic method, in clinical practice a doctor may use the “open, look, listen and feel” test. The clinician should listen for sounds as the patient opens and closes the mouth while performing food and light palpation of the joint. At the same time, the doctor must also monitor possible deviations and displacements. Deviations are observed when the disc moves to the side and then re-centers, that is, it deviates to the left or right, but the final position is still marked in the middle. Displacements are characterized by the movement of the disk to one side or the other, while it remains at this angle. Additionally, you can listen to the joint with a stethoscope, this way you can study the disc popping out of the joint. After comparing the obtained data with preliminary data recorded during the stress test and related manipulations, the doctor can make a working diagnosis. In some cases, the Doppler method may be used. It allows you to broadcast audio sounds during joint movement, so that not only the doctor, but also the patient can hear. The disadvantage of this method is the need to use a lubricating gel, the sensation of which is unpleasant for some patients. Joint vibration analysis (JVA) can also be used. The JVA is a complex measuring device containing a small microphone attached to earphones that pass through the joint area. This device records frequency and cataloged joint noises, but its disadvantage is its excessively high price. Adequate diagnosis of chronic or acute disc displacement disorders will ensure the prevention of complications in the future, leveling the risk of failure of clinical measures.
Making a diagnosis based on joint disorders
Classification of changes in the joint area can be carried out according to the system proposed by Mark Piper. This approach involves categorizing the disorder into 5 main stages. Stage I – normal condition of the joint. Stage II is a loose condition of the ligament (ligament laxity). The ligament is like a rubber band: it can stretch and become doughy, causing noise when moved. Stage III usually involves lateral displacement of the disc. The reason for this may be a traumatic effect on the joint area, but often the presence of pain is not a sign of the bone form of the disorder. Stage IV disc involves medial disc displacement (acute or chronic). Stage V develops when there is a change in the disc anatomy in the area behind the underlying tissue (early/acute or chronic perforation). Using this classification requires a deep understanding of the joint.
Devices for the treatment of muscle pain
The success of treating patients with muscle pain may depend on the choice of the appropriate device. The choice of the latter depends on the etiology of the disorders. If the patient shows signs of pathological abrasion, there are ceramic restorations in the oral cavity, and no disorders are registered from the point of view of the joint, then the goal of treatment is to protect the teeth from pathological abrasion. A night guard can be used for this purpose. Similar designs of mouth guards can be used in the treatment of muscle pain, but in this case they are called splints or splints, or other types of mouth guards. The splint is designed to change the position of the jaw in any direction and correct the vector of acting forces to eliminate the symptoms of muscle pain.
Full overlap tires
If the disc is displaced and there is pain, the patient needs a mouthguard that takes into account the etiology of the disorder. Full-coverage mouth guards are used to routinely protect teeth from abrasion. It can also be used to assess the complexity of the pathology of bruxism or clenching. A mouthguard of this design can be made directly in the dental chair, but its range of use is limited. The use of separate modifications to these aligners should even be avoided in the presence of disc displacement. A rigid, full-coverage splint performs the same function (protecting the teeth) but also provides the stable joint position that is intended by the design. By stabilizing the joint, muscle relaxation is achieved, which provides opportunities for determining the centric relation. If you have muscle pain without disc displacement and difficulty determining the centric relation, a rigid full-coverage splint is a good choice for treatment. Such splints also help to minimize or avoid ligament deformation. At the same time, both the patient and the doctor must understand that there is no universal mouth guard design for all occasions. There are many types of full-coverage rigid mouthguards. For example, the Pankey/Dawson splint is a flat mandibular appliance with no angles that does not cause posterior displacement of the disc or joint. The maxillary anterior orthopedic (Michigan) splint is a solid acrylic splint that covers the maxillary teeth, with a ramp over the structure. The theory behind its use is to eliminate the distal teeth from the insertion route. The Tanner mouthguard allows you to slightly separate the jaws while maintaining the position of the disc and joint, thus achieving muscle relaxation, which can significantly determine the presence or absence of joint pathology.
Hybrid devices
Hybrid devices are distinguished by their ability to multitask. The most common is the anterior bite plane, which is quite easy to create. When the anterior bite plane is combined with the lingual ramp behind the teeth, the appliance can be classified as a Farrar appliance. The latter is used in the treatment of patients with obstructive sleep apnea. The Farrar appliance does not provoke distalization of the joint, maintaining the vertical parameters of the bite, but at the same time does not allow the lower jaw to slide back, holding it with the lingual ramp. The use of the distal Gelb apparatus allows the formation of only distal occlusion. But it is not recommended to use it for more than 12 hours a day or for more than 3 months, since the formation of an anterior bite can lead to the development of pathological abrasion. The use of the Hawley apparatus with front stop markers was first proposed by Kois. The advantage of the Kois splint is that it can be used to equilibrate the occlusion during restorative treatment. In addition, this mouth guard can also be used as a guide. As the splint is continually bitten, the clinician can identify distal stopping areas and inferior biting areas around which appropriate modifications need to be made. The difficult part of the jaw equilibration process is that during its implementation it is possible to reduce the vertical bite parameter, also provoking changes in the joint. The nociceptive trigeminal inhibitory splint (NTI) is essentially an anterior bite plane, but smaller, which also expands its range of application. It is important to remember that hybrid devices cannot be worn 24 hours a day. Especially distal supported appliances, which provoke changes in the bite that could easily be corrected through orthopedic or orthodontic treatment. If the likelihood of a change in the bite is high, the dentist should discuss this with the patient in advance, informing him of the possible results of treatment. At the same time, it must be remembered that the goal of all hybrid devices is to free the patient from pain.
Critical stages of using mouth guards
When making a diagnosis and choosing a treatment method, choosing the appropriate mouth guard should not be problematic. Before fixation, the doctor must be aware that he has all the necessary tools: burs, rubber bands, polishing systems, and, of course, knowledge. When bonding the trays, the process begins with drying the teeth before marking them. For this purpose, a layer of fabric can be placed on the articulating paper clamps. After that, they begin to use first the red articulation strip, and then the blue one. Red is mainly used to analyze lateral displacements, and blue is used to analyze changes in the vertical direction. After this, the necessary modifications are carried out using boron.
When bite is not a problem
Every year, the dental community pays more and more attention to the problem of bruxism during sleep. In 2005, the American Academy of Sleep Medicine (AASM) defined sleep bruxism as a sleep-related movement disorder similar to restless leg syndrome or parafunctional dentofacial activity. This is usually associated with waking up during sleep. As of 2014, the understanding of sleep bruxism has changed somewhat. The AASM now defines this disorder as “repetitive jaw muscle activity characterized by clenching or grinding of the teeth and/or changes in the position of the mandible.” In a 2014 study, Hosoya et al found a correlation between obstructive sleep apnea and a high risk of developing sleep bruxism. Therefore, patients should be screened for risk factors associated with sleep bruxism. If this pathology is suspected, the patient should be examined by an appropriate doctor, who can provide individual consultation and an appropriate diagnosis. Patients diagnosed with sleep bruxism are characterized by the presence of dental hypersensitivity, the presence of bites in the tongue and cheeks, a burning sensation in the masticatory muscles and noises, and a blocking function of the TMJ. Sleep apnea is also commonly associated with fatigue and snoring. Factors indicating the presence of sleep apnea and associated bruxism should be identified during the history taking or during the preliminary diagnostic stage.
conclusions
Effective application of diagnostic methods and differential diagnosis of occlusal changes involves early identification of occlusal pathologies by assessing the state of intermaxillary relationships, TMJ function and pain sensations associated with disorders. A thorough understanding of the concepts of guide tooth, muscle fixation, and sleep bruxism is also part of the clinician's overall knowledge required to conduct an adequate diagnostic process. During the diagnosis, the doctor analyzes the centric relation and central occlusion, the condition of the masticatory muscles, their range of motion and the level of joint displacement. This information is based on a comprehensive preliminary diagnosis, using not only clinical techniques, but also additional instrumental methods. Diagnosis of the patient should be carried out “from the outside in”, always starting with palpation of the masticatory, temporal, medial and lateral pterygoid muscles. A stress test allows the clinician to determine whether loading a joint is causing pain, and a classification system is used to categorize the results of diagnosing a slipped disc. Treatment of slipped discs and muscle pain depends on the choice of mouth guards in a variety of designs, from rigid analogues to hybrid designs. Ultimately, it is critical to identify the difference between problems caused by malocclusion and those caused by sleep bruxism. The combination of all these factors is crucial for the successful restoration of a functionally stable occlusion in the general practice of a dentist.
Posted by Scott Cairns, DDS
Calculations for orthopedic purposes
In the process of creating prosthetic structures for malocclusion, an orthopedic specialist takes measurements of the heights of the lower third of the patient’s face using an anatomical and physiological method.
To do this, the height of the bite is measured in a state of complete reduction of the jaws, with central occlusion and in a state of physiological rest.
Payment procedure:
- At the lowest point of the nose , at the level of the nasal septum, the first mark is placed strictly in the center. In some cases, the specialist places a mark on the tip of the patient's nose.
- in the center of the chin , in its lower zone.
- Between the applied marks, the height is measured in the state of central occlusion of the jaws. To do this, bases with bite ridges are placed in the patient’s oral cavity.
- Repeated measurements are taken between marks , but in a state of physiological rest of the lower jaw. To do this, the specialist must distract the patient so that he really relaxes. In some cases, the patient is offered a glass of water. After a few sips, the muscles of the lower jaw really relax.
- The results are recorded. However, the standardized indicator of normal bite height, which is 2-3 mm, is subtracted from the height at rest. And if after this the indicators are equal, we can talk about normal bite height.
If, when measuring height, the calculation results yield a negative result, the lower third of the patient’s face is underestimated . Accordingly, if the result deviates in a positive direction, the bite is overestimated .
What is the significance of teleradiography in orthodontics, and what is revealed with its help.
In this publication we will talk about diagnostic methods in orthodontics.
Here https://orto-info.ru/ortodonticheskoe-lechenie/podgotovitelnyiy-period/miogimnastika.html you are offered myogymnastics exercises used in orthodontics.
Techniques for correct positioning of the lower jaw
Correct positioning of the patient's jaw in the position of central occlusion involves the use of two methods of placement: functional and instrumental.
The main condition for correct placement is muscle relaxation of the jaw muscles.
Functional
The procedure for carrying out this method is as follows:
- the patient moves his head back slightly until the neck muscles tense, which prevents protrusion of the jaw;
- touches the tongue to the back of the palate, as close to the throat as possible;
- at this time, the specialist places his index fingers on the patient’s teeth, lightly pressing on them and at the same time slightly moving the corners of the mouth in different directions;
- the patient imitates swallowing food, which in almost 100% of cases leads to muscle relaxation and prevents jaw protrusion;
- When bringing the jaws together, the specialist touches the surfaces of the teeth and holds the corners of the mouth until it is completely closed.
In some cases, the procedure is repeated several times until complete muscle relaxation and correct reduction of both rows are achieved.
Instrumental
It is performed using specialized devices that copy jaw movements. It is used only in extremely serious situations, when bite deviations are significant and it is necessary to correct the position of the jaw using the physical efforts of a specialist.
Most often, when carrying out this method, the Larin apparatus and special orthopedic rulers are used, which make it possible to record jaw movements in several planes.
Stages of testing the prosthesis design
After the technician has installed the artificial teeth (this was in the last article), he gives me the wax bases. Mandatory with teeth on the models and in the articulator. I, in turn, must make sure of the quality of the work. It’s just that now that the bases of the prosthesis are made of wax, any mistake will be easy to correct.
My train of thought:
1) First I evaluate working models. They should not have pores, damage or chips. Any inaccuracy on the model will make the prosthesis unbearable. So if I don't like the model, I take a functional impression again. Of course, this is difficult and unpleasant. But it will be much more unpleasant to remake a finished prosthesis.
2) The model must have markings, a midsagittal line, etc. (we talked about them in the previous article). Some anatomical features of the patient should be isolated (tori, bony protrusions, incisive papilla if it is hypertrophied). Then the base will not touch them and injure them.
3) Then I estimate the boundaries of the bases:
Firstly: they should be as thick as the edge of a functional print.
Secondly: they must fit snugly to the model throughout.
Thirdly: they must end exactly along the border of the future prosthesis
(On the upper jaw: 1-2 mm above the transitional fold, bypassing the frenulum of the upper lip and buccal cords. Distally, 1-2 mm overlaps the blind fossae (the place where the hard palate transitions to the soft palate).
On the lower jaw: 1-2 mm below the transitional fold, bypasses the frenulum of the lower lip and buccal cords and completely covers the mucous tubercle in the retromolar region. On the tongue side, the border passes through the junction of the gums and the mucous membrane of the floor of the oral cavity.)
4) I check to see if the bases are balanced.
Balancing a prosthesis is an uneven fit of the base to the prosthetic bed. The prosthesis seems to swing on the jaw.
5) I evaluate the setting of the teeth. Do they correspond to anatomical landmarks? I check whether the shape of the dentition is correct. Are there compensatory curves (Spee, Wilson). Is uniform occlusion created?
6) After a thorough check in the articulator, I remove the dentures from the models and disinfect them. After that, I put them on the patient’s jaws and test them, so to speak, in vivo.
7) First, I examine the patient’s face: is the height of the face restored, are the lips and cheeks sunken. How are the nasolabial and chin folds expressed, are the corners of the mouth drooping, and are the muscles tense?
 Then I look into the patient's mouth. I check the position of the borders of the base and make sure that they fit tightly to the mucosa. I check again to see if the prosthesis is balanced.
Then I look into the patient's mouth. I check the position of the borders of the base and make sure that they fit tightly to the mucosa. I check again to see if the prosthesis is balanced.
9) I evaluate the position of the occlusal plane. It should be parallel to the pupillary line in the anterior region and the Camper line in the area of the chewing teeth.
10) I look to see if the midline of the face coincides with the line between the central incisors, and whether each tooth has two antagonists.
11) I check if balanced occlusion is created. Those. is the same number of teeth in contact on the left and right half of the jaw for any type of occlusion (lateral, anterior).
12) I check the height of the lower part of the face. Normally, it is 2-4 mm less than the resting height. I measure the distance between two points at rest and at the position of central occlusion.
12.1) I can also use a speech test. When pronouncing the sound [v, f], the upper incisors evenly touch the lower lip. They touch it exactly along the line of transition between the lip of the face and the lip of the vestibule of the mouth (dry to wet).
If the teeth are spaced and matched correctly, the patient will not have problems pronouncing these sounds.
13) And the last thing I check is aesthetics. The upper central incisors protrude from under the lip by 1-2 mm. When smiling, the lip rises to the level of the necks of the teeth. The gums are not visible.
14) I give the patient a mirror so that he can evaluate the prosthesis himself. Only after his approval do I give the prosthesis to the technician. He exchanges wax for plastic and prepares the prosthesis for delivery.
That is if everything went well. But there may be mistakes. I'll tell you about them now.
Errors allowed
Creating a prosthetic structure in conditions of malocclusion is a most complex orthopedic procedure, the quality of which depends 100% on the qualifications of the specialist and a responsible approach to work.
Violations in determining the position of central occlusion can lead to the following problems:
The bite is too high
- The folds of the face are smoothed, the relief of the nasolabial zone is poorly defined;
- the patient's face looks surprised;
- the patient feels tension when closing the mouth, while closing the lips;
- the patient feels that during communication the teeth are knocking against each other.
Low bite
- The folds of the face are strongly pronounced, especially in the chin area;
- the lower third of the face visually becomes smaller;
- the patient becomes like an elderly person;
- the corners of the mouth are lowered;
- lips sink;
- uncontrolled salivation.
Permanent anterior occlusion
- There is a noticeable gap between the front incisors;
- the lateral elements do not contact normally, tubercle reduction does not occur.
Permanent lateral occlusion
- Overbite;
- clearance on the offset side;
- shifting the bottom row to the side.
Reasons for such problems
- Incorrect preparation of wax templates.
- Insufficient softening of the material for taking impressions and impressions.
- Violation of the integrity of wax forms due to their premature removal from the oral cavity.
- Excessive jaw pressure on the ridges during impression taking.
- Errors and violations on the part of the specialist.
- Errors in the work of the technician.
The video provides additional information on the topic of the article.
Causes and types
Reasons that have a negative impact on the intermaxillary distance:
- greater abrasion of teeth, due to which the strength of hard tooth tissue is lost;
- functional overload of individual teeth, which can be caused by improper bridge prosthetics;
- disorders of the nervous system that are accompanied by grinding of teeth;
- with a fight in the gastrointestinal tract;
- disturbance of phosphorus-potassium metabolic processes.
There are high and low pathological bites. The reason for the overestimation may be an incorrectly made denture, when the implant turns out to be slightly higher than the rest of the teeth.
Low bite, as a rule, is diagnosed when the hard tissues of the tooth are severely abraded, and in rare cases, when the prosthesis is installed incorrectly.