484
Age-related degradation of the dental pulp is manifested by many negative processes - deterioration of blood circulation in the neurovascular bundle, decreased activity of dentin-forming cells, fibrosis, reduction in size and change in the shape of the pulp chamber, calcification, etc.
The formation of denticles in the tooth pulp is also considered one of the age-related degenerative manifestations. However, aging is not the only reason for the appearance of calcium nodules in the pulp.
General information
Denticles are calcifications formed in the pulp in the form of irregularly shaped nodules measuring up to 2-3 mm. Denticles have many other names - dentinoids, internal odontomas, pulp stones, “teeth”, endoliths, etc.
Although the cause of their formation is most often age-related pulp degeneration (denticles are observed in 90% of older people), they can appear in the teeth of young and mature people for various reasons.
According to statistics, 40-55% of patients in dental clinics have denticles in their teeth. They are also found in children and adolescents, although much less frequently - in only 5%.
Denticles consist of dentin or dentin-like tissue, that is, calcium salts, mainly hydroxyapatite. Most of them (up to 70%) are formed in the root pulp. They can be free in the tooth cavities (surrounded on all sides by pulp), or immured in their walls.
The denticles themselves do not have a source of pain (they lack pain receptors). However, being in the pulp, they can put pressure on its nerves, thereby giving rise to pain.
True, this does not happen very often. Most people do not experience pain when denticles form. And they don’t even suspect that there are “stones” in their pulp.
According to the international classification of diseases, denticles and other forms of calcification are designated by code K04.2.
Petrificates
The internal structure of denticles is layered. In the center is a harder core of amorphous mineral salts called petrificates. Around which calcium-lime layers gradually build up over time.
Petrifications form around necrosis or any destruction in the pulp tissue in the very first stages of the disease. That is, the form of pulpitis: acute diffuse, purulent, chronic fibrous, gangrenous, concremental or another - is formed precisely at the first stage of the inflammatory process in the pulp. Sometimes a cold or an exacerbation of a rheumatic form of joint disease is enough for the process to follow the concremental scenario.
Painful sensations are a consequence of compression of the neurovascular bundle of the pulp by denticles. Due to the discrete structure of the denticles that cause this form of pulpitis, the pain from them is not constant. And it is easily localized according to the patient’s own sensations. He can easily indicate which tooth hurts.
Causes of appearance and mechanism of development
The exact mechanism of denticles formation is not completely clear. But it has been established that the root cause of their appearance can be considered a metabolic disorder, leading to calcification in the tooth pulp.
In turn, metabolic disorders can occur with various pathologies of both the dentofacial apparatus and the body as a whole.
It is believed that the following diseases and factors can directly lead to the formation of denticles:
- age-related pulp degeneration;
- caries;
- periodontitis and other periodontal diseases, including inflammatory ones;
- concremental pulpitis;
- endocrine diseases;
- preparation of dental tissues;
- disruption of the activity of odontoblasts - cells responsible for the formation of dentin;
- injuries to temporary and permanent teeth - fractures and dislocations of roots, etc.;
- hypo- or hypervitaminosis (in particular, lack of vitamins A and C or excess vitamin D);
- long-term use of hormones;
- hereditary dental diseases (dentinogenesis imperfecta, etc.).
Even therapeutic, endodontic and orthodontic dental treatment can provoke the formation of denticles. In particular, dentin burns during the passage of canals or therapeutic pads with their high pH.
Development factors
Despite numerous studies devoted to this issue, a final answer to the question of the reasons for the development of denticles has not yet been received. Experts note a number of characteristic factors, the combination of which leads to the formation of a pathological condition:
- Mechanical damage to dental elements;
- Removal of necrotic crown tissues during treatment;
- Long-term use of orthodontic devices;
- Disorders of the functioning of important body systems;
- Long-term use of hormonal drugs;
- Development of inflammatory and degenerative processes in the periodontal structure;
- Age-related changes, such as abrasion of the enamel layer and dentin;
- Hereditary factors, including abnormal dentin development.
Classification
Denticles are classified according to several parameters.
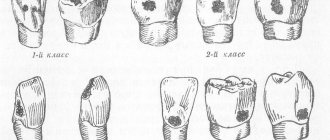
By location:
- to free (surrounded by pulp on all sides);
- parietal or adhesive (in contact with the walls of the pulp cavity);
- interstitial (embedded, built-in) - surrounded on all sides by dentin.
By number:
- single;
- multiple, merging with each other into conglomerates (can become so large that they completely block the root canals).
A very important division in composition and structure:
- True or highly organized. They are formed by preodontoblasts, which work like odontoblasts. They represent heterotopic dentin. They contain dentinal tubules, that is, they are similar in structure to the dentin of teeth. This is a relatively rare type.
- False or poorly organized. They consist of a calcified substance that forms around necrotic areas of the pulp. They do not contain dentinal tubules and are much more common than true ones.
A feature of false denticles is the concentric arrangement of calcified substance around necrotic cells, collagen fibers, and blood clots.
Features of the drug Nanofluor - a varnish for deep fluoridation of dentin and enamel.
Come here to see how diagnostics in dentistry have advanced with the advent of intraoral cameras.
At this address we will tell you how to properly treat acid necrosis of hard dental tissues.
Manifestations and features of the course of the disease
Most often, denticles do not cause pain. Pain occurs when they interfere with blood flow and compress pain receptors located in the pulp.
The presence of denticles may be indicated by the moment pain appears. Pain may occur in the following cases:
- Under the influence of temperature and chemical irritants (overheating of the tooth during preparation, amalgam fillings installed without a gasket).
- When there is a sudden change in body position (when climbing in an airplane, playing sports, etc.).
- With climate change (pain may increase in cold weather).
- With concrementous pulpitis.
- Under the influence of other provoking factors.
The nature of dental pain resembles the symptoms of acute pulpitis. The difference is that dental pain occurs sporadically, due to the provoking factors listed above.
Pain in acute pulpitis is usually long-lasting.
Discomfort can also manifest itself as a feeling of pressure in the causative tooth while eating.
What can happen if pulpitis is not treated?
Since in some cases the disease occurs without pain, many people put off going to the dentist until the last minute. Do not forget that while you are inactive, the disease progresses. Refusal to treat pulpitis can cause serious complications:
- Flux
- periostitis, a pathological inflammatory process developing from the periosteum.
- Periodontitis
- inflammation of the tissue around the root of the tooth with the possible formation of purulent pockets and destruction of the periapical bone tissue.
- Pulp gangrene
(necrosis) is the death of cells in the internal tissue of the tooth.
- Sepsis
- blood poisoning that develops when microorganisms enter the general bloodstream (usually occurs with reduced immunity).
To avoid such dangerous complications, you need to visit the dentist once every six months. Patients at risk should be examined more frequently (once every three months). The risk group includes patients with diabetes, oncology and other diseases that reduce immunity. If you notice symptoms of caries, go to the doctor immediately.
Diagnostic measures
The main way to diagnose denticles is radiography. On an x-ray, single or multiple nodules with a characteristic dense structure are visible in the tooth cavities.
True, in order to see them, the denticles must be large. Small ones are most often discovered during tooth extraction or routine treatment.
If they are large in size, the denticles can cover and mask the root canals on the radiograph.
Since pain from denticles resembles the pain that occurs with pulpitis, the first misdiagnosis may be acute pulpitis or an exacerbation of chronic pulpitis.
The difference between denticles and pulpitis is that in the first case the patient can accurately indicate which tooth hurts, and in the second, due to the fact that the pain sensation, radiating along the trigeminal nerve, spreads to neighboring teeth, it is difficult for him to do this.
Sometimes denticles cause the sensation of a foreign object under the causative tooth. Their presence can indirectly be indicated by the absence of fissures and/or increased abrasion of the occlusal surface.
When hypothermia occurs, patients may experience a feeling of heaviness in their teeth and discomfort while eating.
To diagnose, the doctor can use the Novik test , which consists of sharply lowering the chair, causing pain in the patient.
Diagnosis is complicated if denticles are accompanied by pulpitis. In this case, the following pain sensations are characteristic:
- intensifying along the trigeminal nerve, “not letting go” for a long time;
- increasing at night;
- appearing when chewing solid food;
- starting suddenly with a sharp pain that gradually subsides.
Pulpitis with denticles also manifests itself through intense salivation and lacrimation.
“Fluid” symptoms
Making a diagnosis is difficult because its manifestations are extremely similar to trigeminal neuralgia. In which the main node is located in the temporal lobe near the top of the ear. And it spreads with one branch in the undereye, the second to the nose, and the third - under the cut of the lower jaw, just where the roots of the teeth are. And the picture of pain is extremely similar to dental pain. Only the rarity of the disease (1 case in 15,000) suggests trigeminal neuralgia as a last resort.
Most often, the first diagnosis will still be an exacerbation of chronic pulpitis. But knowing the results of statistics, the doctor always keeps in mind the possibility of pulpitis occurring in a concremental form. The overall percentage of cases of this form reaches 39-54% in older people (over 40) and approximately 5% in children under 16 years of age. The numbers are not comparable to cases of inflammation of the trigeminal nerve.
Clinical picture
Most often, the clinical picture of the development of the disease looks like this:
- Gradual increase in pain along the location of all three branches of the trigeminal nerve.
- Long lasting pain.
- An increase in pain at night, despite the fact that the pain does not seem to be provoked by anything (they did not eat cold or hot, sour or sweet).
- Increasing pain after chewing solid food.
- Unprovoked surges of pain with a slow decrease.
- Manifestations of lacrimation and strong salivation.
- A feeling of heaviness and a foreign object in the gum under the sore tooth.
It is difficult to diagnose this form of pulpitis, no matter what stage of development of the process it is at. The presence of such a disease is revealed as a result of a survey, a history study, or after an X-ray examination of the oral cavity.
X-rays could have been taken for a completely different reason (root removal, prosthetics, etc.). Although most often the patient comes to the doctor as a result of the fact that he is tired of constant pain.
Treatment tactics
Teeth with painless denticles do not lose their functionality and aesthetics. Therefore, if dentinoids do not cause pain or other discomfort, and also do not have a tendency to overgrow, treatment is not carried out.
If they are accompanied by pain and/or interfere with endodontic treatment for other indications, they are removed using a drill (if located in the coronal chamber) or an ultrasonic scaler (if localized in the root canals).
Removal using the example of treatment of concremental pulpitis consists of the following steps:
- local anesthesia;
- preparation of the pulp coronal chamber with a bur;
- removal of calcified contents from root canals with an ultrasonic scaler;
- cleaning and antiseptic treatment of the cleaned cavity;
- obstruction of the canal;
- filling of the coronal cavity.
If the denticles cannot be removed for some reason, electrophoresis with potassium iodide or depophoresis with copper and calcium hydroxide can be performed.
The procedure is accompanied by the disintegration (proteolysis) of the remains of biological tissues, the destruction of pathogenic microorganisms, the formation of a film of calcium and copper hydroxide in the canals and microtubules of the roots.
As a result, long-term sterilization of tooth tissues and activation of the formation of new dentin in root cavities is ensured.
However, you should know that electrophoresis and depophoresis are advisable to use only if the tooth has already been subjected to devital endodontic treatment.
In general, the prognosis is considered favorable, and patients should not have any particular concerns about them.
A new concept in minimally invasive endodontics is the SAF system (self-adaptive file).
In this publication we will talk about the reasons for the formation of dentinogenesis imperfecta.
Here is all the most important information about hypercementosis.
Preventive actions
To date, no special measures have been developed to prevent the formation of pulp stones. And this is understandable - the etiological factors are too numerous and uncertain.
For timely diagnosis and treatment, we can only recommend regular visits to the dentist with dental x-rays, emergency treatment of all diagnosed diseases, high-quality oral hygiene, and giving up bad habits that adversely affect the condition of the teeth.
The video provides additional information on the topic of the article.
Reviews
Considering that denticles most often appear as a factor accompanying aging, it can be assumed that most people will never know that they had denticles in their teeth.
If you personally have experience getting rid of dentinoids, share it with us. How were they discovered, what treatment was given, was it successful? The comment form is at the bottom of the page.
If you find an error, please select a piece of text and press Ctrl+Enter.
Tags toothache
Did you like the article? stay tuned
No comments yet
What might you encounter after treatment?
Some patients report discomfort after filling. It is important to distinguish whether this pain is correct (post-filling) or one that requires immediate consultation with a doctor.
Mild pain is almost normal after pulpitis treatment. This is due to the fact that a serious intervention was performed, especially if inflammatory and pathological processes had previously occurred. Temporary pain occurs during the first couple of days and occurs when chewing. There is no need to go to the dentist, wait a while, the pain will go away.
The pain is sharp, intensifying and occurring throughout the week may indicate the continuation of the inflammatory process. Swelling of the gums indicates the same thing. In this case, you need to visit your dentist.