Already a few months after birth, the baby's first teeth begin to appear. They are temporary and by the time the molars are fully formed, they will fall out, making way for permanent teeth. This whole process takes quite a long time and may be accompanied by complications. In order not to encounter difficulties during the period of changing baby teeth to permanent ones, dentists recommend visiting a specialist from the moment the first teeth appear. The Martinka Clinic employs highly qualified doctors who will help maintain the health of baby teeth and prevent pathologies of permanent teeth.
How do you replace baby teeth with molars?
To the surprise of many parents, children are born with already formed rudiments of not only milk teeth, but also molars. If the first temporary teeth erupt already from 3–6 months, then the internal development of permanent teeth begins only at 12 months.
By the age of 3, most children have already formed a full set of teeth. Until 5–6 years, all teeth will remain in place, and then their replacement will begin, which will last about 6–7 years. Moreover, if a small child has 20 teeth in the oral cavity, then a teenager 13–15 years old already has 32.
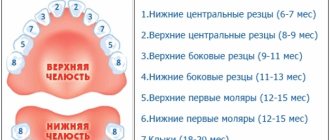
Scheme of the age of eruption of molars in children:
- 5–7 years – lower central incisors;
- 6–7 years – central upper and lateral incisors;
- 7–9 years – lateral incisors on the upper jaw;
- 9–12 years - replacement of premolars and canines;
- after 12 years - replacement of molars and growth of teeth that do not have temporary replacements.
The indicated periods are statistical averages. Molars may begin to erupt earlier or, conversely, later. This process is individual and even non-compliance with the order of loss of baby teeth cannot be ruled out.
Mostly, by the age of 14, the child has already formed the entire dentition. Even the eruption of wisdom teeth is not excluded, although more often the eighth molars erupt after 20 years.
DEVELOPMENT AND STRUCTURE OF TEETH
There are 32 permanent teeth (dens permanens) in the oral cavity of an adult. In each half of the jaw (right or left) there are 2 incisors (dens incisius), 1 canine (dens caninus), 2 premolars, or small molars (dens praemolaris), and 3 molars, or large molars (dens molaris). The 3rd large molar is called the wisdom tooth (dens sapientiae).
In the oral cavity of a 6-7 year old child there are 20 primary teeth (dens deciduus). Each half of the jaw has 2 incisors, 1 canine and 2 large molars.
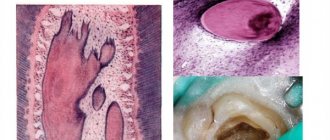
The tooth consists of a crown (corona dentis), rising above the gum; neck (cervix dentis), covered with gum; root (radix dentis), located in the alveolar process of the jaw.
The tooth includes hard and soft tissues. Hard tissues include enamel (enamelum), dentin (dentinum) and cement (cementum), while soft tissues include pulp (pulpa dentis).
The tooth is held in the socket of the alveolar process of the jaw with the help of a supporting (ligamentous) apparatus, including cement, periodontium and the wall of the socket. Some scientists (L.M. Tsepov) do not classify cement as a supporting apparatus of the tooth.
The development of teeth (odontogenesis) undergoes 3 stages: 1) the formation of the dental plate and the formation of tooth germs; 2) differentiation of tooth germs; 3) histogenesis.
1st stage
begins at the 6-7th week of embryogenesis with the formation of the vestibular plate. This plate is formed as a result of the ingrowth of epithelium into mesenchyme along the edge of the oral cavity. Then the vestibular plate splits into 2 layers, resulting in the formation of the vestibule of the oral cavity (vestibulum oris).
After this, a second strand of epithelium grows inward from the vestibular cavity. This is the dental plate (2 plates - upper and lower). From the inner surface of each plate, 10 epithelial outgrowths are formed - dental buds (gemma dentis). Mesenchyme grows into the dental buds - the dental papilla (papilla dentis). As the dental papilla grows from the dental bud, an epithelial dental organ (organum dentale epitheliale), or enamel organ, is formed. This organ has the shape of a double-walled bowl. The mesenchyme thickens around the enamel organ. This seal is called the dental sac (sacculus dentis).
As a result of the 1st stage of tooth development, a tooth germ is formed. It consists of 3 components: the dental organ, the dental papilla and the dental sac.
2nd stage
begins with the differentiation of the components of the tooth germ.
The differentiation of the dental organ (enamel organ) is characterized by the appearance of 3 layers.
The 1st layer is the internal epithelium (epithelium dentale internum), adjacent to the dental papilla. Its cells acquire a prismatic shape and are called enameloblastus, since enamel will then develop from them;
The 2nd layer is the outer epithelium (epithelium dentale externum), adjacent to the dental sac. Its cells have a flattened shape; after teething, they are partially reduced and partially fuse with the gingival epithelium;
The 3rd layer is the intermediate layer of the dental organ, located between the outer and inner layers. Its cells acquire a stellate shape as a result of the accumulation of fluid between them. This layer is called the pulp of the dental organ (pulpa organi dentis), from which the cuticle of the tooth is later formed.
The dental organ is connected to the dental plate using a neck. At the 3rd month of embryogenesis, the dental organ separates from the dental plate.
The differentiation of the dental papilla is that it increases in size and protrudes deeper into the dental organ. Blood vessels and nerve fibers grow into the dental papilla. On its surface, mesenchymal cells differentiate into preodontoblasts, or predentinoblasts. Dentin will later develop from these. Mesenchymocytes of the central part of the dental papilla differentiate into connective tissue cells of the future dental pulp.
The differentiation of the dental sac is manifested in the fact that it is divided into 2 layers: 1) internal and 2) external. Later, cementum will develop from the inner layer, and periodontium will develop from the outer layer.
Stage 3 (histogenesis)
includes:
1) dentinogenesis, or dentin development (dentinogenesis);
2) pulp development;
3) enamelogenesis, or development of enamel (enamelogenesis);
4) development of cementum and periodontium.
Dentinogenesis
begins in the 4th month of embryogenesis. Predentinoblasts of the dental papilla differentiate into dentinoblasts (dentinoblastus). Dentinoblasts have an elongated shape, contain an oval or round nucleus, the cytoplasm contains the Golgi complex, granular ER, mitochondria and the ALP enzyme. Processes extend from dentinoblasts. The process facing the dental papilla is called central.
Dentinoblasts produce collagen molecules, from which collagen fibers are polymerized, and the cementing substance predentin (glycoproteins, phosphoproteins, proteoglycans and phosphorins). Initially, collagen fibers have a radial direction. This is mantle predentin. When the thickness of predentin reaches 40-80 microns, collagen fibers acquire a tangential (longitudinal) direction, and pulpal predentin is formed.
As dentinoblasts deposit predentin substance, they move further and further from the surface to the center, but the ends of their peripheral processes remain in place, and the processes themselves lengthen. Predentin forms around the processes. Thus, the processes end up in the tubules, which are called dentinal. The resulting predentin, composed of organic matter, is a soft substance that can be cut with a knife. In order for predentin to become a solid substance - dentin, it is necessary to deposit salts in it (mineralization).
Mineralization
predentin is carried out in the 5th month of embryogenesis with the participation of alkaline phosphatase, under the influence of which glycerophosphate in the blood is broken down into phosphoric acid and monosaccharides. Phosphoric acid combines with calcium to form calcium phosphate, which is deposited in predentin to form dentin.
During the mineralization of predentin, numerous foci appear in it, in which crystals of mineral salts are deposited. These lesions increase in size and turn into globules (balls). As the globules grow, they merge, and the predentin becomes mineralized and hard. This method of mineralization is called globular.
However, some predentin remains unmineralized. Along the periphery of the developing tooth crown, non-mineralized areas remain, which are called interglobular spaces.
In addition, the part of predentin adjacent to the pulp also does not undergo mineralization;
called pulpal predentin
. Sometimes these areas are called non-calcified pulpal dentin.
Dental pulp development
begins simultaneously with the development of dentin. The central mesenchymal cells of the dental papilla differentiate into fibroblasts, which produce collagen molecules and other components of the intercellular substance of the pulp.
Enamelogenesis (enamel development)
begins after dentin formation.
At this time, the supply of nutrients from the dental papilla through the basement membrane to the cells of the inner layer of the dental organ (enameloblasts) stops, since a layer of dentin appears between the enameloblasts and the vessels of the dental papilla. In this regard, nutrients begin to flow to the enameloblasts from the intermediate layer (pulp) of the dental organ. This leads to the fact that the nucleus from the basal part of the enameloblasts, the Golgi complex and the cell center move to the apical part of the cells. Therefore, the apical part of the enameloblasts turns into the basal, and the basal - into the apical, directed towards the dentin. This is called inversion.
Thus, the formation of dentin provokes the inversion of enameloblasts, and after the inversion, the formation of enamel begins.
On the granular ER of enameloblasts, a protein begins to be synthesized, the granules of which move to the apical part of the cell and form the cuticular plate. As the number of granules in the cuticular plate increases, this plate lengthens and turns into a pre-enamel prism. The more the length of the prism increases, the shorter the anameloblasts become and the further they move to the periphery. After the formation of pre-enamel prisms, enamel mineralization begins.
Simultaneously with the formation of enamel, resorption of the dentin surface occurs, which therefore becomes uneven (scalloped), due to which the enamel is firmly connected to the dentin.
Cementogenesis (development of cement)
occurs in the 6-7th month of a child’s life, when baby teeth begin to erupt and their roots begin to develop.
The structure of the tooth.
Enamel (enamelum) covers the crown and partially the neck of the tooth. The greatest thickness of enamel is on the chewing surface (up to 3.5 mm). Enamel is the hardest tissue in the human body. It consists of 3-4% organic substances and 96-97% salts of calcium phosphate, calcium carbonate and calcium fluoride.
The structural unit of enamel is an enamel prism . Enamel prisms in their longitudinal section have an S-shape, in a transverse section - multifaceted, convex-concave, etc. The prisms are arranged in bundles almost perpendicular to the surface of the dentin. The prism consists of an organic matrix, represented by a network of the finest fibers, and salt crystals. Between the prisms there is a less calcified adhesive substance.
On a longitudinal section of a tooth, Retinus lines , which in a cross section have the shape of rings. The existence of these lines is explained by periodic weakening of mineralization, as well as forceful effects on the tooth during chewing. In addition, dark and light Schräger stripes . The presence of these stripes is explained by the fact that when grinding the tooth, some bundles of enamel prisms were cut perpendicularly, others - longitudinally.
The enamel contains enamel spindles (fusus enameli), enamel bundles (fasciculus enameli) and enamel plates (lamina enameli).
Enamel spindles
- these are the sites of penetration of dentinal tubules into the enamel. Nutrients enter the enamel through the enamel spindles from the dentinal tubules.
Enamel bundles
- these are narrow strips of weakly mineralized enamel, starting at the border with dentin and not reaching its surface.
Enamel plates
- these are narrow strips of weakly mineralized enamel, starting at the border with dentin and ending on its surface.
The presence of enamel bundles and enamel plates weakens the structure of the enamel, since bacterial toxins and bacteria enter the enamel through these bundles and plates, which destroy it.
The strength and chemical composition of enamel depend on metabolism in the body. Water, ions, amino acids, glucose and other substances can penetrate through the enamel. These substances come from saliva. Saliva affects the permeability of enamel. The permeability of enamel increases under the influence of acids, parathyrine, alcohol and with a lack of calcium, fluorine, and phosphorus salts in food. Enamel is connected to dentin through interdigitation.
Cuticle enamel
(cuticula enameli) is a thin organic plate covering the enamel. The cuticle develops from the pulp of the dental organ. The cuticle quickly wears off on the chewing surface and remains only on the lateral surface of the enamel. The cuticle protects the enamel from the harmful effects of various chemicals.
Dentin (dentinum) consists of the main substance in which the dentinal tubules (tubulus dentinalis) pass. The composition of dentin includes 28% organic substances (mainly collagen) and 72% salts (calcium phosphate, magnesium phosphate and calcium fluoride). There are 2 layers in dentin: 1) the outer mantle, in which the collagen fibers are located radially, and 2) the inner pulpal layer, in which the collagen fibers are located tangentially (longitudinally).
In the peripheral part of the dentin of the crown and root of the tooth there are non-calcified areas. In the crown, these areas are relatively large and are called interglobular spaces, in the root area they are small and are called the granular layer of Tomes
. Interglobular spaces take part in the metabolism of dentin.
The inner part of the pulpal dentin does not contain salts (not mineralized) and is called a strip of predentin,
or
uncalcified dentin.
Dentinal tubules
start from the pulp cavity, have a radial direction and end on the surface of the dentin. Some tubules penetrate the enamel (enamel spindles). In the pulpal dentin, the density of dentinal tubules is 75,000 per 1 mm2, in the mantle - 15,000-30,000 tubules. In the crown of the tooth, the dentinal tubules branch weakly, in the dentin of the root - strongly.
The wall of the dentinal tubules consists of peritubular dentin, which differs in that the collagen fibers in it have a circular direction and are richer in mineralization. Dentin located between the dentinal tubules is called intertubular (intertubular).
The dentinal tubules contain the peripheral processes of dentinoblasts and contain fluid. Dentinal tubules take part in metabolism and have trophic significance.
Dentin contains weakly mineralized areas in the form of thin stripes. These sections are called Owen's lines . On a longitudinal section of a tooth, Owen's lines have a tangential direction, and on a transverse section, they have a circular direction.
The dentin surface facing the enamel has interdigitation that promotes its strong connection with the enamel.
Secondary dentin
is formed by dentinoblasts after tooth eruption in a strip of non-calcified pulpal dentin. Secondary dentin includes: 1) replacement dentin and 2) denticles.
Replacement dentin
produced by dentinoblasts when the outer surface of dentin begins to deteriorate. 2 weeks after dentin destruction, newly formed predentin appears. After another 2 weeks, this predentin undergoes mineralization. If the process of dentin destruction proceeds quickly, then replacement dentin does not have time to form and a defect occurs in the dentin.
Denticles
are formed by dentinoblasts in the dental pulp during inflammatory and dystrophic processes. There are denticles: 1) free, located in the pulp of the tooth; 2) parietal, adjacent to the wall of the pulp cavity; 3) interstitial, included inside the tooth wall.
Secondary dentin is characterized by an irregular arrangement of collagen fibers and dentinal tubules and an abundance of interglobular spaces.
Cement (cementum) covers the neck and root of the tooth, contains 30% organic and 70% inorganic substances (mainly calcium phosphate and calcium carbonate). There are 2 types of cement: 1) acellular, covering the neck and the part of the tooth root extending from the neck; 2) cellular, covering the apex of the tooth root.
Cell cement
similar to coarse-fibered bone. It contains cells - cementocytes (cementocytus) and multidirectional collagen fibers. Cementocytes are located in lacunae, from which tubules extend, connected to the same tubules or to dentinal tubules, through which the exchange of substances between cementum and dentin occurs. The tubules extending from the lacunae contain processes of cementocytes.
Acellular cementum
consists only of a cementing substance and collagen fibers directed radially and longitudinally. The radial fibers are embedded into the dentin with their inner ends, and the outer ends pass into the periodontal fibers and are embedded in the wall of the alveolar process of the jaw, forming a circular ligament of the tooth.
Dental pulp,
located in the pulp cavity of the crown and in the root canal of the tooth, it is a type of loose connective tissue. There are 3 layers in the dental pulp: 1) peripheral, adjacent to the wall of the pulp cavity; 2) intermediate, adjacent to the peripheral; 3) central.
Peripheral layer
The pulp is represented by dentinoblasts (dentinoblastocytus), which have a process shape, a length of about 20-30 µm and a thickness of 6 µm. The cytoplasm contains the Golgi complex, granular ER, mitochondria and sudanophil granules. Their peripheral process penetrates the dentinal tubule and takes part in metabolic processes and, possibly, in the perception of irritations. This is evidenced by the presence of acetylcholinesterase in the processes.
The intercellular substance of the peripheral layer of the pulp includes collagen fibers, glycosaminoglycans, proteoglycans, glycoproteins and other substances inherent in the intercellular substance of loose connective tissue.
Intermediate layer of pulp
represented by immature collagen fibers and poorly differentiated cells capable of differentiating into dentinoblasts.
Central layer of pulp
consists of fibroblasts, macrophages and adventitial cells, collagen and reticular fibers. The function of the pulp is trophic.
Periodontium is a dense connective tissue that belongs to the supporting (connecting) apparatus of the tooth and consists of collagen fibers. The inner end of these fibers is embedded in the cement of the neck and root of the tooth, and the outer end is embedded in the jaw bone. The periodontium contains layers of loose connective tissue through which blood vessels pass. The periodontal collagen fibers in the area of the tooth neck form a circular ligament.
The periodontium performs 2 functions: 1) holds the tooth root in the socket; 2) participates in tooth trophism thanks to blood vessels passing through layers of loose connective tissue.
The periodontium includes periodontitis, the bone of the alveolar socket of the jaw and the gum.
Eruption of baby teeth. Development of root and cementum. Milk teeth begin to erupt at the 6-7th month of a child’s life. Before eruption, pulp accumulates in the tooth crown, resulting in an increase in intrapulpal pressure, under the influence of which the tooth crown begins to move to the surface of the gum. The incisors erupt first, then the canines, then the molars.
The process of teething is influenced by nutrition, diseases, the presence of vitamins and other factors. After the crown of the tooth has erupted, its root begins to develop.
Root development
begins from the moment of teething.
If the tooth is single-rooted (incisor, canine), then the lower edge of the epithelial dental organ begins to grow into the mesenchyme. This growing edge is called the “Hertwig root epithelial sheath.”
Hertwig's vagina has the shape of a tube. Its growing edge is slightly tucked inward.
Peripheral mesenchymal cells adjacent to the inner surface of Hertwig's sheath differentiate into dentinoblasts, which begin to produce predentin of the tooth root, followed by its calcification.
The central mesenchymal cells differentiate into fibroblasts, which produce components of the intercellular substance of the tooth root pulp.
If the tooth is double-rooted (premolar), then from the edge of the enamel organ 2 processes grow towards each other. After the fusion of these processes, 2 holes are formed in the Hertwig sheath, and from each of these holes a new Hertwig sheath grows, inside which dentin and pulp of the tooth root are formed.
If a tooth has 3 roots (molars), then 3 processes extend from the lower edge of the enamel organ. After the fusion of these processes, 3 openings are formed, from each of which one Hertwig’s vagina extends.
Development of cement
begins with the fact that the mesenchymal cells of the inner layer of the dental sac differentiate into cementoblasts, which destroy the epithelium of the Hertwig vagina. As a result of contact of cementoblasts with dentin of the root and neck of the tooth, cementoblasts are activated and begin to produce the intercellular substance of cement (collagen, glycosaminoglycans, proteoglycans and other substances).
As the tooth root grows, cementoblasts move to its apex, wall themselves with cement and turn into process-shaped cementocytes located in the lacunae. Therefore, the cement in the area of the apex of the tooth root, in which the cementocytes are located, is called cellular cement. The cement of the neck of the tooth and the base of its root does not contain cementocytes, and is therefore called acellular cement.
Periodontal development
occurs due to the mesenchymal cells of the outer layer of the dental sac, which differentiate into fibroblasts that produce collagen protein and other components of the intercellular substance of connective tissue.
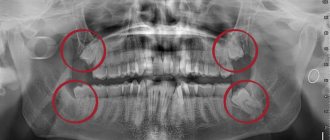
The replacement of baby teeth and the eruption of permanent teeth begins in the 6-7th year of a child’s life. In the 5th month of embryogenesis, permanent incisors and first molars are formed, then premolars and canines; second molars - in the 1st year, third molars - in the 4th-5th year of the child’s life.
Permanent teeth, which have milk precursors (incisors have incisors, canines have canines, premolars have molars), are laid below and behind the rudiments of milk teeth and are located in the same cavity with them. Later, the rudiments of permanent teeth are separated from the milk teeth by a bone septum.
As the dental plate lengthens, the rudiments of permanent molars appear on it, which do not have milk predecessors.
Eruption of permanent teeth that have deciduous predecessors
characterized by the fact that in the crown of a permanent tooth the amount of pulp increases, which presses on the crown, promoting its advancement towards the gum surface. At this time, osteoclasts destroy the bone septum between the permanent tooth germ and the root of the baby tooth. As the crown moves toward the gum surface, dentinoclasts and cementoclasts destroy the root of the baby tooth. At the moment when the root of the baby tooth is completely destroyed, the crown of the baby tooth, practically not held in place by anything, is easily pushed out by the crown of the permanent tooth.
The first to erupt after the first molar are the permanent incisors, then, within 9-14 years, the canines and premolars (small molars).
Eruption of permanent large molars (molars),
having no milk predecessors, is carried out in exactly the same way as the eruption of milk teeth, but only at a later date and after the lengthening of the dental plate. The first molar erupts at the 6-7th year of the child’s life, the second molar at the 9-14th year and the third molar at the 20-25th year.
Vascularization of teeth
carried out by the branches of the maxillary artery, penetrating through the main and additional openings in the apical part of the tooth root. In the dental pulp, the arteries branch into many anastomosing capillaries, which flow into a vein that leaves the pulp cavity through the same openings in the tooth root. The pulp contains lymphatic capillaries and small lymphatic vessels.
Blood flow in the pulp vessels is influenced by temperature and changes in mechanical pressure during chewing of food.
Innervation of the tooth
carried out by branches of the trigeminal nerve, the fibers of which end in receptors. There are unmyelinated nerve fibers ending with effectors on pulp vessels.
There is evidence that sensory nerve fibers penetrate into the initial sections of the dentinal tubules. These fibers perceive painful stimulation that occurs under the influence of pressure on them from the fluid located in the dentinal tubules. It is possible that painful stimuli are perceived by the processes of dentinoblasts, as evidenced by the presence of acetylcholinesterase in these processes.
Age-related changes in teeth
characterized by the fact that the enamel and dentin on the chewing surface are erased. The enamel becomes dull, cracks appear on its surface, and mineral salts are deposited. In enamel, dentin and cement, the content of organic substances decreases and the amount of mineral compounds increases. As a result, the permeability of these tissues to water, ions, amino acids, enzymes, and glucose decreases. As the body ages, new dentin formation stops. Cement, on the contrary, grows.
The dental pulp atrophies in old age, and the nutrition of the dental tissues is disrupted due to sclerosis of the blood vessels. The number of dentinoblasts decreases, some of them turn into dentinocytes.
Regeneration
There is no tooth enamel observed, dentin regeneration is carried out due to the formation of secondary replacement dentin, carried out by dentinoblasts.
Features of the process of the appearance of molars
The rudiments of permanent teeth are formed in the child in the womb in the fifth month of pregnancy. If no violations occurred during this period, then at about the age of one year, babies begin to develop molars inside their tissues. That is why the condition of baby teeth plays a big role. Any infection and pathology can affect this process.
Normally, by the age of 5–6 years, a child may exhibit symptoms of the eruption of the first molars:
- increased salivation;
- Possible runny nose or nasal congestion;
- increase in jaw size;
- loosening of a baby tooth;
- swelling of the gums;
- loss of a baby tooth;
- sore gums;
- elevated temperature;
- eruption of a permanent tooth.
At the moment when molars in children begin to grow and cut through the soft tissue of the gums, the root of the baby tooth is reabsorbed, which subsequently falls out on its own. The gum may be open for some time, then it heals. Between the loss and growth of teeth, it can take from several days to 2-3 weeks.
Possible problems when changing teeth
The eruption of baby teeth causes a lot of worries and problems, since often the first teeth come through very painfully and the baby becomes capricious, sleeps poorly and refuses to eat.
There are no such problems with the growth of molars, but more serious difficulties may arise:
- delayed eruption;
- preservation of baby teeth;
- growth of a superset of teeth;
- displacement, torsion and other malocclusions;
- absence of molars.
All these pathologies can be the result of hereditary predisposition, gene mutations, problems with intrauterine development, jaw trauma, immunodeficiency diseases, mineral deficiencies, diseases of the oral cavity or baby teeth.
Recommendations
It is already extremely difficult to avoid complications during teething, since all pathological changes occur during the period of their development. It is for this reason that experts advise the prevention of dental anomalies and diseases even during a woman’s pregnancy.
Recommendations from dentists.
- During pregnancy, a woman should take all prescribed vitamins, treat infectious diseases, including caries, and eliminate bad habits.
- Start visiting the dentist at 1–2 years of age.
- Do not avoid treating any dental disease in baby teeth.
- Monitor your child's oral hygiene.
- Regularly undergo preventive examinations with a dentist.
Parents should explain to the child that molars are permanent and if they are damaged or removed, new ones will not grow. For this reason, they should be taken care of from day one.
Note!
We draw your attention to the fact that each child’s body is strictly individual and there are no “strict deadlines for the eruption and loss of teeth”; we can only clearly identify the sequence of appearance of teeth in the mouth. All terms are given with a certain degree of convention (±2-3 months), based on the most common situation in the practice of dentists. Therefore, do not be alarmed if the number of teeth in your baby’s mouth does not correspond to the tabulated data. To be more sure or if something worries you, it is recommended to show your baby to a pediatric dentist.
Please note that all information is provided for informational purposes only.