Hemifacial spasm was first described by Gowers in 1884 and is a segmental myoclonus of muscles innervated by the facial nerve. The disease occurs at the age of 50-60 years, almost always on one side, although sometimes, in severe cases, there is bilateral damage. Hemifacial spasm usually begins with short clonic movements of the orbicularis oculi muscle and over the course of several years affects other facial muscles (frontal, subcutaneous, zygomatic, etc.).
Clonic movements gradually progress to sustained tonic contractions of the involved muscles. Chronic irritation of the facial nerve or nucleus (which is considered the main cause of hemifacial spasm) can occur due to various reasons.
The muscles of the face are susceptible to the same movement disorders as the muscles of the limbs or trunk. Myoclonus, dystonia and other movement disorders manifest themselves in the form of specific syndromes in the facial muscles. A clear understanding of the mechanism of development of disorders allows for correct diagnosis and selection of adequate treatment.
Causes of hemifacial spasm include vascular compression, nerve compression from mass lesions, brainstem lesions from stroke or multiple sclerosis, and secondary causes such as trauma or Bell's palsy.
Although there are various treatments for craniofacial movement disorders, chemodenervation with botulinum toxin has proven to be very effective in treating these disorders, outperforming both medical treatment and surgical treatment in some cases.
Stimulation of the facial nerve nucleus is thought to result in hyperexcitability of the nucleus, while stimulation of the proximal nerve may result in ephaptic transmission within the facial nerve. This mechanism explains the rhythmic, involuntary myoclonic contractions that occur with hemifacial spasm.
Compressive lesions (eg, tumor, arteriovenous malformation, Paget's disease) and noncompressive lesions (eg, stroke, multiple sclerosis, basilar meningitis) may present with hemifacial spasm. Most cases of hemifacial spasm, previously considered idiopathic, were probably caused by abnormal blood vessels and compression of the facial nerve within the cerebellopontine angle.
Epidemiology
Hemifacial spasm occurs in people of different races with equal frequency. There is some predominance of this disease in women. Idiopathic hemifacial spasm usually develops in the fifth or sixth decade of life. The development of hemifacial spasm in patients younger than 40 years of age is unusual, and is often a symptom of a neurological disease (eg, multiple sclerosis).
Symptoms
Involuntary movements of the facial muscles are the only symptom of hemifacial spasm. Fatigue, anxiety or reading can speed up movements. Spontaneous hemifacial spasm involves facial spasms, which are myoclonic spasms and are similar to segmental myoclonus, which can occur in other parts of the body. Postparalytic hemifacial spasm, such as after Bell's palsy, manifests as facial synkinesis and contracture.
There are a number of conditions similar to hemifacial spasm.
Spasm of the masticatory muscle
Hemispasm of the masticatory muscle is similar to hemifacial spasm and occurs when the motor trigeminal nerve is irritated. This is a rare condition that is segmental myoclonus, and is manifested by unilateral involuntary contractions of the muscles innervated by the trigeminal nerve (mastication). As with hemifacial spasm, hemispasm of the masseter muscle is well treated with medication and botulinum toxin. In addition, there is evidence that surgical treatment may be effective in some cases.
Myoclonic movements
Myoclonic movements in the facial muscles can also occur with lesions of the brain or brain stem. They differ from hemifacial spasm in the distribution of abnormal movements (more generalized, possibly bilateral), and can be diagnosed by neurophysiology. Imaging techniques can reveal deeper causes. Central myoclonus responds well to anticonvulsant therapy.
Oromandibular dystonia
Oromandibular dystonia is a muscular dystonia that affects the lower musculature of the face, primarily the jaw, pharynx and tongue. When oromandibular dystonia occurs in combination with blepharospasm, it is called Medge's syndrome.
Botulinum therapy is most effective in the treatment of oromandibular dystonia. Medications are also used to a certain extent for oromandibular dystonia.
Craniofacial tremor
Craniofacial tremor may be associated with essential tremor, Parkinson's disease, thyroid dysfunction, and electrolyte imbalances. This condition rarely occurs in isolation. Focal motor seizures sometimes need to be distinguished from other facial movement disorders, particularly hemifacial spasm. Postictal weakness and increased involvement of the lower face are hallmarks of focal motor seizures.
Chorea of the face
Facial chorea occurs in the context of a systemic movement disorder (eg, Huntington's disease, Sydenham's chorea). Chorea is an episodic complex of movements without a pattern. A similar condition, spontaneous orofacial dyskinesia, occurs in older edentulous people. As a rule, the installation of prostheses gives a good effect.
Tiki
Facial tics are short, repetitive, coordinated spontaneous movements of grouped muscles of the face and neck. Tics may occur physiologically or due to diffuse encephalopathy. Some medications (eg, anticonvulsants, caffeine, methylphenidate, antiparkinsonian drugs) may cause tics. Single, repetitive, stereotypical movements are characteristic of tics.
Facial myokymia
Facial myokymia manifests itself as worm-like twitching under the skin, often with a wave-like distribution. This condition is distinguished from other abnormal facial movements by the characteristic EMG discharges, which are short, repeated bursts of motor unit potentials in the range of 2-60 Hz, with periods of silence of up to several seconds. Facial myokymia can occur with any process in the brain stem. Most cases of facial myokymia are idiopathic and resolve on their own within a few weeks.
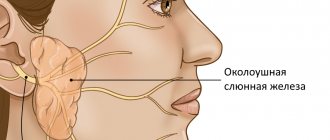
Facial neuritis causes, symptoms, treatment and prevention methods
Massage
First, the exclusively healthy side of the face, the collar area, is massaged, therapeutic exercises, and positional treatment are performed.
The purpose of the massage is to neutralize swelling and congestion, improve lymph and blood circulation in the facial muscles, restore the conduction of nerve impulses along the facial nerve and the function of facial muscles, and prevent the development of contractures. For a positive result, on average, 10 to 20 sessions of 5–15 minutes are required, depending on the degree of nerve damage, the dynamics of recovery, and the goals of therapy. In the early period, a gentle acupressure of the face, neck, collar area, and shoulder girdles is performed using stroking, rubbing, kneading, and vibration. Facial massage is not prescribed for atherosclerosis, active tuberculosis, high fever, blood diseases, or oncology.
Physiotherapy
Physiotherapy for neuritis of the facial nerve helps to alleviate the severity of symptoms, improve conductivity and restore the functions of the facial nerve, and activate microcirculation and metabolic processes. The procedures combine well with drug treatment, are safe when used correctly, cause virtually no adverse reactions, are painless, and have a long-lasting effect.
From the first day of treatment for facial neuritis, physiotherapy is prescribed in the form of non-contact heat, positioning treatment, and adhesive plaster tension. From 5–6 days, the following physiotherapy procedures are performed according to indications:
- therapeutic effect of an ultra-high frequency electric field
- ultrasound
- electrophoresis of drugs
- transcutaneous electrical nerve stimulation;
- myoelectrostimulation
- local darsonvalization (exposure to tissue with low-power alternating electric current)
- microwave therapy
- laser blood irradiation
- ozokerite treatment
Drug treatment
The doctor recommends drugs for the treatment of facial neuritis in the case of a particular patient, paying attention to the causes and characteristics of the course of the disease, the severity of symptoms, and the presence of concomitant pathologies.
The standards of drug treatment for facial neuritis include:
- analgesics
- decongestants
- B vitamins
- antiplatelet agents
- non-steroidal anti-inflammatory drugs
- vasodilators
Usually, for neuritis of the facial nerve, tablets are prescribed. To enhance their effect, an ointment or gel with an analgesic, local irritant, and warming effect is used externally. If necessary, to achieve the desired effect as quickly as possible, medications are administered intramuscularly.
With slow nerve recovery, glucocorticosteroids are prescribed, drugs that improve metabolic processes in the nervous tissue. If complete recovery does not occur within two to three months, the treatment program includes biostimulants and hyaluronidase. In case of secondary neuritis of the facial nerve, the underlying disease is treated simultaneously with symptomatic therapy.
Surgery
In case of complete rupture of the facial nerve, congenital neuritis, and lack of effect from conservative therapy after 7–11 months, surgery is necessary. In order to restore the conductivity of the facial nerve and the motor functions of the facial muscles, stitching and plastic surgery of the damaged nerve trunk are performed. To reduce the cosmetic defect, plastic surgery of the facial nerve is performed using autotransplantation. If there is a significant decrease in hearing, hearing aids are performed.
Surgical treatment makes sense during the first year of the disease; later, irreversible atrophy of the facial muscles occurs.
Other treatments
In the complex treatment of facial nerve neuritis, acupuncture is used. Sterile single- or reusable needles are inserted into pre-selected points at different depths, which are heated and rotated to enhance the therapeutic effect. Other treatment and rehabilitation measures help restore the functions of the facial nerve and facial muscles, and neutralize the symptoms of neuritis:
- reflexology
- biofeedback (biofeedback training)
- immunosorption (selective purification of blood from antibodies and antigens)
- local medicinal baths
- facial taping (adhesive tape tension)
- mask made of clay, paraffin
- botulinum toxin injections to eliminate muscle contractures
Diagnostics
Early cases of hemifacial spasm are sometimes difficult to distinguish from facial myokymia, tics or myoclonus, which may be caused by pathological processes in the cerebral cortex or brainstem. In such cases, neurophysiological testing is the most valuable diagnostic method.
Wide and variable synkinesis on eyeblink tests and high-frequency discharges on electromyography (EMG) with associated clinical manifestations are diagnostic criteria for hemifacial spasm. Stimulation of one branch of the facial nerve can spread and cause a response in the muscle innervated by another branch. Synkinesia is absent in essential blepharospasm, dystonia or epilepsy. Needle myography shows irregular, short, high-frequency burst potentials (150-400 Hz) of motor units that correlate with clinically observed facial movements.
Visualization methods
Magnetic resonance imaging is the diagnostic method of choice when there is a need to exclude compression effects. Angiography of the cerebral vessels is generally of little value in the diagnosis of hemifacial spasm. Ecstatic blood vessels are rarely identified, and these vessel findings may be difficult to correlate with nerve effects. Performing angiography and/or magnetic resonance angiography is typically used to perform surgical vascular decompression.
Facial nerve neurosis
Neurosis of the facial nerve is sometimes confused with neuritis, although it has nothing to do with inflammation. Tibetan medicine classifies it as a disease of the Wind system and considers its main cause to be nervous, emotional stress, psycho-emotional disorders, and mental fatigue. Often this disease accompanies depression, anxiety and fear neuroses.
Symptoms of facial neurosis are spasms of facial muscles, nervous tics in the form of blinking, twitching of the face, obsessive, involuntary swallowing. Sometimes nervous tics are accompanied by a feeling of numbness, tingling or burning.
Muscle twitching can start from the cheek, then move to the eye area, the orbicularis muscle. This causes symptoms of blepharospasm - frequent blinking, photophobia, dry eyes. When severe, blepharospasm can result in the inability to see out of one eye.
What to do if the facial nerve on the cheek twitches? Symptomatic treatment of facial neurosis consists of the use of antispasmodics, sedatives, and anticonvulsants. In Eastern medicine, these drugs are not used because they do not affect the cause of the disorder. Instead, the Tibet Clinic uses complex herbal medicine.
Herbal medicines of Tibetan medicine have an equally effective sedative, calming effect and at the same time help:
- restore the overall balance of the nervous system,
- improve and stabilize emotional state,
- restore psycho-emotional stability,
- eliminate symptoms of stress, mental overload, fatigue,
- increase the stability of the nervous system under stress.
These herbal remedies are used in the complex treatment of anxiety neuroses, fear, depressive and other disorders of the nervous system. They complement well acupuncture, acupressure, moxotherapy, relaxation massage, stone therapy and other methods of oriental medicine. With their help, doctors at our clinic effectively eliminate the symptoms and causes of facial neurosis and restore normal tone of facial muscles.