Surgical removal of the parotid gland is called a parotidectomy . In most cases, surgery is performed due to the presence of a tumor, often benign, of the parotid salivary gland.
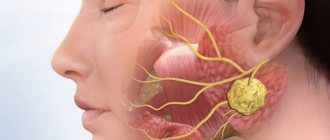
Parotid salivary gland and facial nerve - schematic drawing
The salivary glands secrete saliva into the mouth to digest food and protect against infections. When the parotid glands are removed, there are no problems with the secretion of saliva - this function will continue to be performed by the remaining salivary glands: the submandibular, sublingual, and numerous small glands.
The parotid gland is penetrated by nerves, veins and arteries. We are interested in the facial nerve.
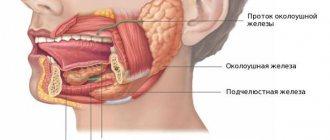
Removal of the parotid, submandibular gland, removal of cervical lymph nodes
The salivary glands are divided into minor and major salivary glands. There are 3 pairs of large salivary glands: the parotid salivary glands, located below and in front of the auricle directly under the skin, the submandibular salivary glands and the sublingual glands, located under the mucous membrane of the floor of the mouth. The minor salivary glands are located in the mucous membrane of the mouth, palate, cheeks and lips. Various tumors, stones, and recurrent infections are the most common reasons for operations on the salivary glands.
Symptoms
A stone located in the duct of the salivary gland clogs the duct and prevents the flow of saliva into the mouth. In this case, saliva collects in the salivary gland, which becomes swollen and often painful. Depending on the location of the stone, pain and swelling occurs either under the jaw (submandibular gland) or in front of the auricle and in the area of the angle of the jaw bone (parotid gland). Some stones can be removed endoscopically through the mouth under local anesthesia as an outpatient procedure, but sometimes the entire salivary gland must be removed. Most often, stones are found in the submandibular gland.
The tumor is usually palpable as a nodule in the salivary gland and can cause swelling, pain, and facial nerve dysfunction. Even a benign tumor usually must be removed.
Sialadenitis - symptoms and treatment
Diagnostic measures for diseases of the salivary glands can be divided into clinical, laboratory and instrumental.
Clinical methods include the collection of complaints, anamnesis (medical history), as well as direct examination of the patient.
During the questioning, the patient’s complaints are clarified, the time of their occurrence, the nature, intensity of pain, the impact of these symptoms on the quality of life, the presence of relapses and remissions, and their duration are specified. Separately, it is worth dwelling on questions about the presence or absence of somatic and infectious diseases - sometimes they can be a cause or an aggravating factor in the course of sialadenitis. It is worth clarifying whether parents and relatives had similar conditions.
During the clinical examination, the doctor pays attention to the presence of swelling and asymmetry of the face, the size, consistency, shape and relief of the affected and healthy salivary gland. These data largely depend on the primary nature of the disease, the presence of relapses and the nature of the treatment performed or its absence. The more relapses there were, the more sclerotic the gland was, which negatively affected its functioning. In the oral cavity, you should pay attention to the mouth of the excretory duct, and also examine the excretory duct itself (if possible) for the presence of salivary gland stones and other pathological changes. It is important to determine whether there is salivation. To do this, massage the gland tissue, after which the amount of saliva, its color and consistency are assessed.
Laboratory methods are required if sialadenitis is suspected. Blood, urine and saliva itself are examined. A general blood test can detect leukocytosis (increased levels of white blood cells) - the primary sign of inflammation. In blood biochemistry, special attention should be paid to blood glucose levels, and in urine - to the amount of salts. In saliva you can find a large number of leukocytes, impurities and pus, possibly the presence of bacteria and sand. Physicochemical parameters of saliva are given special attention [8].
One of the first hardware diagnostic methods for diseases of the salivary glands includes an x-ray of the gland - sialography . It allows you to determine the presence of stones in the thickness and excretory duct of the gland. sialography with contrast appeared , with the help of which it is possible to detect not only stones, but also to identify a narrowing of the lumen of the excretory duct, the presence of cysts and other neoplasms that impede the normal functioning of the gland.
The most modern sialogram method is digital dynamic sialography , through which it is possible to eliminate the overlap of the bone components of the jaws, visualize the soft tissue component of the gland and evaluate the flow of saliva through the duct. Among other things, it significantly reduces the radiation dose to the patient.
Computer and magnetic resonance sialotomography of small foreign bodies (stones) in the excretory duct and the gland itself.
The sialosonography method gives a fairly complete picture of the structure of the gland. With its help, you can easily identify sclerotic changes in tissues, foreign bodies, estimate their number, density, size, and also exclude the presence of neoplasms.
Thermosialography makes it possible to study the dynamics of changes in the temperature of the gland. This allows you to evaluate the effectiveness of the treatment.
Ultrasound-guided salivary gland biopsy is a fairly common diagnostic method. It is especially effective in the presence of cavities (cysts) in the thickness of the glandular tissue [9].
Currently, both throughout the world and in Russia, the most minimally invasive and informative method for diagnosing lesions of the salivary glands is widespread - sialoendoscopy . Modern devices help to visualize not only the excretory and intraglandular ducts, but also the ductal system, up to ducts of 2-3 orders, sometimes it is even possible to examine ducts of 4-5 orders.
The presence of a second working channel in the endoscope body allows not only visualization, but also washing, expansion of the duct, and, if necessary, collection of biopsy material. Using an endoscope, you can evaluate the color of the walls of the excretory duct, their elasticity, and detect the reasons that impede the normal flow of saliva through the ducts - stones, mucus plugs, polyps, neoplasms, areas of narrowing of the lumen of the duct. Also, thanks to endoscopic support during surgery, you can not only get a complete picture of the problem, but also eliminate it with minimal intervention.
Salivary gland removal procedure
The operation to remove the salivary gland is performed under general anesthesia. The operation to remove the parotid gland lasts from 1 to 2 hours and the submandibular gland less than 1 hour.
The facial nerve passes through the parotid gland and the inferior branch of the facial nerve is located in the surgical site. Therefore, when the parotid gland is removed, small needle cables are placed on the face for the duration of the procedure to identify the facial nerve.
During surgery to remove a tumor, we also try to remove nearby tissue, but this is not always successful due to the location of the facial nerve. The submandibular gland is usually removed completely.
Complications after surgery
During surgery to remove the parotid gland, the facial nerve can be impacted, sometimes causing facial nerve palsy, usually the inferior branch, which can cause the corner of the mouth to droop. Typically, facial nerve paresis recovers within a few weeks with facial exercises, and only in rare cases does the facial nerve fail to recover.
Sometimes the cancer affects the facial nerve and then the facial nerve is completely removed, in which case the paralysis is permanent. However, the condition can usually be improved through various surgical interventions.
After removal of the parotid salivary gland, the pinna of the ear is usually partially numb, but over time some sensitivity returns. Due to the risk of frostbite, the auricle must be properly protected from the cold.
During surgery to remove the submandibular gland, the facial nerve may be injured (stretched), causing temporary dysfunction of the corner of the mouth, but permanent damage caused by this branch of the facial nerve is very rare. Damage to the sensory and motor nerves passing under this gland is extremely rare.
After parotid surgery, saliva may leak from the wound, especially when eating. Salivary secretion is harmless and usually ends spontaneously. Surgery to remove one salivary gland does not cause noticeable dry mouth.
Inflammatory processes
Sialadenitis - inflammation of the parotid salivary glands - is the most common problem that occurs in this area. The inflammatory process, as a rule, is one-sided and has a viral or bacterial origin. Sialadenitis of the parotid gland occurs in both acute and chronic forms.
The parotid glands have a lobular structure, are well supplied with blood, and produce a third of the total daily secretion volume
Reasons for the development of the inflammatory process in the OSJ:
- past infectious diseases;
- playing wind instruments (increased load on the masticatory muscles of the face adjacent to the OSJ);
- previous operations;
- stenosis of the OSJ duct;
- high blood pressure.
Types of inflammation
There are several types of sialadenitis (depending on the cause):
- acute contact (develops as a complication of an abscess (boil) localized next to the OSJ, secondary infection);
- blockage and inflammation of the gland duct with food particles, toothbrush villi or other foreign body;
- mumps (you can recognize this disease by the characteristic swelling of the cheeks and neck);
- acute lymphogenous (not only the parotid glands themselves become inflamed, but also the lymph nodes, as well as subcutaneous fatty tissue);
- chronic interstitial (complication of previous surgery or previous infections);
- parenchymal (occurs in a chronic form, the cause is a cyst in the OSJ).
Mumps
The symptoms of this type of inflammation are the most striking. The pathological process affects one or both OSJs at once, leading to a decrease in the amount of synthesized secretions, dry mouth and digestive problems. The risk group is children 3–10 years old with reduced immunity. Mumps most often occurs during the cold season (especially after suffering from infectious or viral illnesses).
Children aged 3 to 10 years are most susceptible to mumps.
Classic signs of mumps:
- intense pain in one (both) parotid salivary glands;
- feverish state (chills, sharp rise in body temperature);
- swelling of the face;
- dry mouth;
- saliva becomes cloudy and thick;
- an unpleasant putrid taste appears in the mouth, pus may be released;
- chewing and swallowing are difficult and painful;
- decreased appetite;
- the neck muscles are tense, painful on palpation, pain radiates to the ear, temple, nose.
A mild form of mumps can be virtually asymptomatic. The affected gland slightly increases in size and may be painful on palpation. Moderate inflammation begins with an increase in body temperature, which is accompanied by general weakness and severe headaches. This form of the disease, as a rule, affects both glands - they swell, become large, and extremely painful.
Salivation sharply decreases, the oral mucosa is hyperemic. Pressure on the gland most often leads to the release of pus. Loss of appetite, chills, and fever are classic signs of severe mumps. The area of the glands, the entire neck, and face are swollen. The auditory canal narrows, swallowing function is impaired.
Increased size, swelling, pain when pressed are the main signs of inflammation of the OSJ (sialoadenitis)
Important! An alarming signal is the appearance of an area of erosion on the skin above the gland, through which dead cells of the OSJ and purulent exudate are released. The gangrenous (severe) form of mumps, if left untreated, can result in sepsis (blood poisoning). Treatment tactics for mumps depend on the severity of the disease and the age of the patient. As a rule, the patient is prescribed bed rest, systemic and local drug therapy.
Sjögren's syndrome
It is noteworthy that sialadenitis of the parotid salivary gland can also be of autoimmune origin - develop as a result of the pathological production of antibody cells by the body itself. Autoimmune inflammation of the OSJ is called Sjögren's syndrome. The main provocateurs for the development of this pathology are genetic predisposition and viral infections. When the virus enters the glandular tissue, “local” cells are destroyed due to increased synthesis of lymphoid cells.
Treatment of autoimmune inflammation is exclusively symptomatic.
Principles of treatment of sialadenitis
Mild and moderate forms of the inflammatory process are indications for bed rest. Symptomatic treatment of sialadenitis involves the use of antipyretic, analgesic drugs, as well as dry warming compresses (the latter measure provided that the patient’s body temperature has not risen above 37.2 degrees). Pleomorphic adenoma is a common benign formation of the spinal cord and is an indication for surgical intervention.
It is very important to maintain a drinking regime (at least 2.5 liters of water per day), since the inflammatory process in the OSJ leads to a decrease in secretion production, dry mouth and digestive problems. In addition, a patient with sialadenitis must follow the so-called salivary diet - eat fermented milk products, fiber (vegetables, fruits). To reduce the load on the chewing muscles and facilitate digestion, it is recommended to first grind all food in a blender (food processor).
Careful oral hygiene is an important condition for the speedy recovery of patients with sialadenitis. In addition to the usual twice-daily brushing of your teeth, it is recommended to rinse your mouth with a soda solution (1 teaspoon of powder per glass of warm boiled water) after each meal. Based on the cause of inflammation, the patient is prescribed antibiotic therapy or antiviral drugs. Severe forms of sialadenitis are treated exclusively in a hospital setting (including surgery).
Treatment of sialadenitis is complex, involves taking antipyretic and painkillers, antibiotic therapy, and the use of dry compresses
Possible complications of OSJ inflammation
In the absence of timely treatment of sialadenitis, the disease can result in:
- breakthrough of an abscess into the ear canal (with a purulent form of inflammation);
- melting of the walls of large vessels with subsequent bleeding;
- parotid hyperhidrosis (increased work of “local” sweat glands);
- suppuration, swelling of the surrounding soft tissues;
- blockage of the salivary duct, formation of fistulas.
It is noteworthy that mumps can result in testicular atrophy in men (that is, infertility).
Removal of cervical lymph nodes (cervical dissection)
When removing a malignant tumor of the salivary gland, the cervical lymph nodes are usually removed, a so-called cervical dissection is performed. The lymph node is usually small, surrounded by a bean-shaped capsule, and lymph fluid flows through it. There are a large number of lymph nodes in the neck.
The first metastases of salivary gland cancer are usually found in the cervical lymph nodes and therefore it is believed that their removal is necessary in the case of cancer. Typically, surgery to remove the salivary gland, which also involves a cervical dissection, takes 1 to 2 hours longer.
Submandibular gland
Removing the pancreas is an important surgical procedure. It is one of the two largest salivary glands in the human body, the other being the parotid gland. The most common reason for gland removal is due to recurrent infections and/or blockages that cause swelling (chronic sialolithiasis). Another reason is the presence of an abnormal mass contained in the gland (benign or malignant).
The pancreas and inflammation of the glandular ducts are the causes of swelling and, as a result, pain and discomfort. When a blockage occurs, backflow occurs, causing saliva to accumulate behind the occlusion. When this happens, the salivary glands swell in size. Over time (for example, between meals), the body resumes saliva production, and the saliva is compressed back and forth until the next meal, which activates the gland and produces more saliva, leading to the development of edema.
Initial (surgical) treatment is as follows:
Apply hot compresses to the widened area of the mouth two to three times a day. After applying the warm compress, give a very gentle (orthogonal) massage to the swollen areas.
Mix dry and sour candies. These sweets stimulate saliva production.
Increase your water intake to two liters per day. Try to avoid caffeine as it acts as a diuretic and can dehydrate the body.
The gland may or may not become infected. If there is inflammation, your doctor will prescribe an antibiotic, usually over a 3-week period. Use the antibiotic as directed and complete the full program even if symptoms subside.
Over the course of 3-4 weeks, the gland slowly returns to its normal shape. If the above precautions do not help, surgical removal is the next step.
If there is an abnormal mass, it may not change in size or even disappear. Unlike a blockage, swelling due to a mass does not change with food intake. Most masses grown in the submandibular gland are caused by benign tumors such as aphthoma or Warthin's tumor. These tumors are usually painless and move easily when palpated. Even if they are benign, tumors must be removed because they will not heal themselves and will continue to grow over time, causing facial distortion. Usually after decades, these benign tumors can also develop into cancer (carcinoma in pleural adenoma).
Unfortunately, some masses can be cancerous and include mucoepidermoid carcinoma, basal cell carcinoma, and metastases from skin cancer (squamous cell carcinoma is the most common). If there is pain, numbness over the chin or teeth, tongue or mouth, or facial paralysis, the likelihood that the mass is cancerous increases.
Typically, submandibular mass testing involves a CT scan as well as a fine needle aspiration (FNA) of the mass itself. Obtaining an FNA is useful in determining the extent of surgical removal. If malignancy is detected, a more extensive surgical procedure is required, including complete removal of the gland as well as surrounding lymph nodes (lymphatic clearance).
A common concern patients have regarding surgery is whether it will affect their saliva production. The answer is NO.
Sialolithotomy
In cases where there is a stone in the submandibular gland duct, an option you can try before removing the entire gland is a procedure called saliototomy. In fact, only the stone itself can be removed. If the stone is located near the mouth, this procedure can be performed at a local anesthesia clinic.
If the stone is more than 1.5 cm from the canal opening, the procedure must be performed in the operating room under general anesthesia. In this case, a small catheter is usually left in place to prevent scar tissue from closing the lumen and is removed after about 5 days.
Dangers of this process include infection and bleeding. A rare risk of this process is the development of scar tissue in the canal, which leads to recurrent swelling of the gland. There is also a small risk of numbness in the mouth.
Removal of submandibular glands
In cases where saliototomy cannot be used as an option or where a true mass exists, the entire gland should be removed. This is achieved by reducing approximately 3 cm below the body of the mandible to a length of approximately 4-5 cm. Anatomically, the omentum is prepared by carefully ligating the large vessels and preventing damage to the nerves. The defect is detected and it is ligated. The incision is closed with a plastic suture. The whole process takes about 1-2 hours.
Depending on how the surgery goes and how healthy the patient is, he may leave the clinic the same day or the next day. Surgical drains are usually removed within 24 hours and sutures 5-7 days after surgery. Pain after surgery is minimal, and in most cases people do not even need painkillers. Patients can eat as they please, but any exercise or heavy lifting is prohibited for the first 1-2 weeks after surgery.
Surgical risks include bleeding and infection. However, rare risks of subnuclear ablation include permanent lip paralysis, permanent tongue paralysis, and numbness in the lower part of the mouth.
Why is this happening? Because the nerves that go to the rim, tongue and larynx pass through the subeye and are at risk of injury.
Sometimes there may be temporary damage to the nerves and their function may return over time (weeks or months), but in some cases it may never return. The use of radio wave diathermy for vascular ligation and basal nerve conduction monitoring with a neurostimulator significantly reduces intraoperative and postoperative risk.
Endoscopic salnioscopy
Pancreatic endoscopy is performed by introspection, resulting in minimal (if any) incisions in the mouth or throat.
If you have problems with the submaxillary gland, please contact our clinic to schedule an appointment.