Macroglossia is an enlargement and thickening of the tongue that occurs as a result of a pathological process or as a developmental anomaly. It can develop evenly (diffuse enlargement of the tongue) or partially involving the root, back or lateral surfaces of the tongue. The tongue does not fit in the mouth, protrudes outward, teeth imprints are detected on it, and speech impairment occurs. In the classification criteria, macroglossia is distinguished between true (congenital and acquired) and relative (with micrognathia) [1, 2]. Congenital macroglossia is more common in childhood and is the result of hypertrophy of the tongue and vascular developmental anomalies (Beckwith-Wiederman syndrome, neurofibromatosis type I, Starge-Weher hemangiomatosis, congenital lymphangioma). Macroglossia associated with hereditary metabolic disorders is observed in hypothyroidism, Huller syndrome, Sanfilippo syndrome [3]. Acquired macroglossia is most often associated with amyloidosis, a group of diseases characterized by the deposition of specific interstitial insoluble fibrils in organs and tissues, leading to severe functional impairment and death [4, 5]. Various tumors of the oral cavity (squamous cell carcinoma, verrucous carcinoma, lymphoepithelial carcinoma, squamous interepithelial neoplasia) can cause macroglossia. It develops extremely rarely with syphilis and tuberculosis [6].
Enlargement of the submandibular salivary glands (MSGs) is observed in a number of rheumatic (autoimmune sialadenitis in Sjogren's disease and syndrome, IgG4-related sialadenitis, ANCA-associated vasculitis, etc.), dental (viral/bacterial sialadenitis, sialosis, etc.) and oncohematological diseases (B- and T-cell lymphomas with damage to the salivary glands, plasmatic dyscrasias, etc.) [7, 8].
AL amyloidosis is a systemic oncohematological disease related to plasmatic dyscrasias. It is characterized by the deposition in various organs and tissues of a protein formed from the variable part of monoclonal light chains of immunoglobulins as a result of clonal plasma cell proliferative disorders. It is known that 15% of patients with AL amyloidosis have a unique symptom complex associated with a massive increase in the frequency of heart function, the development of diffuse macroglossia with tongue biting and a change in voice timbre. Periorbital edema, carpal tunnel syndrome, purpura, and muscle hypertrophy develop in 40% of patients with AL amyloidosis [9]. The average life expectancy of patients with AL amyloidosis ranges from 1-1.5 years after diagnosis, while when the heart is involved in the process, it is only 5 months. Dental manifestations of the disease may long precede the development of severe functional disorders of the heart, gastrointestinal tract and kidneys [10, 11]. Therefore, knowledge of soft tissue lesions in AL amyloidosis can significantly improve early diagnosis and significantly increase survival of patients with this severe systemic disease. Our observation can serve as an example of late diagnosis of soft tissue lesions in AL amyloidosis.
Patient A
., 61 years old, October 10, 2014, was admitted with complaints of a dense tumor-like formation in the submandibular region, enlarged tongue and periodic biting of the tongue, difficulty swallowing when eating, hoarseness of voice, numbness of the fingers and limitation of movements in the hands and right shoulder joint , hemorrhagic rashes on the skin of the neck (Fig. 1).
Rice.
1. Macroglossia, increased PFS and diapedetic hemorrhages on the skin of the neck (a) and in the supraclavicular area (b) in a patient with AL amyloidosis. The patient has been aware of herself since March 2013, when she noticed the appearance of tumor-like formations in the area of the prostate gland, which gradually increased in size and merged into a single conglomerate. She was examined at her place of residence. According to ultrasound examination (ultrasound), exacerbation of chronic parenchymal sialadenitis was diagnosed. Standard therapy for acute sialadenitis was carried out: antibacterial and anti-inflammatory drugs. Cytological examination of the thyroid gland did not reveal tumor growth. The tumor formation continued to increase further, numbness in the fingers and difficulty clenching the hand into a fist appeared. In March 2014, due to the ineffectiveness of therapy, a biopsy of the prostate gland and magnetic resonance imaging (MRI) were performed. Hyperplasia in chronic sialadenitis was diagnosed. According to the studies conducted, Mikulicz's disease (damage to the parathyroid gland and sublingual salivary glands) was diagnosed and the patient was referred for consultation to an oncologist to resolve the issue of radiation therapy. Radiation therapy was performed with a total radiation dose of 46 Gy. Despite the therapy, the disease progressed, the tongue significantly increased in volume, the dryness of the mouth increased, swallowing of food was impaired, and movement in the hands and shoulder joint became limited. In October 2014, an MRI examination of the head was performed with a puncture biopsy of the tongue; the diagnosis of a tongue tumor was excluded. A patient with a diagnosis of sialadenitis of the parathyroid gland was sent for consultation to the Research Institute of Rheumatology named after. V.A. Nasonova and was hospitalized with a diagnosis of AL-amyloidosis with soft tissue damage (increased PFS, macroglossia, carpal tunnel syndrome, tendon flexion contractures of the hands, diapedetic petechial skin rashes). On admission: condition of moderate severity, asthenic physique (weight loss per year 25 kg). Flexion contracture of the right hand (Fig. 2), tunnel syndromes on both sides in the wrist and elbow joint, limitation of movements in the right shoulder joint.
Rice. 2. Flexion contracture of the right hand of a patient with AL amyloidosis.
Examination of the dentist: skin: multiple petechiae in the supraclavicular areas and along the anterior surface of the neck. Facial skin color is not changed.
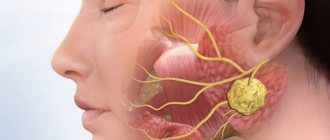
The configuration of the face is changed due to the massive formation of stony density in the submandibular region (20×8 cm) (see Fig. 1). The parotid glands are not palpable. Regional lymph nodes are not palpable. Movement in the temporomandibular joint is free.
The mucous membrane of the oral cavity is almost impossible to examine due to the massive enlargement of the tongue. There is no free saliva. The tongue occupies the entire space between the palate and the floor of the mouth; there are deep imprints of teeth on the lateral surfaces. The tissues of the tongue are stony, the back of the tongue is hyperemic and dry. The patient cannot close her mouth completely. Sleeps half sitting.
In a photograph of the skull in a direct projection, the fan-shaped divergence of the molars and premolars of the upper and lower jaws attracts attention (Fig. 3).
Rice. 3. Multiple destructive foci in the bones of the skull, fan-shaped divergence of teeth in a patient with AL amyloidosis.
Sialometry (stimulated test) was performed - 0 ml of secretion was obtained.
Sialography: there are no signs of parenchymal mumps. The X-ray picture is normal (Fig. 4).
Rice. 4. Sialograms of patient A. Normal variant. a - direct projection; b - lateral projection.
In a biopsy of the minor salivary gland: sialoadenosis with signs of atrophy. Amyloidosis was not detected.
Examination by a rheumatologist: the condition is closer to satisfactory. Asthenic physique. Consciousness is clear. Body temperature is normal. There are flexion contractures of both hands (see Fig. 2), tunnel syndromes on both sides in the wrist and elbow joint. There is no swelling. The cardiovascular and respiratory systems are unremarkable.
Echocardiography revealed diffuse thickening of the myocardium of the “semolina” type. Cardiac amyloidosis is questionable. Ultrasound of the shoulder joints: subluxation of the heads, deformation of the articular surfaces of the shoulder blades on both sides.
Immunological blood test: antinuclear factor was determined at a titer of -1/320 h+sp. An immunochemical study of blood serum and urine confirmed the presence of monoclonal secretion of Bence Jones protein (BJλ).
Considering the absence of AL amyloidosis in the biopsy of the minor salivary gland, the patient underwent a repeat biopsy of the prostate gland and skin. A biopsy of the thyroid gland (Fig. 5) and skin revealed massive deposits of amyloid protein. Based on the results of a myelogram, trephine biopsy of the bone marrow and computed tomography of the skeletal bones (multiple foci of destruction of the skull bones in the thoracic vertebrae, sternum, clavicles, humeral heads and shoulder blades), a combination of two plasmatic dyscrasias was diagnosed: multiple myeloma and AL amyloidosis.
Rice. 5. Amyloid masses (orange-brown) located periductally to the PIJ. Coloring Congo red. ×200.
Thus, by the time of diagnosis, the patient’s clinical manifestations were extensive and almost irreversible. Despite the patient’s repeated visits to various dental institutions and a biopsy of the prostate gland 5 months after the appearance of their enlargement, the diagnosis of the disease was not verified within a year. Therefore, we consider it necessary to familiarize dentists with the algorithm of dental examination for systemic diseases that occur with enlargement of the major salivary glands (MSG), developed at the Research Institute of Rheumatology named after. V.A. Nasonova (see diagram, table).
Diseases of the salivary glands
Go to:
- Maxillofacial Surgery
The salivary glands produce secretions that keep your mouth moist, protect your teeth and mucous membranes, and help you digest food.
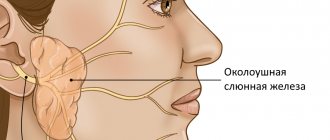
The major salivary glands include the paired parotid, submandibular (submandibular) and sublingual glands. The largest of them are the lunar glands.
Salivary gland problems
Many factors can interfere with the proper functioning of the salivary glands, preventing the production of sufficient secretions and preventing the flow of saliva into the oral cavity.
- Salivary stones (Sialolithiasis)
One of the most common causes of an enlarged gland is the presence of a stone in the gland or in its duct.
There are never too many promotions Read more
Sometimes salivary stones block the ducts, making it difficult for saliva to enter the mouth. Saliva accumulates in the gland, causing pain and swelling.
- Inflammation of the salivary gland (Sialadenitis)
A bacterial infection affects the gland, causing it to become inflamed, swollen, and its ducts blocked.
Sialadenitis is manifested by a painful enlargement of the gland and the appearance of purulent discharge from the ducts of the gland, opening into the oral cavity.
- Viral infections of the salivary glands
Viral infections such as mumps, influenza, Epstein-Barr virus, cytomegalovirus, coxsackievirus, and human immunodeficiency virus (HIV) can also lead to reactive swelling of the salivary glands. Swelling occurs in the parotid glands on both sides. Subsequently, after 48 hours, symptoms typical of a viral infection appear - headache and fever.
- Salivary gland cysts
A cyst can form in the salivary gland as a result of injury, infection, or the presence of a salivary stone. There are also congenital cysts of the parotid glands. The cyst is a slightly protruding round formation, soft in consistency, painless on palpation.
- Tumors of the salivary glands
There are malignant and benign tumors of the salivary glands.
The two main common tumors are pleomorphic adenoma and Warthin's tumor.
Pleomorphic adenoma usually occurs in the parotid glands. The tumor grows slowly and does not cause pain. Pleomorphic adenoma is a benign tumor.
Warthin's tumor is also benign and occurs in the parotid glands. It is usually observed on both sides more often in men.
-10% on all MRI and CT scans in the department on Narodnaya
More details
- Sjögren's syndrome, Mikulicz's disease
Systemic autoimmune diseases, in which the process mainly involves the salivary and lacrimal glands, which leads to dry mouth (xerostomia) and a feeling of sand in the eyes (xerophthalmia). Women get sick more often.
Treatment of diseases of the salivary glands
Treatment of diseases of the salivary glands depends on the cause and nature of the disease. When stones form in the duct, treatment usually begins with removing the stones, prescribing a salivary diet and physiotherapeutic procedures. If these measures do not produce the expected results, surgery may be required to remove the stone or affected gland.
Surgery is usually indicated for malignant and benign neoplasms of the salivary glands.
Other salivary gland problems can be treated with medication.
Bacterial infections can be eliminated with a course of antibiotics. If necessary, bougienage of the gland duct is carried out and massage is prescribed. You can make an appointment with a maxillofacial surgeon by phone or through an online appointment.
Mumps
Vomit
Encephalitis
21826 02 December
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-treatment.
In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. To make a diagnosis and properly prescribe treatment, you should contact your doctor. Mumps: causes, symptoms, diagnosis and treatment methods
Definition
Mumps, or “mumps,” is an acute viral disease accompanied by intoxication (that is, “poisoning” of the body with toxins), fever, enlargement of one or more salivary glands, and often damage to other glandular organs and the central nervous system.
Causes of the disease
The causative agent of the disease is an RNA virus of the genus Paramyxovirus
, family
Paramyxoviridae
. The virus is unstable in the external environment - it quickly dies under the influence of high temperature, ultraviolet rays, and disinfectant solutions, although at low temperatures it can remain viable for up to 1 year.
The source of infection is a sick person. The sick person becomes infectious 1-2 days before the onset of clinical symptoms and secretes the virus during the first 5-7 days of illness.
The virus is transmitted by airborne droplets (when talking, coughing, kissing) and household contact (using shared utensils, toys and other infected objects).
Classification of the disease By type:
1. Typical form:
- uncomplicated (only the salivary glands are affected),
- complicated (other organs and systems are affected),
- isolated:
- glandular form (only mumps is present),
- nervous form (with damage to the central nervous system);
2. Atypical form:
- erased (weak clinical picture of the disease),
- innaparent (asymptomatic).
By severity
(severity criteria are the severity of intoxication and fever, local manifestations, the presence of complications):
- light,
- average,
- heavy.
With the flow:
- smooth,
- unsmooth:
- with complications
- with the addition of a secondary infection,
- with exacerbation of chronic diseases.
Symptoms of mumps
The incubation period varies from several days to a month, but more often it lasts 15-19 days. In children, prodromal phenomena are rarely observed, appearing 1-2 days before the development of a typical picture of the disease in the form of malaise, myalgia (muscle pain), headache, chills, sleep disturbances and appetite.
Mumps begins acutely with fever, intoxication, and pain in the area of the parotid salivary gland.
Mumps of mild severity occurs with subfebrile body temperature (within 37-38°C), absence or mild signs of intoxication, without complications.
With moderate mumps, severe and prolonged fever (38-39.9°C), severe intoxication syndrome (manifested by chills, headache, weakness, pain in the joints and muscles), enlarged salivary glands, and the presence of complications predominate.
Severe mumps is characterized by high and prolonged temperature (40°C or higher for a week or more), pronounced symptoms of intoxication (asthenia, severe weakness, tachycardia, decreased blood pressure, sleep disturbance). The disease is almost always bilateral, and complications are usually multiple. Intoxication and fever have a wave-like character, each new wave is associated with the appearance of another complication.
The first symptoms of mumps are pain in the area of the parotid salivary gland, especially during chewing or talking. By the end of 1-2 days, the parotid salivary gland enlarges and acquires a doughy consistency. With a significant increase in the salivary gland, swelling of the surrounding tissue appears, spreading to the cheek, temporal region and mastoid region. Over the next 2-3 days, other salivary glands (parotid on the other hand, sublingual (sublingual), submandibular (submandibular)) may be involved sequentially or simultaneously in the process, with the addition of soreness under the tongue and in the chin area. The disease is characterized by a positive Filatov's symptom (swelling and pain when pressing on the tragus, mastoid process and in the area of the retromandibular fossa), Murson's symptom (swelling and hyperemia around the external opening of the excretory duct of the parotid gland).
Other organs are often involved in the pathological process.
- Inflammation of the pancreas (pancreatitis) develops on the 4-6th day of illness in 20-40% of cases or even before the enlargement of the parotid salivary glands. Clinically, pancreatitis is manifested by pain in the upper abdomen, nausea, vomiting, and constipation.
- Damage to the gonads in men (orchitis) develops acutely on the 6-8th day of illness, less often at a later date. The lesion is predominantly unilateral, most often on the right side. Orchitis may precede enlargement of the parotid salivary glands (primary orchitis), develop simultaneously with mumps (concomitant orchitis) and be the only manifestation of the disease (autonomous orchitis). Orchitis is accompanied by a repeated rise in temperature, pain in the affected testicle, radiating to the groin and femoral region. The testicle thickens and increases in size within 3-5 days. Symptoms completely disappear after 7-12 days.
- Inflammation of the prostate gland (prostatitis) is manifested by discomfort or pain in the perineum and anus.
- Damage to the ovaries (oophoritis) occurs in girls during puberty. Patients note pain in the iliac region, high fever and intoxication are present.
Diagnosis of mumps
Mumps must be distinguished from purulent inflammatory diseases of the parotid glands, infectious mononucleosis, diphtheria, and peritonsillar abscess.
Laboratory diagnosis of mumps includes:
- general blood analysis;
Anatomy and pathology of the salivary glands. Sialadenitis, sialosis
In the article, the authors consider the normal and pathological anatomy of the salivary glands. Sialadenitis and sialosis are treated. They are trying to consider the macroscopic and microscopic picture of these diseases.
Key words: salivary glands, sialadenitis, sialosis, pathological anatomy, dental diseases, parotid gland, sublingual gland, submandibular gland.
The salivary gland is an important part of the human digestive system. It performs exocrine, endocrine, filtration and excretory functions. The excretory ducts of the glands open into the oral cavity. There are large and small salivary glands.
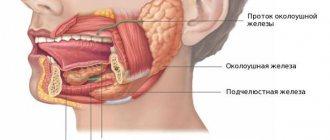
The large salivary glands are located outside the oral cavity and include the parotid, sublingual and submandibular glands. The minor ones are located deep in the mucous membrane and are represented by the labial, buccal, palatine, molar and lingual glands.
Parotid gland, glandula parotidea
It is the largest gland. Located in the mandibular fossa, the excretory duct runs along the outer surface of the masticatory muscle and opens on the mucous membrane of the vestibule of the mouth in the area of the second upper molar [2].
In terms of its structure, it is complex alveolar, serous type, and has a lobular structure. The gland is covered with fascia, which encloses it in a capsule [4].
Submandibular gland, glandula submandibularis
Located in the submandibular space, the excretory duct opens on the sublingual papilla, like the duct of the sublingual gland. In structure it is a complex alveolar-tubular gland of a mixed nature, which also has a lobular structure. The submandibular gland secretes protein-mucosal saliva with a predominance of the protein component [4].
Sublingual gland, glandula sublingualis
It lies on the mylohyoid muscle, directly under the mucous membrane of the floor of the mouth, and has a thin connective tissue capsule. The excretory ducts of some lobules open independently into the oral cavity, and the main duct is located next to the duct of the submandibular gland [5].
The structure is a complex alveolar-tubular salivary gland, producing mixed saliva with a predominance of mucous secretion.
Diseases of the salivary glands can be either primary (independent) or secondary - a manifestation or complication of any systemic disease. Diseases can be caused by the development of infection, tumor, traumatic injury, as well as obstructive, tumor-like or autoimmune damage.
Sialadenitis
Inflammation of the salivary gland is called sialadenitis. Most often, the parotid gland is affected, less often - the submandibular gland, very rarely - the sublingual gland. Sialadenitis can be acute or chronic, and according to the etiology of the disease it can be viral, fungal or bacterial. The following routes of infection are possible: hematogenous, contact, lymphogenous and intraductal from the oral cavity of the body.
Acute sialadenitis
May occur due to exposure to local and general factors. Local factors - any surgical intervention, compression of the excretory ducts by a tumor, traumatic lesions. Common factors are diabetes mellitus, chronic gastrointestinal diseases, immunodeficiencies, cardiovascular diseases [1].
Acute sialadenitis is divided by morphology into gangrenous, serous and diffuse purulent. The salivary gland enlarges in this disease. Purulent sialadenitis is characterized by pronounced neutrophilic infiltration with an abundance of purulent bodies. With serous sialadenitis, swelling, neutrophilic infiltration, and plethora are observed.
Complications of acute sialadenitis include the occurrence of abscesses, sepsis and phlegmon of the neck tissue. Outcome: recovery or transition to chronic [3].
Chronic sialadenitis
Most often secondary, i.e. as a complication of traumatic injuries, infectious diseases, developmental defects. According to the degree of clinical manifestations, active and inactive sialadenitis are distinguished. Chronic sialadenitis often takes on a recurrent nature, so there are two stages: the remission stage and the exacerbation stage.
The salivary glands are enlarged, have a smooth surface and a densely elastic consistency. With exacerbation of chronic sialoadenitis, they acquire a doughy consistency
There are two morphological forms of chronic sialoadenitis: interstitial, ductal (Kussmaul sialodochitis).
Interstitial is characterized by focal or diffuse lymphohistiocytic infiltrates with macrophages, as well as the proliferation of connective tissue with atrophy of the epithelium of aciar structures. The preserved areas of the salivary gland in this case represent hypertrophied acini with hyperplastic cells of the intercalary and striated excretory ducts [3].
With ductal sialadenitis, between the acini and terminal ducts there are diffuse lymphohistiocytic infiltrates with an admixture of polynuclear leukocytes. The ducts are expanded and lined with multirow cubic epithelium. The cells of the epithelial layer of the interlobular excretory ducts are in a state of necrobiosis.
Outcome: with rare relapses, cirrhosis is possible, and with frequent relapses, the formation of large cysts with elements of purulent inflammation.
Full recovery usually does not occur. Preventive measures are aimed at preventing exacerbation of pathological processes and increasing the body's resistance.
Sialosis
It is characterized by hypertrophy of serous acinar cells, which contain mucoid substance, and is non-inflammatory in nature. It is based on dystrophic processes and changes. There is an enlargement of the glands, most often the parotid glands, painless or slightly painful swelling, and hyposalivation. Microscopically: narrowing of small and large ducts, as well as depletion of the gland parenchyma pattern due to hypertrophy and cell hyperplasia. There are three stages: the initial stage, characterized by hypersecretion, the clinically pronounced stage, which is characterized by depletion of secretion, dystrophic changes in the epithelium, and the late stage of lipomatosis and fibrosis [1]. Thus, the outcome is salivary gland lipomatosis.
Treatment is aimed mainly at eliminating the factor contributing to the development of sialosis, dystrophic changes in the salivary glands. In the late stage, there are indications for the use of surgical treatment methods: parotidectomy, extirpation of the excretory ducts of the salivary glands.
Pathology of the salivary glands is not so common, but still occurs, which is why it is important to know the normal and pathological anatomy of the salivary glands for the prevention, detection and treatment of pathological processes that occur in the oral cavity.
Literature:
- Afanasyev V.V., Abdusalamov M.R. Atlas of diseases and injuries of the salivary glands. - M.: VUNMC Roszdrav, 2008. - 192 p.
- Gaivoronsky I.V., Nichiporuk G.I. Anatomy of the digestive system: textbook. ELBI-SPb, 2006.-64 pp..
- Zavyalova M. V. Pathological anatomy of the head and neck: textbook / M. V. Zavyalova, S. V. Vtorushin, I. V. Stepanov; ed. V. M. Perelmuter; rec.: V. A. Shkurupiy, E. L. Kazachkov; Siberian State Medical University (Tomsk). - Electron. text data - Tomsk: Siberian State Medical University, 2013. - 167 p.
- Prives M. G., Lysenko N. K., Bushkovich V. I. Human anatomy. 9th ed. M.: Medicine, 1985. - 672 p. Textbook for students of medical institutes.
- Sapin, M. R. Atlas of human anatomy for dentists: atlas / M. R. Sapin, D. B. Nikityuk, L. M. Litvinenko. - Electron. text data - Moscow: GEOTAR-Media, 2013. - 600 p.
Medical Internet conferences
Features of the development and course of oral diseases in endocrine pathology
Babajanyan S.G.
Scientific supervisor: Ph.D., ass. Kazakova L.N.
GBOU VPO Saratov State Medical University named after. V.I.Razumovsky Ministry of Health of the Russian Federation
Department of Pediatric Dentistry and Orthodontics named after. S.R. Mirotvortseva
All over the world, diseases of the endocrine system in children are increasingly attracting the attention of dentists, since upon examination of the oral cavity the first signs of the disease are revealed - dryness, burning of the oral mucosa, loss of filiform papillae of the tongue, thirst [1].
The endocrine system is a system of endocrine glands located in the central nervous system, various organs and tissues, and is one of the main regulatory systems of the body. The endocrine system exerts its regulatory influence through hormones [2].
Endocrine diseases can be associated with genetically determined anomalies, inflammatory and tumor processes in the body, disorders of the immune system, injuries, circulatory disorders, lesions of various parts of the nervous system, and impaired tissue sensitivity to hormones. The loss of any of the components of hormonal regulation from the general system disrupts the single chain of the body's functional system and leads to the development of various pathological conditions. Pathology of the endocrine system is expressed by diseases and pathological conditions, which are based on hyperfunction, hypofunction and dysfunction of the endocrine glands [3].
Changes in the function of the glands of the internal system lead to endocrine disorders and cause certain changes in the oral cavity.
Diabetes mellitus ranks third after cardiovascular diseases and cancer [4]. In the first months of newborns, this pathology is rare; peak incidence is observed after 5 years of age and during puberty [5]. According to statistics, diabetes mellitus is the most important medical and social problem of humanity due to its high prevalence and chronic course.
Insulin-dependent diabetes mellitus is most common in children. Approximately 2 in 1000 children aged 5 – 18 years suffer from this disease. The development of insulin-dependent diabetes occurs as a result of viral or toxic lesions of the pancreas in children who are genetically predisposed to developing the disease. There is also an assumption about an autoimmune mechanism for the destruction of insulin-producing B cells [6]. According to the literature, diseases of the oral cavity associated with diabetes mellitus are observed in 87% of patients. With this disease, natural changes occur in the tissues of the oral cavity, depending not only on age, but also on the duration of the disease, the degree of metabolic control and the presence of diabetic complications [7.8]. Hyperglycemia and “jumps” in blood glucose levels during the day often lead to suppression of salivation and a feeling of dryness in the oral cavity [9,10,11]. Xerostomia is the first sign of diabetes mellitus in the oral cavity. Saliva is involved not only in the processes of remineralization, but also plays a huge role in maintaining homeostasis in the oral cavity. A decrease in salivation creates favorable conditions for the development of dysbiosis, this manifests itself in the form of an increase in the number of microorganisms, especially hemolytic streptococci and staphylococci [12,13,14] . In patients with diabetes mellitus, rapid and significant deposition of soft plaque and tartar occurs. MJ Campbell explains the presence of a significant amount of dental plaque - a high concentration of glucose in saliva (from 0.44 to 6.33 mg of glucose per 100 ml of saliva, with a norm of 0.24 to 3.33 mg), which promotes the proliferation of microorganisms. According to LW Burket, a decrease in alkaline reserves in diabetes mellitus contributes to the formation of tartar.
The compensated form of diabetes mellitus entails a violation of mineral metabolism, a decrease in the formation and activation of destruction of bone tissue, which affects the condition of the hard tissues of the tooth. When mineral metabolism is disrupted, calcium begins to be washed out of the body, and then fluoride. When there is not enough calcium and fluoride, the enamel becomes fragile. Acid released by bacteria penetrates into it faster, which contributes to the formation of caries; the high rate of its progression is due to the fact that the dentinal tubules are expanded, and this facilitates the spread of the process deeper [15].
Diabetes mellitus affects the condition of periodontal tissues, as shown by a number of reviews and studies [16]. With this pathology, regional hemodynamics are impaired [17]. Vascular disorders in patients with diabetes mellitus develop not only due to spastic changes in blood vessels and capillaries, but also due to changes in the function of the blood itself (increase in the diameter of red blood cells, accumulation of glycated hemoglobin) [18]. During the above processes, the wall of blood vessels thickens, which leads to a slowdown in the supply of nutrients and a decrease in tissue resistance to microorganisms [19].
Considering the hormonal system as a whole, one cannot help but pay attention to the state of the thyroid and parathyroid glands in diabetes mellitus. At the stage of compensation for diabetes mellitus, these glands work in changed conditions, but maintain dynamic constancy. However, in childhood, these glands themselves are not yet fully formed. The final formation of the thyroid and parathyroid glands is achieved by puberty, so there is a high probability of developing an inferior structure.
The thyroid hormone, thyrocalcitonin, has a hypocalcemic effect and inhibits bone resorption [20]. The thyroid gland has a great influence on the process of calcification of enamel and dentin. The formation of thyroid function coincides with the period of differentiation of the primordia of primary teeth, so at the 10th week of embryonic development ameloblasts are formed, and at the 12th week odontoblasts are formed, and at the 16th week the period of dentinogenesis and amelogenesis begins, while in the same period other glands are in a state of development and begin to function only at the 20-26th week of pregnancy [21].
With diffuse toxic goiter, characterized by diffuse hyperplastic changes in the thyroid gland, the body is intoxicated by excessively produced and released thyroid hormones into the blood. The disease is 5 times more common in women and is more likely to occur between 12 and 14 years of age [6]. Patients with toxic goiter experience various changes in the hard tissues of the teeth. The hard tissues of teeth have increased transparency at the cutting edge. On the labial surface there are white chalky spots, the severity of which depends on the duration and severity of the disease. In patients with thyrotoxicosis, dental pulp denticles are more common, according to the literature, almost 3 times [22].
The close functional connection of the salivary glands with the thyroid gland is known. Toxic goiter leads to a change in the physicochemical composition of saliva, while its viscosity decreases, which leads to a decrease in the absorption of organic substances on the surface of the teeth, which weaken the mechanism of protecting the enamel from demineralizing factors.
Hypofunction of the thyroid gland can be either congenital (cretinism) or acquired (juvenile myxedema). Thyroid hormone deficiency is most often secondary to primary thyroid disease and is sometimes associated with dysfunction of the hypothalamus or pituitary gland. Cretinism is rare. Juvenile myxedema can develop for many reasons, such as thyroidectomy, thyroid radiation, autoimmune diseases, infection, or drug treatment [6].
Gratkowska N.; Gilbert-Dreyfus A.; Alexandre C.L.; Hayden P; Weyers H., note that with hypothyroidism there is a delay in the eruption of baby teeth by 1-2 years. The replacement of baby teeth with permanent teeth is usually delayed by an average of 2-3 years.
Hypothyroidism leads to changes in the microelement composition of dental hard tissues [21]. Histologically, degenerative changes in the structure of enamel and dentin are revealed, osteodentin is formed, enamel and dentinogenesis slows down, and late mineralization of tooth buds. With hypofunction of the thyroid gland, the shape of the crown of the teeth changes; the incisors can be round in cross section, with teeth on the cutting edge. Fangs and molars can be in the form of incisors, the crowns are shortened. Sometimes they can be doubled (fused primordia) [23].
In hypothyroidism, vascular congestion and perivascular hemorrhages are detected, individual epithelial cells with dystrophic cell changes appear in the stratified squamous epithelium, collagen fibers are saturated with edematous fluid, swell and homogenize, swelling of the main substance of the connective tissue with areas of metachromes is noted [24].
The parathyroid glands produce substances of a protein nature - parathyroid hormone, or parathyroid hormone, which takes part in the regulation of mineral, especially calcium and phosphorus metabolism, affects the processes of calcification and decalcification in the bones. Parathyroid hormone maintains a constant calcium level in the blood serum (2.2 - 2.5 mmol/l), circulating in the bloodstream in the form of complexes with proteins, usually with inactive ones. When there is a lack of parathyroid hormone in the body, the metabolism of phosphorus and calcium is disrupted. Vitamin D plays an important role in maintaining normal levels of calcium in the blood, which affects the intake of calcium from the intestines into the body and stimulates the deposition of calcium in bone tissue.
With hypoparathyroidism, protein and mineral metabolism is disrupted and, as a consequence, calcification of enamel and dentin is impaired. Opaque white spots may appear in mature teeth. Histologically, the picture of the enamel is characteristic of hypoplasia: underdevelopment, deformed prisms with bends, defects and folds on the surface of the enamel, wide and numerous interglobular non-calcified zones and cavities in the dentin, the odontoblast layer is scanty, the pulp is normal, denticles are often found [23]. Hypofunction of the parathyroid glands significantly slows down teething.
Hyperparathyroidism is a disease caused by hyperfunction of the parathyroid glands and accompanied by changes in the bones, calcium deposition in various organs and tissues due to impaired phosphorus-calcium metabolism. Excessive production of parathyroid hormone can be expressed in a primary defect of the gland (adenoma, hyperplasia, hypertrophy) or secondary as a compensatory phenomenon that corrects the state of hypocalcemia caused by rickets or chronic kidney disease [6]. Primary hyperparathyroidism is a very rare form of endocrine disease in childhood.
Analysis of the above material shows the close relationship of the endocrine system with all structures of the oral cavity at all stages of their development, starting from the moment of the formation of all tissues. Early diagnosis of these diseases in the oral cavity will make it possible to comprehensively plan the prevention and treatment of developing pathologies in the oral cavity. If there is endocrine pathology in children, the following recommendations must be followed. Routine examinations and sanitation of the oral cavity in children with endocrine pathology must be carried out depending on the nature and form of the underlying disease, taking into account the activity of the carious process, but at least 3 times a year. It is mandatory to carry out a set of therapeutic and preventive measures aimed at increasing the resistance of hard dental tissues, restoring the functional activity of oral fluid, improving trophic processes and increasing the resistance of the oral mucosa.
Discussion
The diagnosis of AL amyloidosis is challenging for physicians around the world due to the variety of clinical manifestations and vague symptoms [9, 11–13]. A significant increase in PVS occurs in autoimmune, granulomatous, lymphoproliferative and IgG4-related diseases (see table), but the development of macroglossia in combination with a massive increase in PV is highly specific, suggesting the presence of AL amyloidosis [10, 14]. A biopsy of the prostate gland was performed on the patient 5 months after the onset of clinical manifestations, but the lack of Congo red staining of the biopsy specimen did not allow diagnosing the deposition of amyloid masses in the salivary gland. A biopsy of the affected organs (heart, kidneys, liver, lungs, parathyroid gland, etc.), for histological verification of AL amyloidosis, is performed in the absence of a positive result in alternative sites (minor salivary glands, gums, subcutaneous fat aspirate, rectum) [9, 10, 14]. In our case, a biopsy of the minor salivary gland and gum gave a negative result, but a biopsy of the prostate gland and skin confirmed the presence of AL amyloidosis.
Symptoms of damage to the salivary glands in systemic diseases occurring with an increase in BSG Note. LPD - lymphoproliferative diseases; PP - parenchymal parotitis; CS - chronic sialadenitis; focus >1—focus of lymphoid infiltration of more than 50 cells; LHI—lymphohistiocytic infiltrate; LEP—lymphoepithelial lesion; MSG - minor salivary glands; BSG - large salivary glands.
Scheme. Algorithm for examining patients with enlarged major salivary glands during a dental appointment. MSG - minor salivary glands; BSG - large salivary glands. Note. LPD - lymphoproliferative disease; IHC - immunohistochemical staining of tissues.
It should be noted that immunochemical testing of blood serum and urine should be performed before biopsy. The presence of low levels of monoclonal secretion or light chains of monoclonal Ig in serum or urine is mandatory for AL amyloidosis [9–14], while the absence of these signs suggests manifestations of secondary AA amyloidosis [5]. Considering the variety of diagnoses that were made to the patient during the year, we should focus on the algorithm for examining a patient who came to the dental clinic with enlarged salivary glands (see diagram). Infectious parotitis, salivary stone disease and solid tumors of the salivary glands are well covered in textbooks on surgical dentistry, while diseases with systemic involvement of the major salivary glands receive little attention. The picture of chronic sialadenitis can be present in biopsy samples of the salivary glands in all systemic diseases (see table). Its severity depends on the duration and activity of the pathological process, and without additional research methods it does not allow diagnosing the pathology of the salivary glands. An important diagnostic method is sialographic examination. Parenchymal sialadenitis is a radiological sign. Its presence is a diagnostic sign of Sjogren's disease and primary MALT lymphomas of the major salivary glands [7]. The patient was diagnosed with parenchymal sialadenitis without a sialographic examination. Functional diagnostic methods and MRI can be used to determine the degree of enlargement of the salivary glands and intraglandular lymph nodes, to partially exclude the presence of salivary stones and solid tumors and, in some cases, to suggest the presence of parenchymal parotitis based on multiple cystic changes in them. These methods cannot make a diagnosis, which requires morphological verification. According to the modern classification, Mikulicz's disease is classified as a group of IgG4-associated lesions. Determination of the levels of the IgG4 subclass of IgG in the serum and immunohistochemical examination of the biopsy specimen to determine the synthesis of IgG4 by more than 40% of plasma cells is necessary to make a diagnosis of IgG4-related sialadenitis [6, 7].
The use of radiation therapy for systemic diseases involving the salivary glands (Sjögren's disease/syndrome), granulomatous and IgG4-related sialadenitis, etc.) is a serious mistake, as it increases the manifestations of xerostomia and stimulates the development of lymphomas in these diseases [15] . Using an algorithm for examining patients with systemic lesions of the salivary glands, developed during the examination of 298 patients with a significant increase in the major salivary glands at the Research Institute of Rheumatology named after. V.A. Nasonova, can reduce diagnostic errors in dental practice when conducting differential diagnostics.