Inflammation of the salivary glands is called sialadenitis . Any salivary gland can become inflamed. Most often, an inflammatory process is detected in the parotid glands (parotitis); the sublingual and submandibular glands become inflamed much less often. Usually the disease occurs secondary, as a complication or symptom of another disease, but the primary form of the disease also occurs. The inflammatory process can be either unilateral or bilateral; multiple lesions of the salivary glands are rare. The nature of the disease can be either viral or bacterial.
Types of inflammation
Depending on the infectious agency, two types of sialadenitis are distinguished. This:
- viral;
- bacterial.
Viral sialadenitis
The disease is formed as a result of the penetration of the mumps virus into the human body. The disease is known as "mumps". Transmission is carried out by airborne droplets. After entering the body, the virus penetrates the tissue of the parotid salivary gland, causing inflammation. In the generalized form of mumps in men, the testicles are affected, which can subsequently cause infertility.
Important! In some cases, viral sialadenitis develops against the background of cytomegalovirus infection.
Bacterial (nonspecific) sialadenitis
Formed as a result of infection through the oral cavity. Provoking factors may be:
- Poor oral hygiene.
- Reactive obturation. The resulting narrowing of the duct causes a reduced volume of saliva secreted. The accumulated secretion becomes a convenient environment for the proliferation of pathogenic microflora, which is constantly present in the oral cavity.
- Mechanical obturation. Develops as a result of blocking the lumen of the duct. Pathogens actively multiply in the collected saliva, causing inflammation.
The bacterial form of sialadenitis develops as a result of infection of the ducts of the oral cavity
The second option for infection is transmission through the blood. The cause may be severe infectious pathologies, in particular scarlet fever. The third way of infection of the salivary gland is through the lymph. The cause is inflammatory pathologies of the face, oral mucosa and pharynx. To be honest, periodontitis, furunculosis or tonsillitis.
The chronic form of sialadenitis develops as an independent disease. The reasons may lie at the genetic level. Sometimes inflammation is a response to an autoimmune pathology or some general disease. Quite often, a chronic form of inflammation is recorded in the category of elderly patients, which is due to a deterioration in the blood supply to the organ.
Symptoms
With mumps, the parotid glands are affected. The problem is manifested by the following characteristic symptoms:
- deterioration of general health;
- swelling of neck tissues;
- pain when pressing on areas of inflammation;
- discomfort during conversation and eating;
- headaches of varying intensity;
- dry throat.
Symptoms of inflammation of the sublingual salivary gland and its treatment
If the pathological process spreads to the sublingual and parotid glands, then the symptoms of blockage are supplemented by:
- increased temperature;
- intoxication of the body;
- bad breath;
- severe pain when opening the mouth;
- sensation of a foreign body under the tongue.
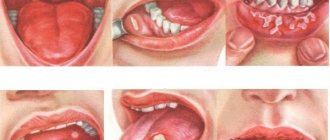
Depending on the form of the course and symptoms, sialadenitis is also divided into serous, purulent and gangrenous. The first form of pathology is characterized by: swelling of the salivary gland; deformation of the earlobe; increase in temperature, release of serous fluid when pressing on the inflamed structures, obstruction of the duct.
With the gangrenous form of the disease, it becomes difficult for a person to sleep at night due to pain. There is also a thickening of the affected structure, spreading of swelling to the tissues of the ear, neck and cheeks. The skin over the problem area turns red.
The advanced form of sialadenitis is gangrenous. It is characterized by a rapid increase in pathological symptoms, death of soft tissues, and blood infection. Untimely medical care can lead to the death of the patient.
Symptoms of inflammation of the salivary glands
The general symptoms of the disease are as follows:
- dryness of the oral mucosa due to lack of salivary fluid;
- shooting pains;
- pain accompanying chewing, swallowing food and opening the mouth;
- swelling and hyperemia of the skin in the projection of the salivary gland;
- unpleasant taste of saliva;
- possible appearance of purulent contents;
- painful formation in the area of inflammation;
- a feeling of fullness, which indicates the accumulation of pus;
- increased general body temperature and weakness.
The most severe inflammation of the parotid salivary gland is caused by the mumps virus entering the body.
Mumps - mumps - is especially dangerous, since other glands of the body, for example, the pancreas, can be involved in the pathological process. Symptoms of inflammation include: acute onset with an increase in body temperature to 39–40 degrees, swelling in the area of the parotid salivary gland, pain that intensifies during chewing.
Acute sialadenitis of the parotid salivary gland occurs in several stages, each of which is accompanied by certain symptoms.
- Serous sialadenitis. It is typically characterized by dryness of the oral mucosa, soreness in the ear area, and the development of slight swelling. The lobe is slightly raised upward. Increased pain is recorded during eating. The increase in body temperature is slight.
- Purulent stage. Characterized by increased pain. There is an increase in body temperature above 38 degrees, increased swelling, and restriction when opening the mouth. When pressing on the area of inflammation, purulent masses flow. The gland is dense and painful.
- Gangrenous inflammation. An abscess forms over the inflamed gland, serving as an outlet for dead tissue.
In the absence of adequate drug therapy, death due to the development of sepsis cannot be ruled out. The cause may be internal bleeding caused by the melting of the walls of large blood vessels in the neck.
Symptoms of chronic inflammation depend on the current form of the disease:
Damage to the salivary glands
- Chronic interstitial sialadenitis. Most often it develops in the parotid glands (about 85%). It is diagnosed in most cases in elderly patients. It remains asymptomatic for a long time. The development of the clinical picture is due to a deterioration in the condition caused by a narrowing of the ductal lumen. A sign of exacerbation is the appearance of a feeling of dry mouth and an increase in the size of the gland. It becomes painful when touched.
- Chronic parenchymal sialadenitis. Mostly women suffer from it. In the initial stage of development, when pressure is applied to the gland, a significant volume of salty-tasting liquid is released. Later, a feeling of heaviness and compaction develops. It is possible that saliva may be released with admixtures of pus and mucous lumps. In the later stages, the gland is painless, lumpy, and discharge of pus is observed.
- Sialodochitis is inflammation of the ducts. A typical symptom is increased production of salivary fluid during eating and talking, as well as the formation of congestion in the corners of the mouth. During the period of exacerbation of the pathology, impurities of pus are present in the saliva, the gland becomes swollen and dense.
Chronic mumps
Acute mumps rarely becomes chronic, so chronic mumps often occurs as a primary disease.
Chronic mumps are classified into 2 groups: parenchymal and interstitial.
Chronic parenchymal parotitis
Chronic parenchymal parotitis is often asymptomatic. However, the clinic is varied. Patients may complain of swelling, pain in the gland area, and a taste of pus in the mouth. The disease lasts a long time, periodically exacerbating. Most often one gland is affected.
Objectively we can see a swelling of the gland with clear contours. Palpation is painless, the gland is dense, the surface is lumpy. When massaging the gland - saliva with pus.
Diagnostics
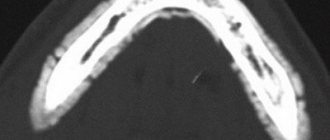
For diagnosis, a contrast sialogram is performed. On the sialogram you can see deformation and/or necrosis of the ducts of 2-4 orders and the parenchyma of the gland - in the image there are cavities filled with a contrast agent. As the disease progresses, the cavities merge, areas of necrosis increase until the glandular tissue is replaced by fibrous tissue.
The radiosialographic method allows us to identify the stage of the disease. At the initial stage, there is a rapid accumulation of radioactivity. In the stage of pronounced signs - slow accumulation. In the late stage, radioactivity is low.
The cytological method for diagnosing punctate and gland secretions is also used.
Treatment of chronic parenchymal parotitis
Treatment of chronic parenchymal parotitis is difficult due to the inability of dead gland tissue to regenerate. Therefore, the dentist’s task is to relieve the disease.
The gland is stimulated with ocular probes and washed every day with antibiotic solutions and massaged, freeing it from solution and pus until clear saliva appears. The ducts can also be washed with chymotrypsin, a solution of potassium iodide. Novocaine blockades and radiotherapy are indicated.
With frequent relapses, extinguishing the function of the gland is carried out by three times instillation of ethyl alcohol with increasing concentrations of 60-80-96.
Surgical treatment: parotidectomy, extirpation of the parotid duct + denervation of the auriculotemporal nerve.
Diagnostics
Acute sialadenitis is diagnosed by examining the patient and collecting existing complaints. The sialography procedure is used in rare cases, since the introduction of a contrast agent causes increased pain.
Differential diagnosis is necessary for the correct choice of treatment method
To confirm chronic sialoadenitis of the parotid salivary gland, contrast sialography is used. It allows you to determine the current form of the pathology. Narrowing of the lumen of the duct is typical for the interstitial form of inflammation. In this case, the volume of contrast agent penetrated into the gland tissue does not exceed 0.8 ml.
A healthy organ holds approximately 2–3 ml. In the parenchymal format of sialadenitis, numerous cavities with a diameter of up to 10 mm are recorded. The tissues of the gland and the ducts themselves are not determined. The capacity of the cavities is 6...8 ml of contrast.
Our doctors who will solve your vision problems:
Fomenko Natalia Ivanovna
Chief physician of the clinic, ophthalmologist of the highest category, ophthalmic surgeon. Surgical treatment of cataracts, glaucoma and other eye diseases.
Yakovleva Yulia Valerievna Refractive surgeon, specialist in laser vision correction (LASIK, Femto-LASIK) for myopia, farsightedness and astigmatism.
You can find out the cost of a particular procedure or make an appointment at the Moscow Eye Clinic by calling in Moscow 8 (499) 322-36-36 (daily from 9:00 to 21:00) or using the ONLINE REGISTRATION FORM.
Treatment of the disease
Treatment of sialadenitis should be carried out by a specialized specialist. Incorrectly selected therapy can cause complications. Uncomplicated forms of inflammation are treated on an outpatient basis (at home). The patient will be advised to:
- compliance with bed rest;
- gentle diet - food should be crushed, which reduces pain when swallowing and chewing;
- Drinking plenty of fluids helps reduce the symptoms of intoxication.
Local treatment gives excellent results. Any dry bandages with a warming effect can be applied to the area of the inflamed parotid salivary gland. Compresses based on alcohol and camphor oil help well. In addition, the patient will be recommended to visit a physiotherapy office. The most commonly prescribed procedures are UHF and Sollux.
To ensure the outflow of saliva from the inflamed gland, artificial stimulation is necessary. Any foods with a sour taste, for example, lemon slices, cranberries, sauerkraut, help with this. The body, in response to irritation of taste buds, automatically increases the production of saliva.
In order to activate the process of salivation, you can use medications, in particular, a solution of pilocarpine hydrochloride. At what point the patient should stimulate the secretion of saliva will be decided by the attending physician, based on the current symptoms.
Important! Stimulating the secretion of saliva helps to avoid stagnation and promotes the removal of dead tissue cells from the inflamed gland.
When the body temperature rises and the pain accompanying sialadenitis is relieved, the patient is allowed to take drugs from the NSAID group - Analgin, Pentalgin, Baralgin, Ibuprofen and others. The drugs have analgesic, anti-inflammatory and antipyretic effects.
In the absence of a therapeutic result and a deterioration in general health - there are no improvements within 3 days - or signs of suppuration of the gland appear, the patient is prescribed antibiotics.
If necessary, surgical therapy is performed: opening and draining the inflamed gland, in the presence of a significant volume of purulent masses. Antibacterial drugs are injected directly into the site of inflammation.
If suppuration develops, the patient is recommended to undergo surgical treatment - opening and drainage of the gland
Treatment of inflammation of the parotid salivary gland is a long and complex process. In case of exacerbation, the patient is prescribed drugs from the group of antibiotics and medications that stimulate the production and discharge of saliva.
X-ray therapy shows a good therapeutic result for the chronic form of sialadenitis. When diagnosing stones in the ducts of the gland - the calculous form of sialadenitis - surgical treatment is prescribed.
The structure of the lacrimal gland
The gland that synthesizes tear fluid consists of two parts: lower (palpebral, orbital) and upper (orbital, secular). These parts are separated by a muscular tendon responsible for raising the upper eyelid.
The orbital part is located in the upper outer region of the orbit. 3-5 excretory tubules emerge from it, flowing into the upper fornix of the conjunctiva. The palpebral part (its smaller size) is localized slightly lower, above the conjunctiva. The excretory ducts open into the ducts of the orbital part or into the conjunctival sac.
The blood supply to the glands is carried out by the ophthalmic artery, and innervation by the trigeminal and facial nerves, as well as fibers of the cervical plexus. Nerve impulses enter the lacrimal center located in the medulla oblongata.
Prevention of the development of sialadenitis
There is no specific prevention - the introduction of a specialized vaccine - for sialadenitis. The exception is mumps. Vaccination is carried out with a three-component drug that is effective against three diseases at once - mumps, measles and rubella. All children aged 1.5 years are vaccinated. Lasting immunity is developed in approximately 96% of vaccinated children.
Nonspecific prevention is as follows:
- regular oral hygiene;
- sanitization of all foci of inflammation in the mouth;
- prevention of saliva stagnation;
- rinsing the mouth during infectious pathologies.
Inflammation of the parotid salivary gland is treated by a dentist. If there are signs of mumps development, the child should be shown to a pediatrician. In this case, adult patients turn to a therapist.
results
If tumor formations are detected during an ultrasound, doctors refer the patient to an MRI of the soft tissues of the neck with contrast as an additional examination.
Sometimes, to establish the nature of the tumor, puncture, biopsy and histology are also required. All these procedures will help determine the nature of the tumor - whether it is malignant or benign. Material can also be collected during a biopsy or puncture under ultrasound guidance. Author: Telegina Natalya Dmitrievna
Therapist with 25 years of experience
>
What are tears for?
With the help of tears, you can not only express your emotional state, first of all, we need them to protect our eyes. A thin layer of tear film covers the surface of the cornea and makes it perfectly transparent and smooth, protecting the eyes from drying out.
At the heart of tears is an antibacterial enzyme - lysozyme , which helps cleanse the conjunctival sac of small foreign bodies and microorganisms.
In normal conditions, a small amount of tears is required to moisturize the eye - 0.4-1 ml per day; it is produced by additional conjunctival glands. Large lacrimal glands begin to work when additional irritants appear: severe pain, emotional stress, foreign body contact with the conjunctiva or cornea. And also in too bright light, exposure to smoke and toxic substances.