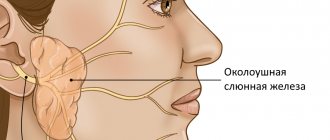
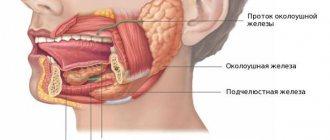
Salivary gland adenoma is a benign neoplasm formed from glandular epithelial cells. Tumors of the parotid salivary gland are most often diagnosed. This can be either a single formation or including several nodes.
Pathology can develop in both men and women. But in the latter it is detected somewhat more often. According to statistics, adenoma of the parotid salivary gland occurs in approximately 2% of all diagnosed cases.
Most often, the tumor forms in people aged 50–70 years. It belongs to benign formations, has clear boundaries, oval or regular round shape. Bilateral involvement is rare.
Causes of pathology
Doctors do not know the true causes of the disease. But several factors have been identified that can become an indirect circumstance of its development.
These include:
- direct injury to the ear or existing inflammatory processes - mumps, sialadenitis;
- predisposition at the genetic level - doctors have put forward the theory that a mutating gene can be inherited;
- penetration into the body of pathogenic microorganisms that can provoke compaction of glandular tissues;
- hormonal disorders can cause changes in the structure of healthy tissues, adjusting their qualitative composition;
- the influence of negative external factors - high-dose multiple irradiation, frequent radiography of the brain;
- smoking - nicotine tars disrupt the processes of saliva production, causing increased dryness of the oral mucosa;
- poor nutrition - as a result of a deficiency of substances necessary for the body, a disruption occurs in the process of producing salivary secretions;
- occupational diseases - quite often a salivary gland adenoma is detected in workers of metallurgical, chemical and woodworking enterprises. Its development is due to the toxic effects of industrial waste.
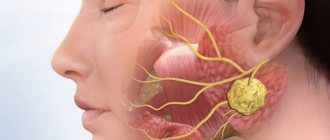
This is what a benign tumor of the salivary gland looks like; the reasons for the mutation of glandular tissue cells are not fully known to doctors
There is also an assumption that the cause of the pathology is the regular use of mobile gadgets.
Polyp in the ear
Benign polyps of the ear include polyps.
These are neoplasms that arise as a result of the proliferation of granulation tissue. The polyp may be located in the external auditory canal or middle ear. Neoplasms localized in the ears can spread to other parts of the skull. Most often, a polyp is a complication of a chronic inflammatory process in the ear. At the site of chronic inflammation of the mucous membrane, a gradual proliferation of tissue occurs, replacing normal tissue with connective tissue.” into the external auditory canal through the perforation of the eardrum.
A polyp in the ear is manifested by the following symptoms:
- Suppuration, sometimes mixed with blood (stopping the flow of pus can be caused by blockage of the ear canal by a polyp);
- Itching, noise and pain in the ear;
- A feeling of constriction, the presence of a foreign body in the ear cavity;
- Decreased or loss of hearing;
- Headaches.
In the absence of adequate treatment, a polyp caused by an infection in the ear often becomes the cause of chronic otitis media, supports the inflammatory process and prevents the penetration of drugs to the site of infection. The growth of the polyp leads to blockage of the ear canal and deafness. Under certain conditions, there is a risk of its degeneration into a malignant tumor.
For polyps of small size, in some cases, otolaryngologists carry out conservative treatment with creams containing glucocorticoids and antibacterial drops. If the disease is fungal in nature, antifungal drugs are used. The main treatment for a polyp in the ear is surgery.
The polyp is cut off on an outpatient basis with a special loop or using another instrument: a curette, an ear conchotome. Radical surgery is performed in a hospital. The operation is performed if the fistula is localized in the semicircular canal. An alternative treatment option is laser removal of polyps.
Classification of the disease
There are several types of adenoma.
Polymorphic (pleomorphic)
The tumor slowly increases in size, but if left untreated it can reach a significant volume. Defined as a dense formation with a bumpy surface. Feature – there is a possibility of degeneration.
Basal cell
Formed from basaloid cells. In most cases it is represented by several nodes. The risk of degeneration is minimal.
Greasy
Small in volume education. It is asymptomatic. It can only be removed surgically. Does not cause complications.
Canalicular
It is distinguished by a thin beam structure. Outwardly it resembles small beads. It is formed from epithelial cells and is diagnosed in old age. Has clearly visible boundaries.
Adenolymphoma
Originates from cells of lymphatic tissue. It grows slowly. Location: behind the ear.
Monomorphic
Occurs only from cells of glandular tissues.
To identify the type of adenoma, a complete diagnosis is necessary. It is impossible to determine the type of tumor visually.
Complications in the presence of serrated adenoma
The main danger of serrated adenomas is the possibility of their malignant transformation into cancer. Until a few decades ago, it was believed that colorectal malignancies develop only from adenomatous polyps. Accordingly, it was recommended to simply observe villous neoplasms. But later it turned out that these tumors can also degenerate into cancer, and have their own, unique path of carcinogenesis. The larger the size of the polyp and the longer it exists, the higher the risks of malignant transformation. The most dangerous in this regard are large, long-existing neoplasms on a wide base.
Symptoms and signs
The most common type is pleomorphic adenoma. Pathology can develop over a long period of time without making itself known.
When examining a patient, a specialist will be able to determine the presence of an adenoma capsule even before the appearance of specific symptoms.
The disease manifests itself with certain symptoms, depending on the location of the tumor. This may include pain, which manifests itself when the formation reaches a significant size, damage to the facial nerve, or clearly visible visual asymmetry of the face.
Poor mobility of the facial muscles on the affected side also occurs. If the tumor is located deep in the tissue, then swallowing disorders occur. A person's speech may also change.
A tumor can be identified by palpation at the beginning of its formation. It will feel like a hard tumor and stand out against the background of healthy tissue. Adenolymphoma and the polymorphic form can develop in the form of numerous nodes and be combined, for example, with an adenoma of the submandibular salivary gland.
In rare cases, an initially benign formation degenerates. The process is accompanied by the development of the following symptoms:
- formation of a clearer boundary;
- expressiveness of the structure;
- rapid increase in capsule volume;
- detection of metastases in local lymph nodes.
If one of the signs is detected, urgent medical advice should be obtained.
Osteoma in the ear
Osteoma in the ear (exostosis, osteophyte) develops mainly from the compact layer of the posterior wall of the bony part of the external auditory canal. Much less often, neoplasms are found on the lower and upper walls of this section. Endophytic osteomas penetrate into the mastoid process. Osteoma is a benign tumor that grows rather slowly.
Osteoma has the appearance of a round formation, which is covered with a skin layer, very dense when palpated with a Vojacek probe. It is treated surgically. The operation is performed after the tumor has grown to medium size. In this case, removing the tumor is technically as convenient as possible. If the tumor is small, there is a risk of not completely removing the pathological tissue. If the osteoma is large, it is possible to capture a significant part of the healthy bone tissue during surgery. This will cause a large bone defect.
Diagnostics
During the initial examination, the doctor performs palpation (palpation) of the affected area. And only after that he prescribes an examination. Diagnosis of the disease includes the following laboratory and instrumental studies:
- Blood analysis. Necessary to obtain information about the general condition of the body;
- CT scan. Helps obtain a visual image of the tumor and its internal structures;
- Sialography. X-ray examination using contrast. Allows you to determine the shape and current size of the adenoma;
- X-ray of the skull. Detection of cranial deformation indirectly indicates the presence of a tumor;
- Ultrasound examination. Allows you to visualize the compaction, clarify the location of its localization, as well as the degree of germination into the surrounding healthy tissue;
- Puncture. Taking the liquid contents of the capsule for further study. Necessary to determine the structure of the adenoma;
- Biopsy. Sampling of tumor tissue to determine the type of tumor;
- Cytology. Used to study cell formation.
The ultrasound image clearly shows a nodular neoplasm in the area of the salivary gland
Based on the results obtained, a decision is made on the type of treatment.
Benign tumors of the ear
Benign tumors of the middle ear include hemangioma and various neurogenic neoplasms. Hemangiomas of the middle ear are manifested by the following symptoms:
- Decreased hearing;
- Ear congestion;
- Feeling of noise.
Often the first symptom of the disease is a slowly occurring paralysis of the facial muscles on the side where the hemangioma is located. For middle ear hemangioma, otolaryngologists usually perform abdominal surgery or widely remove the mastoid process.
Chemodectoma of the middle ear develops from glomus bodies, which are normally located at the bottom of the tympanic cavity, on the dome of the bulb of the internal jugular vein and in the temporal bone. They differ in structure from glomus bodies, which are located in other areas. Depending on the histological structure and the ratio of cell accumulations, there are 3 types of glomus tumors: adenoid-like, alveolar and angioma-like. According to the clinical course, limited and widespread forms of chemodectoma are distinguished.
Diagnosis of chemodectoma is carried out using radiography of the jugular fossa, pyramid of the temporal bone, attic-antral region, mastoid process. X-ray examination includes radiography of the temporal bone in three main projections and tomography in direct and lateral projections.
Chemodect treatment is surgical. Small tumors that do not destroy the eardrum are removed or exposed to ultra-low temperatures. Tumors that have spread to the external auditory canal, mastoid process, or antrum are also subject to surgical treatment. Otolaryngologists perform operations of varying scope - from tympanotomy to extended radical surgical interventions on the ear. Sometimes cryotherapy is used. For tumors that destroy the pyramid and spread into the cranial cavity, external gamma irradiation is performed, which often causes growth arrest or a decrease in chemodectoma.
Treatment of salivary gland adenoma
If an acute form is detected, drug therapy is prescribed. It includes drugs from the category of antibiotics and painkillers. Additionally, it is recommended to take medications that stimulate saliva production. To prevent the development of complications, anti-inflammatory drugs are prescribed.
In addition, physical procedures are prescribed: electrophoresis, laser treatment, UHF therapy. But most often, experts are inclined to a radical method of treatment - removal of the tumor - in order to minimize the risk of relapse of the pathology.
How is the operation performed? The procedure includes several stages:
- An incision is made in the area where the tumor is located.
- After opening the adenoma capsule, it is dissected.
- Next, the capsule is peeled off, and its contents are transferred for histological examination.
- The surgeon then carefully sutures the emptied capsule to prevent the formation of a salivary fistula. The technique of layer-by-layer suturing is used.
Treatment of salivary gland adenoma in most cases involves surgical desquamation of the capsule.
During the operation, the external cavity incision is made in such a way that when the process of malignancy is identified, the surgeon has the opportunity to open the cervical area more deeply.
Complications after tumor removal occur, but are relatively rare. This may include paralysis of the facial nerve, disturbances in facial expressions, and the formation of a fistula. They are usually caused by insufficient qualifications and experience of the operating surgeon. Relapses of the disease are possible, but are uncommon.
Lipoma and atheroma behind the ear
The area of skin around the ear contains a huge number of sebaceous glands. For this reason, lipomas and atheromas often form behind the ear. Lipomas that form behind the ear grow slowly and are often not cancerous. They are a soft-elastic formation with a smooth surface, surrounded by a capsule. The lipoma in the photo looks like a wen.
Atheroma is a cavity formation filled with sebum. Formed due to blockage of the sebaceous glands. Atheromas occur for the following reasons:
- Disorders of fat or carbohydrate metabolism;
- Genetic predisposition to increased oily skin;
- Hormonal imbalances and diseases of the endocrine system;
- Hyperhidrosis is a disease associated with excessive sweating;
- Failure to comply with personal hygiene rules.
Atheroma is a rounded formation protruding above the surface of the skin, which can reach up to 4.5 cm in diameter. When the tumor becomes infected or inflammatory reactions occur, the following symptoms occur:
- Pain behind the ear;
- Redness of the skin;
- Burning and itching;
- Fluctuation is a symptom that indicates the presence of fluid in a cavity formation.
When pressure is applied to the walls of the atheroma or they are damaged, the viscous mass contained inside comes out to the surface of the skin. It has a white color and an unpleasant odor. When atheroma suppurates, the contents have a green-yellow tint. Lipomas and atheromas behind the ear are removed surgically. Modern treatment methods are used - laser or radio wave removal.
Salivary gland adenoma is a benign formation that appears in the glandular epithelium of the salivary glands. The salivary glands are parotid, submandibular, and sublingual. The most common occurrence of tumors is on the parotid gland. If the components of such a tumor are benign, then it is an adenoma of the parotid salivary gland.
Disease prognosis
The prognosis for salivary gland adenoma is quite optimistic. Especially if the process of rebirth has not yet begun. High-quality treatment prolongs a person’s life by 10–15 years.
If the problem is ignored and a benign neoplasm transforms into a malignant one, the five-year survival limit passes (depending on the stage of cancer):
- Stage 1 – approximately 80% of operated patients;
- Stage 2 – no more than 60%;
- Stage 3 – only 42%;
- Stage 4 – less than 25% of all diagnosed cases.
Timely diagnosed pathology and treatment allow a person to lead a normal lifestyle
If left untreated, death occurs within 1–3 years after the adenoma turns into cancer. There is no prevention of the disease as such. Doctors give only general recommendations - maintaining a healthy lifestyle and a balanced diet, including substances necessary for a person.
Glomus tumor of the middle ear
Tympanic paraganglioma (glomus tumor of the middle ear) develops from glomus bodies, which are located on the medial wall or roof of the tympanic cavity, jugular - on the bulb of the jugular vein. Paraganglioma is a benign neoplasm, but mature forms of the tumor have infiltrating and locally destructive growth.
Due to the impossibility of total removal, a glomus tumor of the middle ear can pathologically spread to vital structures of the body (brain stem, internal carotid artery).
Patients complain of a “pulsating” noise in the ear. During an objective examination behind the eardrum, the doctor sees a pulsating red mass. As the tumor grows, the following symptoms occur:
- Hearing impairment;
- Facial asymmetry;
- Dysphonia (speech disorder);
- Dysphagia (swallowing disorder).
If the glomus tumor of the middle ear is widespread, angiography is mandatory. The study is necessary to confirm the vascular nature of the neoplasm, determine its size, location and sources of blood supply.
This plays a role in the possibility of embolization, a minimally invasive procedure that is an alternative to surgery. The procedure is aimed at preventing blood supply to the damaged area, which helps to reduce the size of the tumor and achieve a good effect with further surgical removal of the identified tumor.
Treatment consists of surgical removal of the glomus tumor of the middle ear. Total surgery is performed in the presence of a glomus tumor that does not spread beyond the middle ear. For subtotal (incomplete) removal of the tumor, and depending on the patient’s age, radiation therapy or stereotactic radiotherapy (gamma knife) is used.
Treatment prognosis
The treatment prognosis is favorable. But the formation of new adenomas in other parts of the intestine cannot be ruled out, so we recommend that all patients over 50 years old undergo a total colonoscopy under anesthesia every 10 years with simultaneous removal of detected tumors. This will prevent the development of colorectal cancer or detect it in the early stages, when treatment prognoses are very optimistic.
As part of the prevention of serrated adenoma, it is recommended to avoid alcohol and tobacco use, as well as control weight. Considerable attention is paid to the timely detection of polyps using the same colonoscopy.
Removal of a serrated adenoma of the colon allows the patient to return to his normal lifestyle as soon as possible. The endoscopic techniques used at the Euroonko clinic are painless, safe, low-traumatic and have minimal risks of complications.
Book a consultation 24 hours a day
+7+7+78