What are salivary glands
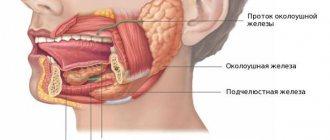
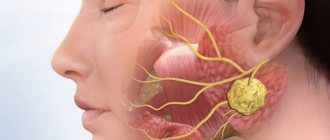
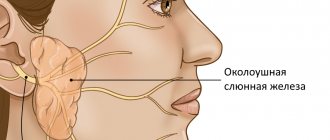
The salivary glands are divided into small and large. The last type of structures refers to paired organs and is localized on three sides. The major salivary glands include:
- parotid;
- submandibular;
- sublingual.
The submandibular glands are the least likely to become blocked because their ducts have the largest diameter. Also, the disease rarely affects structures located under the tongue.
There are more than 600 minor salivary glands. All of them perform important functions in the human body:
- They synthesize proteins and enzymes necessary for complete digestion of food.
- Produce hormone-like substances.
- Filters blood components into saliva.
These structures, like other internal organs, are subject to pathological processes. Main types of damage:
- sialadenitis or blockage;
- mumps;
- sialolithiasis.
The first type of violation is more common than the others listed.
Sialolithiasis is associated with the formation of stones in the ducts of the gland and a violation of the outflow of saliva from it.
Sialendoscopy as a method for removing stones from the salivary gland
Chronic obstructive pathologies of the salivary glands can be caused by the presence of salivary stones, the formation of a mucus plug, duct stenosis, the influence of foreign bodies, or anatomical variations in the gland duct system, which can result in retention of saliva in the duct, discomfort, and even infection. Specifically, sialolithiasis is a condition in which a calcified mass forms in the salivary gland. Most often, this disorder is observed in the area of the submandibular gland (in the so-called “Wharton’s duct”) and can cause swelling and pain in the affected area, especially during stimulation of salivation. If the stone does not come out of the gland on its own, it must be removed surgically.
To diagnose such pathologies, methods of radiosialography, ultrasound examination and magnetic resonance sialography can be used. Radiosialography is the most common method for identifying stones in the salivary gland duct, but its use is contraindicated in cases of acute infection or if the patient is hypersensitive to the contrast agent. Ultrasonography is a first-line diagnostic method that allows non-invasively and without the use of contrast to visualize the presence of a calculus in the salivary gland. It should be remembered that the parameters of sensitivity and specificity of this method vary depending on the stage of mineralization of the stone. For diagnostic purposes, of course, you can use more expensive methods such as computed tomography, magnetic resonance imaging or scintigraphy.
Currently, sialoendoscopy is widely used as a non-invasive approach for diagnosing and treating pathologies of the salivary glands. This method allows for direct access to the gland duct, its expansion and irrigation, as well as to establish the presence or absence of patency of the duct.
In this article, we describe the clinical cases of two patients who underwent sialolithotomy procedures using a sialoendoscope at Korea University Anam Hospital. In addition, we will describe the differences between sialoendoscopy and other methods for diagnosing and treating sialolitis.
Clinical case 1
Patient Information
An 81-year-old female patient presented to the dental clinic with a sensation of a foreign body under her tongue and symptoms of dry mouth. She was previously diagnosed with thyroid carcinoma in June 2003 and underwent a total thyroidectomy procedure. The patient's medical history included hypertension and chronic kidney disease. The stone was identified in the duct of the right submandibular gland (Figure 1).
Figure 1. Salivary stones measuring 2 × 10 mm were identified in the right submandibular gland using CBCT.
Surgical procedure
The working area was treated with betadine. After disinfection, the oral cavity was washed generously with saline solution. Local anesthesia was performed in the area of the tongue and floor of the mouth with a 2% lidocaine solution with an epinephrine concentration of 1:100,000. Afterwards, the tongue was sutured with 3-0 silk thread in order to provide optimal conditions for the operation. Using a microscope, the entrance to the duct of the right mandibular gland was found, after which it was entered with probe No. 0000, and then expanded to the size of probe No. 3 (photo 2). In order for the endoscope to penetrate the lumen of the duct, it was expanded using a dilator. The sialoendoscopy procedure was performed under copious irrigation with saline solution. The stone was removed using a three-wire ring (loop) (photo 3). The size of the opening of the duct was smaller than the size of the stone, so the doctor had to make a 0.1 cm incision at the entrance to the gland duct. After removing the stone, we examined the gland with an endoscope to make sure there was patency (photo 4). The glandular system was washed with a steroid solution. No bleeding, swelling or pain was noted in the postoperative period. The patient underwent daily dressings of the intervention area and monitoring for the development of possible wound infection.
Photo 2. a. Gland duct probe. b. Orifice dilator. c. Endoscope monitor. d. Three-portable endoscope. e. Three-wire ring (loop).
Photo 3. a. Stones in the gland duct. b. Removing stones using a loop. c. Capture the stones with a loop and remove them from the duct.
Photo 4. Removal of stones through the mouth of the submandibular salivary gland. b. View of removed stones.
Clinical case 2
Patient Information
A 66-year-old man sought dental attention due to a blocked duct of the right mandibular gland (Figure 5). Approximately 7-8 years ago, he noticed swelling and pain in the lower neck while eating. The sialolithotomy procedure was performed 4-5 years ago in another hospital, but the stones were never completely removed due to their pathological mobility during the operation. The patient had no systemic health problems.
Figure 5. Salivary stones measuring 3 × 4 mm were identified in the right submandibular gland using CBCT.
Surgical procedure
The working area was treated with betadine. After disinfection, the oral cavity was washed generously with saline solution. The patient was given full anesthesia via nasotracheal intubation, and the tongue was sutured with 3-0 silk suture. The intervention protocol was similar to the one we have already described in the first clinical case (photo 6). No bleeding, swelling or pain was noted in the postoperative period. The patient underwent daily dressings of the intervention area and monitoring for the development of possible wound infection.
Photo 6. View of the removed stone.
Discussion
Symptoms of obstructive salivary gland pathologies include recurring, painful swelling of the major salivary glands, which can negatively affect the patient's quality of life. Previously, radiosialography, sonography and MR sialography methods were used to diagnose diseases of the salivary glands. Radiosialography is the main method for examining the salivary glands, which can be used to diagnose sialolithiasis by analyzing images obtained after the injection of contrast into the gland duct. Contraindications to the use of this method are similar patient reactions to the contrast agent and the presence of an acute infectious lesion. Sonography is a non-invasive method for diagnosing stones in the structure of the salivary glands, however, the effectiveness of this approach largely depends on the experience of the doctor conducting the diagnosis. MR sialography allows for complete visualization of the entire salivary gland system, however, the resulting diagnostic images may be characterized by the presence of various types of distortions and artifacts, especially in cases of adjacent localization of dental restorations. However, all of the above-mentioned limitations characteristic of different diagnostic methods can be overcome using the sialoendoscopy method. It is less invasive than other approaches to diagnosing salivary gland pathologies and can be successfully used to assess the condition of their ducts and internal structure.
Several research groups have examined how satisfied patients were with the sialoendoscopy treatment process. Kroll et al, using the short version of the SF-36 questionnaire, found that patients reported a high level of satisfaction after sialoendoscopy. Aubin-Pouliot et al, using a questionnaire designed to assess chronic obstructive sialadenitis, demonstrated similar results. In addition, an interesting fact was established that after sialoendoscopy on the submandibular gland, the symptoms decreased much more pronounced than after a similar manipulation on the parotid salivary gland.
Recent studies have shown that microsialoliths play an important role in the pathogenesis of chronic sialadenitis. They can accumulate in normal salivary glands and provoke the development of obstructive atrophy. The latter, in turn, promotes the colonization and proliferation of microbes, causing inflammation in the peripheral ductal system, accompanied by even more severe atrophy and progressive infection, leading to chronic sialadenitis. According to Quinn et al, intraductal placement of antibiotics facilitates their penetration into the parenchyma of the glands, allowing the existing symptoms of the lesion to be completely eliminated. However, the same results were obtained when irrigating the internal structure of the glands with saline solution.
Radioactive iodine (RAI) therapy is another cause of salivary gland disease. According to Kim, chronic sialadenitis is the most common complication of RAI, especially in cases after thyroidectomy. The prevalence of chronic sialadenitis associated with RAI is 11–65%. Damage to the salivary glands caused by radioactive iodine leads to the development of obstructive sialadenitis and recurrent swelling with or without pain during meals. This chronic condition subsequently causes hyposalivation and associated symptoms, such as difficulty swallowing, taste disturbances, oral candidiasis and caries. Currently, chronic sialadenitis caused by radioactive iodine therapy is treated conservatively by maintaining a good level of oral hygiene, frequent hydration, the use of saliva substitutes, and stimulation of the salivary glands.
According to Kim's study, sialoendoscopy demonstrates similar effects to sialocentesis (intraductal irrigation with sterilized saline) and can improve obstruction symptoms as early as 3 months after mechanical dilatation with an endoscope. However, in patients with chronic sialoadenitis caused by radioactive iodine therapy, sialoendoscopy has been found to have limited ability to relieve existing symptoms of xerostomia.
This article described examples of using the sialoendoscopy method to remove stones from the salivary glands. This method is more effective compared to other approaches to the treatment of sialolithiasis, and at the same time less uncomfortable. In the two clinical cases analyzed, patients did not demonstrate any significant complications or similar effects after performing the manipulation.
Conclusion
This article describes two clinical comparisons of non-invasive sialolithotomy procedures using sialoendoscopy. This approach can be effectively used not only to treat cases of sialolithiasis, but also for ductal stenosis and sialadenitis. At the same time, sialoendoscopy is a minimally uncomfortable procedure, which is characterized by a low level of complications. To formulate any definite recommendations regarding the use of sialoendoscopy in cases of stones in the salivary glands, it is necessary to ensure that studies are carried out with the participation of a larger number of subjects.
Authors: Dong-Keon Lee, Euy-Hyun Kim, Chang-Woo Kim, Mong-Hun Kang, In-Seok Song, Sang-Ho Jun
Causes
The acute course of the pathology in 99% of cases is associated with the introduction of harmful microorganisms into the structure. Depending on the type of pathogenic agent, the following causes of blockage of the salivary glands are distinguished:
- Epidemic parotitis caused by a viral infection. The main route of infection is airborne. The virus penetrates through the mucous membranes of the nasopharynx and enters the blood. Reproduction of pathological particles occurs in the glandular structures of the parotid glands. In representatives of the stronger sex, the testicles, which have glandular tissue, are also affected. This type of disease can cause infertility.
- Bacterial damage. The disease progresses due to external factors and internal chronic diseases.
Among the factors provoking sialadenitis, the following should be noted:
- lack of oral care;
- narrowing of the ducts of the salivary glands associated with exhaustion of the body or surgery;
- cancerous damage to structures;
- diabetes;
- dysfunction of the digestive system;
- blocking of the duct by a foreign body.
Due to impaired salivation, optimal conditions are created for the proliferation of bacterial flora. The problem can be triggered by chronic infectious pathologies - typhoid fever, scarlet fever, chronic gingivitis or tonsillitis. Purulent wounds and boils also increase the risk of blockage of the salivary gland duct.
The chronic form of the disease does not occur against the background of acute sialadenitis, as occurs with other diseases. The condition is explained by the fact that the affected glands are naturally prone to the disorder in question.
Chronic inflammation of structures is more often observed in people:
- having a hereditary predisposition to sialadenitis;
- those suffering from autoimmune pathologies;
- suffered severe hypothermia.
The risk category for the disease includes patients with diabetes mellitus, cardiovascular and neurological diseases.
Causes of salivary gland cancer and risk groups
A normal salivary gland cell becomes cancerous when a certain set of mutations occurs in it. The development of malignant tumors is caused by mutations in oncogenes (genes that activate cell reproduction) or tumor suppressor genes (suppress cell reproduction, “repair” damaged DNA, trigger programmed cell death - apoptosis). In each specific case, it is very difficult to judge the reasons for the mutations that occurred in cells. It is impossible to say why exactly they happened.
There are some risk factors that increase the likelihood of developing a malignant tumor:
- The older a person is, the more changes in his genes accumulate, the higher the likelihood of developing various types of cancer.
- Salivary gland cancer is more common in men than in women.
- Irradiation of the head. For example, this may be a previous course of radiation therapy, exposure to ionizing radiation in the workplace.
- There is evidence that the risk of salivary gland cancer is increased in people who have certain occupational hazards: contact with asbestos, nickel alloy dust, work in enterprises that produce rubber and woodworking.
The role of heredity is currently considered insignificant. Most patients do not have a family history (close relatives who have been diagnosed with the same type of cancer). The role of alcohol and tobacco has not been proven. These unhealthy habits are known to increase the risk of head and neck cancer in general, but no association has been found with salivary gland cancers.
Is a mobile phone dangerous? In one study, researchers found that heavy cell phone users were more likely to have parotid tumors (usually benign). But other studies have not found such a relationship.
Symptoms
With mumps, the parotid glands are affected. The problem is manifested by the following characteristic symptoms:
- deterioration of general health;
- swelling of neck tissues;
- pain when pressing on areas of inflammation;
- discomfort during conversation and eating;
- headaches of varying intensity;
- dry throat.
Symptoms of inflammation of the sublingual salivary gland and its treatment
If the pathological process spreads to the sublingual and parotid glands, then the symptoms of blockage are supplemented by:
- increased temperature;
- intoxication of the body;
- bad breath;
- severe pain when opening the mouth;
- sensation of a foreign body under the tongue.
Depending on the form of the course and symptoms, sialadenitis is also divided into serous, purulent and gangrenous. The first form of pathology is characterized by: swelling of the salivary gland; deformation of the earlobe; increase in temperature, release of serous fluid when pressing on the inflamed structures, obstruction of the duct.
With the gangrenous form of the disease, it becomes difficult for a person to sleep at night due to pain. There is also a thickening of the affected structure, spreading of swelling to the tissues of the ear, neck and cheeks. The skin over the problem area turns red.
The advanced form of sialadenitis is gangrenous. It is characterized by a rapid increase in pathological symptoms, death of soft tissues, and blood infection. Untimely medical care can lead to the death of the patient.
Symptoms of the disease
Benign and malignant tumors of the salivary glands present with similar symptoms. One of the main differences is that cancer grows much faster and more often leads to a number of symptoms associated with growth into surrounding tissues and compression of nerves.
You need to visit a doctor if you are bothered by the following symptoms:
- A lump or swelling has appeared in the mouth, cheek, jaw, or neck.
- You have noticed that your face has become asymmetrical.
- I am worried about pain in the mouth, neck, ear, cheek, jaw. It doesn't last long.
- Numbness of part of the face.
- Weakness in the facial muscles, because of this, half of the face may be “lowered,” which becomes especially noticeable when baring teeth or frowning.
- I can't open my mouth wide.
- Difficulty swallowing.
Diagnostics
A treatment regimen for salivary gland blockage is prescribed after an x-ray. In this case, a panoramic image is recommended, allowing one to study the condition of the affected structures from different angles. In difficult cases, x-rays of the glands are performed using a contrast agent. This research technique is also used in cases of suspected cancer.
Photo of an x-ray of the glands
Before making a diagnosis, the doctor visually examines the patient’s oral cavity and palpates the salivary glands. The success of treatment depends on the timely identification and elimination of the provoking factor.
Differential diagnosis of various forms of sialadenitis plays an important role. Each type of pathology requires a special approach to treatment, so the doctor pays attention to the symptoms of the disease.
The criteria by which a doctor distinguishes one disease from another are presented in the table below:
| Problem type | Provoking factor | Symptoms of blockage |
| Chronic parenchymal | Formed due to damage to the gland by benign tumors. Infection does not play a role in the development of the disease | Slow development of symptoms, without sharp pain |
| Acute lymphogenous | Develops after an infectious disease or when the immune system is weakened | Characterized by the spread of the inflammatory process to adjacent soft tissues |
| Chronic interstitial | Triggered by autoimmune problems (rheumatoid arthritis, lupus erythematosus) | Slow development of signs of the problem with periods of exacerbation and remission |
| Sharp contact | Occurs due to boils and open wounds located next to the saliva gland | The pathology is characterized by severe pain, swelling of the affected structure and a sharp decrease in salivation |
| Epidemic | Develops against the background of the introduction of viral particles into the gland | Swelling of the parotid and cervical glands |
Treatment
Therapy for sialadenitis is carried out in a hospital. Most often, signs of pathology are eliminated with the help of medications and physiotherapeutic procedures. Less commonly, doctors resort to surgery to cleanse or remove the gland. The operation is indicated for purulent or gangrenous type of problem.
For mumps, patients are prescribed antiviral drugs. Symptomatic treatment is also carried out, aimed at reducing the temperature and relieving pain in the affected area.
Acute blockage of the salivary gland requires complex therapy. To normalize the function of the gland, patients are prescribed a special salivary diet. The diet includes crackers, sour fruits and vegetables, and berries. Drink a 1% solution of pilocarpine hydrochloride orally. The substance promotes contraction of the muscles located next to the salivary gland. All measures are aimed at accelerating the removal of foreign objects and pathogenic particles by enhancing the secretory function of the gland.
If the disease is infectious, the use of antibacterial agents is required. Penicillin antibiotics and antiseptic solutions are injected into the ducts to disinfect the affected area (Miramistin, Dioxidin)
To relieve swelling and inflammation, compresses with Dimexide are applied to the problem area. The procedure is carried out twice a day for 30 minutes. The drug also reduces the intensity of pain.
Additionally, the inflamed glands are heated using UHF. If the situation worsens, a novocaine-penicillin blockade is performed. The procedure is necessary to prevent infection of neighboring tissues.
Chronic sialadenitis is treated according to a different scheme:
- The inflamed ducts are massaged daily with the introduction of antibacterial drugs. The procedure acts as a prevention of purulent complications of sialadenitis.
- Injections with novocaine are made into the subcutaneous fat to improve the secretory function of the glands.
- For 10 days they undergo daily treatment with electric currents.
- To prevent exacerbation of the pathology, iodolipol is injected into the problem area once every 3 months.
Prevention of violation
There are no vaccines or specially developed drugs against sialadenitis. The only exception is mumps. To prevent the development of the disease, the child is offered an inactivated vaccine against measles, mumps and rubella. All children over 1 year of age are vaccinated against the disease. After the vaccine, stable immunity to the pathogen remains in 96% of vaccinated people.
There are also nonspecific measures to protect against sialoadenitis, including:
- regular oral hygiene;
- timely treatment of wounds and mouth ulcers;
- elimination of chronic foci of infection;
- prevention of saliva stagnation in infectious diseases.
Treatment of salivary gland blockage should be carried out promptly. Otherwise, the disease threatens infection of the soft tissues of the face and further infection of the body. The consequences of sialadenitis require resuscitation measures to preserve the life and health of the patient. The list of dangerous consequences of pathology also includes: rapid destruction of enamel, disruption of oral microflora, chronic inflammation of the gums. For this reason, it is important not to bring your health condition to a critical level.