Why does my tongue hurt?
Physiological reasons
Pain in the tongue is often the result of minor injuries: superficial burns from too hot liquid, accidental biting, damage from hard pieces of food, fish bones.
Painful sensations are combined with numbness or, on the contrary, hypersensitivity. They disappear within a few minutes or hours, less often – days. Burning and sore tongue can also be caused by eating spicy foods, certain spices, or drinking strong alcoholic beverages. In people who smoke, the sensitivity of the tongue increases due to the constant effect of tobacco smoke on the mucous membrane, which leads to the frequent occurrence of pain under the influence of other irritants.
Traumatic injuries
More serious injuries occur due to biting the tongue during an attack of epilepsy, sports, or accidents. Abrasions and wounds in the form of teeth marks are found on the tongue. Depending on the severity of the damage, pain lasts from several days to 1-2 weeks. In patients with incorrectly selected orthodontic structures or poorly fitted removable dentures, pain becomes the result of chronic irritation of the tongue. With advanced caries, the organ is systematically injured by the sharp edges of the teeth.
Glossitis
Pain syndrome is not observed with all glossitis; it is more typical for infectious lesions. The inflammatory process of bacterial etiology is manifested by hyperemia, swelling, increased local temperature, aching, raw pain. With viral glossitis, blisters form, which subsequently open to form painful erosive defects.
Tongue pain
Abscess and phlegmon of the tongue
An abscess develops against the background of microtrauma or becomes a complication of bacterial glossitis. Characterized by rapid onset and progression of symptoms. Superficial abscesses are localized under the mucosa, usually in the back area. They represent an area of limited swelling with a painful thickening in the center. They are accompanied by sharp pain when moving the tongue, swallowing, and sometimes radiating into the ear.
Deep abscesses are located deep within the organ. They manifest themselves as hyperthermia, intoxication syndrome, in some cases – chills, enlarged regional lymph nodes, and excessive salivation. The tongue is so swollen that it can hardly fit in the mouth, making speech and breathing difficult. The pain is sharp, jerking, bursting, pulsating, aggravated by movement, swallowing, or touching.
In patients with phlegmon, the area of purulent inflammation is not limited, quickly spreading to the entire tongue, floor of the mouth, and neck. Febrile fever, chills, and regional lymphadenitis are observed. The pain syndrome is intense, diffuse, depriving sleep. Eating is very difficult or impossible. Speech is slurred. Due to the blockage of the airways due to swelling of the soft tissues of the oral cavity and oropharynx, attacks of suffocation develop.
Oral candidiasis
Painful sensations are more often observed in acute candidiasis, but are not typical for the chronic form of the disease. Children, old people, and weakened patients with severe somatic pathologies suffer. A loose or dense milky-white cheesy coating forms on the tongue, spreading to the palate, cheeks, and lips. When plaque is removed, a bleeding, eroded or macerated mucous membrane is exposed.
When eating food, pain and burning occur. In the absence of therapeutic measures, transformation into atrophic candidiasis is possible. The tongue becomes shiny, fiery red. The papillae atrophy. The mucous membrane of the oral cavity is swollen, hyperemic, dry, thinned. Patients complain of severe pain in the affected area. Plaque is not detected or is insignificant.
Glossalgia
Glossalgia is a pathology accompanied by unpleasant sensations in the tongue in the absence of organic changes. Occurs in diseases of the liver and gastrointestinal tract, vascular, endocrine diseases, pathologies of the central and peripheral nervous system. Painful sensations without clear localization, diffuse, have a burning, pinching or sore character, are more pronounced in the area of the tip and sides, less often appear on the root and back of the tongue. May be episodic or regular. As a rule, they are combined with neurotic disorders.
Xerostomia
Pain in the tongue is a concern in the final stages of the disease. Against the background of complete inhibition of the function of the salivary glands, glossitis develops. Constant dryness of the mucous membrane leads to the formation of erosions and ulcers. Painful sensations intensify when talking, while eating, and are combined with constant dry mouth. Patients with xerostomia may have multiple caries.
Neuralgia
Pain in the two anterior thirds of the tongue is characteristic of damage to the third branch of the trigeminal nerve (n.mandibularis), combined with painful sensations in the chin, lower jaw, lower lip, gums, and buccal mucosa. The pain syndrome is paroxysmal in nature and is a series of impulses resembling an electric shock. It is provoked by cold influences, shaving, chewing, speech, laughter.
With neuralgia of the glossopharyngeal nerve, pain appears at the root of the tongue, from where it spreads to the tonsils, soft palate, pharynx, and sometimes to the ear, eye, and lower jaw. The attack is provoked by swallowing, chewing, yawning, coughing, talking, and is accompanied by dryness in the throat, which at the end of the paroxysm is replaced by increased salivation.
Neuralgia of the hypoglossal ganglion is characterized by pain in the anterior parts of the tongue, the sublingual zone: boring, burning, pulsating, paroxysmal. Lasts from a few minutes to 1 hour. It radiates to the lower jaw, temple, back of the head, side of the neck, shoulder girdle, sometimes to the arm, upper chest. It intensifies when talking, eating, especially rich or spicy food.
Anemia
Pain in the tongue is typical of pernicious anemia and is caused by glossitis. The tongue becomes “varnished” and acquires a crimson color. Weakness, tachycardia, and dizziness are observed. Characteristic symptoms are shortness of breath, pale skin, puffiness of the face. Loss of appetite, hepatomegaly, and stool instability are detected. Neurological disorders are detected: muscle weakness, gait changes, stiffness, numbness of the limbs.
Sometimes painful sensations in the tongue area occur with iron deficiency anemia. Glossitis is combined with dysphagia, angular stomatitis, and atrophic gastritis. The prevailing symptoms are weakness, tinnitus, dizziness, shortness of breath, and palpitations. Dry skin, deformed nails, and hair loss are noted.
Other reasons
Pain in the tongue is sometimes detected in the following conditions:
- Allergy
. Soreness, paresthesia, severe itching are caused by food allergies, less often - by a reaction to plant pollen or animal fur. Combined with sneezing, lacrimation, swelling of the mucous membranes. - Initial stages of cervical osteochondrosis.
Vague pain sensations in the tongue are complemented by awkwardness, restrictions in neck movements, and pain in the neck. - IHD.
Pain in the tongue, oral cavity, and lower jaw can be observed during an atypical course of an attack of angina pectoris or myocardial infarction.
Oral examination
Glossitis
Glossitis
is an inflammation of the tissues of the tongue, manifested in its soreness, changes in color and structure, and the appearance of a dense coating. There is a burning sensation, hyperemia (overflow of blood vessels), food loses its taste, and salivation increases.
If the doctor has diagnosed the patient with glossitis, then the next step is to find out whether this indicates a pathology of other organs. This could be a herpes virus, poisoning with heavy metal salts, etc. Treatment is prescribed depending on the initiating cause, trying to exclude it. It usually includes local antiseptic therapy.
Diagnostics
The cause of the symptom is determined by the dentist. If there are indications, patients are referred for consultation to a gastroenterologist, therapist, neurologist, and other specialists. The doctor determines when the pain first appeared, what symptoms were accompanied, and how the disease developed. To clarify the diagnosis, the following procedures are performed:
- Inspection
. During the physical examination, general changes are sometimes detected (for example, pale and dry skin with anemia). When examining the tongue, swelling, hyperemia, discoloration, the presence of erosions, ulcers, and infiltrates may be detected. With neuralgia, areas of pain indicate damage to one or another nerve. During a dental examination, carious teeth, defects in dentures and orthodontic structures may be detected. - Instrumental techniques
. To exclude xerostomia and assess the condition of the salivary glands, sialography and ultrasonography are recommended. If gastrointestinal pathologies that provoke glossalgia are suspected, esophagogastroduodenoscopy and a contrast study of the stomach are performed. For neuralgia, electromyography is indicative. - Lab tests
. Confirm the presence of pernicious or iron deficiency anemia. As part of the differential diagnosis, saliva is examined. In case of candidiasis and bacterial lesions, the discharge is inoculated onto nutrient media. For viral infections, PCR is performed.
Desquamative
Glossitis on the tongue, as in the photo, is scientifically called desquamative, migratory or exfoliative1, but popularly this disease is better known as “geographic tongue”, because in appearance it resembles a geographical map with clearly defined continents in the form of bright red areas of the affected area. mucous membrane.
The photo shows the geographic language
The disease most often develops in the fair half of humanity, more often during pregnancy due to metabolic disorders, when the expectant mother lacks vitamins and useful nutritional minerals. Also, pathology often develops against the background of chronic lesions of the gastrointestinal tract, burns of the mucous membrane and acute allergic reactions.
It is worth knowing that this form rarely develops into an acute stage, so if characteristic signs appear, you should not wait for accompanying symptoms, such as pain or swelling - you should immediately consult a doctor.
Treatment
Pre-hospital assistance
It is recommended to avoid foods that are too hot, cold, hot or spicy. You should eat soft foods that do not injure the tongue, preferably stewed, boiled, steamed. The best option is a diet that includes purees, slimy porridges, pureed soups. Before and after meals, you need to rinse your mouth with weak solutions of chlorhexidine and potassium permanganate or a solution of furatsilin. For severe pain, the surface of the tongue can be lubricated with local anesthetics.
Conservative therapy
An important part of the treatment is the sanitation of the oral cavity, and, if necessary, the replacement of dentures and orthodontic structures. The list of therapeutic measures is determined by the nature of the pathology:
- Glossitis
. Rinses and applications with anesthetics are indicated. For intense pain, lubrication with a mixture of glycerin and anesthesin is effective. Plaque is removed with a swab containing proteolytic enzymes. Treat with antiseptics. Local healing drugs are used. - Phlegmon and tongue abscess
. For superficial abscesses, rinse with antiseptic solutions, prescribe antibacterial agents, and if ineffective, surgical interventions are performed. For deep abscesses and phlegmons, conservative therapy is an auxiliary treatment method, carried out against the background of operations, and includes antibiotics, analgesics, antihistamines, and anti-inflammatory drugs. - Candidiasis
. Alkalinizing rinsing solutions are used as local remedies. The oral cavity is lubricated with antifungal ointment and treated with solutions of iodinol, lugol, fucorcin. The therapeutic regimen also includes general antifungal drugs and, in severe cases, immunotherapy. - Glossalgia
. It is recommended to take light tranquilizers, motherwort, and valerian. A good result is achieved with trimecaine blockades of the lingual nerve and injections of B vitamins. Unpleasant sensations are eliminated through oral baths and applications with anesthetics. The main pathology and neurotic disorders are treated. - Xerostomia
. It is recommended to stop smoking and drinking alcohol, use soft-bristled toothbrushes, drink frequently to moisturize the mouth, and suck on sugar-free lollipops to stimulate saliva production. The oral cavity is lubricated with a solution of vitamin A. Novocaine blockade of the salivary glands is performed, vibration massage, medicinal electrophoresis, and galvanotherapy are prescribed. - Neuralgia
. Anticonvulsants, non-narcotic analgesics, and vitamin complexes are used. For severe pain, antidepressants, sleeping pills, sedatives, and antipsychotics are recommended. Therapeutic blockades are carried out. Lubricate the tongue with a solution of cocaine. Patients are given a referral for SMT, galvanization, and diadynamic therapy. - Anemia
. In case of iron deficiency anemia, treatment of the underlying disease, nutritious nutrition with a high content of heme iron, and ferrous preparations are required. In case of pernicious anemia, the provoking pathology is corrected and vitamin B12 is prescribed.
The main reasons for the development of pathologies
Many people ask questions about how and how to treat glossitis of the tongue. But, as we noted above, before prescribing a set of therapeutic measures, you first need to find out what form of pathology the patient has and what exact reason it is caused by.
| Oral problems | Diseases of the body | Related factors |
|
|
|
Do you think you have glossitis of the tongue and don’t know what to do? Even minor symptoms of pathology and slight discomfort are a reason to consult a doctor who will conduct a comprehensive examination (examination, smear or scraping, blood tests and LBC culture, histology), make an accurate diagnosis and prescribe treatment.
Structure and functions
The tongue is a muscular organ without bones, covered with a mucous membrane.
Main functions:
- is directly involved in the pronunciation of sounds;
- determines the taste of what a person eats and drinks;
- is an integral element of the digestive system - it carries out the primary processing of food before it enters the esophagus.
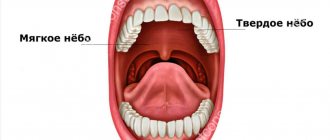
The structure of the organ is quite simple, but very interesting. The tongue is divided into two parts: the back - the root and the front - the body or, as it is also called, the back, which has a velvety structure. The top is covered with papillae, which are responsible for taste buds.
Comments
At what age do people usually get Günther Müller's glossitis?
Vladimir (01/30/2021 at 11:57 pm) Reply to comment
- This type of glossitis, in fact, like all others, can develop in patients of any age, but people who have chronic diseases, pathologies of the gastrointestinal tract, and smokers are always at risk.
Editorial staff of the portal UltraSmile.ru (02/05/2021 at 09:16) Reply to comment
It turns out that our tongue can say a lot about the body, it’s not for nothing that doctors always ask to see it, even if they just came for a medical examination. Can any age have these diseases or older people?
Maria (02/05/2021 at 07:32) Reply to comment
I wonder what is better to eat to avoid such serious problems? It seems to me that a lot depends on food. Against the backdrop of abundance, you begin to not understand what is useful and what is not.
Marina (02/05/2021 at 08:20) Reply to comment
I once had glossitis, about five years ago. Although I don’t smoke, don’t drink, I lead a healthy lifestyle. Before this I had a sore throat. What folk remedies do you recommend that are the most effective?
Irina Frolova (02/05/2021 at 09:40) Reply to comment
Hello. I developed glossitis due to candidiasis. The tastes are very dull. Everything seems to have been cured, but I don’t feel the same brightness from food. Please tell me, can something be done about this or is it forever?
Vera (03/04/2021 at 10:56 am) Reply to comment
Since childhood, all doctors have told me “geographical language.” It has some stains and a yellow-green coating. Is this a disease or not? It just doesn't bother me the way it feels. But it's not very easy to clean.
Vladimir (03/04/2021 at 11:38 am) Reply to comment