Postoperative complications develop in at least 10% of all operations. There are several reasons for this.
Firstly, the situation that made surgical intervention necessary does not disappear at the time of surgery. The patient will have a long time to restore normal functioning of the body.
Secondly, surgical intervention itself is a non-physiological effect that disrupts many cyclic processes in the body. This includes the introduction of a narcotic substance that loads the liver and kidneys, and a change in heart and respiratory rhythm, blood loss, and pain. Emergency and long-term operations are natural factors for the occurrence of complications. Normally, on the 3-4th day the body copes with unexpected circumstances, and the patient’s well-being improves.
Treatment of postoperative complications requires a qualified approach on the part of doctors and medical personnel.
Local complications
The following troubles may occur in the area of the surgical wound:
- bleeding due to a blood clotting disorder, slipping of the suture material from the vessel or insufficient restoration of hemostasis during surgery. To eliminate bleeding, stitches are placed, re-ligation is done, cold is applied to the wound, or hemostatic drugs are administered;
- hematoma due to a bleeding vessel. The hematoma is opened and removed by puncture. If it is small in size, it dissolves with ultraviolet irradiation or application of a compress;
- infiltrate - swelling of tissue within 10 cm from the edges of the suture due to infection of the wound or the formation of necrosis in the subcutaneous fat. Depending on the cause, physiotherapeutic procedures or surgical treatment are used to resolve it;
- suppuration - infiltrate with severe inflammation. To eliminate it, the sutures are removed, the edges of the wound are exposed, washed and drainage is installed;
- eventration - prolapse of internal organs outward due to suppuration, weak suturing of wound edges, increased intra-abdominal pressure during coughing or flatulence, or reduced tissue regeneration (healing). It is necessary to reposition the organs with aseptic technique, strict bed rest and wearing a tight bandage.
- Ligature fistula - occurs when an abscess forms around the suture material. It requires excision along with suture material.
Postoperative bleeding
Bleeding after surgery is a serious complication that can be fatal. Therefore, this condition requires immediate medical attention.
There are acute blood loss (mild), massive blood loss syndrome (moderate) and hemorrhagic shock (severe).
The main clinical criteria for assessing the patient’s condition and the degree of blood loss are hemodynamic indicators (blood pressure (BP), heart rate (HR), central venous pressure), hematocrit and hemoglobin levels.
Postoperative bleeding can be early or late.
Early blood loss occurs in the first few hours after surgery. As a rule, it develops against the background of a blood clotting disorder, due to a disorder of water-electrolyte balance or the action of narcotic drugs. Late bleeding occurs after several days or even weeks and is usually caused by infection in the wound or suture dehiscence. In any case, the patient’s life is in danger and urgent medical attention is required.
Causes of postoperative bleeding
- Arrosion of a blood vessel due to the onset of a purulent process. This complication occurs some time after the intervention.
- Dehiscence of sutures, slipping of the ligature from a large-diameter vessel. It is observed with incorrect suturing technique or the use of low-quality suture material.
- Blood clotting disorder.
- Infection.
Sometimes bleeding develops from small vessels that remain unstitched. This is possible when blood pressure decreases during surgery, causing the vessels to collapse.
Bleeding in the late postoperative period often develops due to purulent melting of tissue in the wound, disintegration of tumor tissue, and failure of sutures.
What types of bleeding are there?
- Arrosive - when the vascular wall is damaged due to the germination or disintegration of a neoplasm, a destructive or necrotic process (with tissue death).
- Diapedetic - with blood leaking through the vascular wall during scurvy, scarlet fever, malaria.
Classification by volume of blood loss:
- Lung 10-15% of circulating blood volume (CBV), up to 500 ml, hematocrit more than 30%
- Average 16-20% of blood volume, from 500 to 1000 ml, hematocrit more than 25%
- Severe 21-30% of bcc, from 1000 to 1500 ml, hematocrit less than 25%
- Massive >30% bcc, more than 1500 ml
- Lethal >50-60% of the volume of blood volume, more than 2500-3000 ml
- Absolutely lethal >60% of blood volume, more than 3000-3500 ml
Based on where the bleeding comes from:
- Venous – when the vein wall ruptures
- Arterial - from an artery
- Mixed - from different vessels
What are the symptoms of bleeding?
Common signs of internal bleeding are weakness, darkening or clouding of the eyes, drowsiness, dizziness, cold sweat, and thirst. Loss of consciousness is possible. The intensity of blood loss is determined by pulse rate, blood pressure and characteristic complaints of the patient. Also, as a rule, after surgery, a drainage is installed and there is a massive flow of blood through the drainage.
Minor blood loss often does not manifest itself in any way, but for some, the pulse increases slightly and the blood pressure drops slightly.
Manifestations of moderate bleeding: heart rate up to 100 beats per minute, decrease in systolic pressure to 80 mmHg. Art., moderate shortness of breath, dry mouth, cold hands and feet, cold sweat, dizziness, severe weakness, slow reactions, fainting.
With severe blood loss, symptoms are more pronounced. A drop in blood pressure of more than 80 mmHg is noted. Art., tachycardia more than 110 beats per minute, shortness of breath, hand tremors, excruciating thirst against the background of a decrease in the volume of urine excreted, apathy. There may also be a sharp pallor of the mucous membranes and skin, cyanosis of the limbs and the area around the lips, clouding or loss of consciousness.
Clinical manifestations of massive hemorrhage include cyanosis of the skin and mucous membranes, confusion, and delirium. The eyeballs sink inward, facial features become sharper, the pulse reaches 160 beats per minute, blood pressure drops to 60 mm Hg. Art.
With fatal and absolutely fatal blood loss, we are talking about a threat to life. The pupils dilate, convulsions appear, the number of heart beats (bradycardia) sharply decreases to 2–10 beats per minute, breathing becomes agonal, urine and feces are spontaneously released. The patient falls into a coma, his skin is dry, pale with a marbled pattern. The result is agony, death.
Treatment of postoperative bleeding
For minor bleeding, it may be sufficient to use local cold, a hemostatic sponge, or a tight bandage. Special drugs and blood components are also administered to stop bleeding.
In case of heavy bleeding, it is necessary to stop it. In case of bleeding from the surgical wound, re-ligation or additional suturing of the wound is required.
Stopping late postoperative bleeding often requires repeated emergency surgery.
https://www.facs.org/~/media/files/education/core%20curriculum/postoperative_care.ashx https://teachmesurgery.com/perioperative/general-complications/haemorrhage/ https://lektsia.com/8x2f8f .html
General complications
As a result of surgical intervention, systemic disorders occur in the body, which are considered as postoperative complications:
- painful sensations. They are relieved with analgesics, antispasmodics and desensitizing agents in various combinations;
- nervous system disorders. If the patient suffers from insomnia, he is prescribed sleeping pills and sedatives;
- Postoperative bronchitis and pneumonia appear more often in smokers. In such cases, antibiotics and symptomatic therapy are prescribed;
- acute heart failure is considered the most dangerous complication requiring measures to save the patient;
- acute embolism and thrombosis in cardiovascular pathologies, increased blood clotting, varicose veins. To prevent such complications, it is necessary to place the operated limbs above the level of the body, tighten the feet and legs with elastic bandages, and prescribe therapy with anticoagulants and desagrenants;
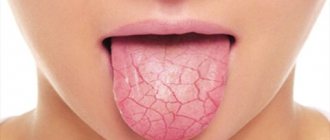
- complications of the gastrointestinal tract in the form of stomatitis and sialadenitis (inflammation of the salivary glands) or more serious consequences of the operation - paresis (lack of tone and peristalsis) of the stomach and intestines;
- On the part of the bladder, difficulty and retention of urination are often observed. Catheterization may help;
- Bedsores form when the patient remains in one position for a long time in a supine position. To prevent them, good patient care is needed. When bedsores appear, they are treated with antiseptic solutions and wound healing agents.
Treatment of complications after surgery is a very important point in the rehabilitation program for a surgical patient. This is given due attention by surgeons at the Sanmedexpert clinic. As a result, the number of postoperative complications is minimized.
Types of postoperative scars
Keloid.
A lumpy scar made of overgrown connective tissue that is red or bluish in color. It looks like a tumor or a mushroom cap. The size of the keloid scar is larger than the wound itself, it hurts, itches, and sometimes pulsates.
Hypertrophic.
Outwardly similar to a keloid, but its size does not extend beyond the wound. A hypertrophic scar does not cause any discomfort and lightens over time.
Normotrophic.
A well-healing scar is initially convex and reddened, after 3 months it becomes almost invisible, there is no sensitivity.
Complications of postoperative scars
Ligature fistula of a postoperative scar.
At the site of the suture, an inflamed hollow canal (hole) is formed, from which pus, sometimes urine and feces, are released. The cause of the complication is infection entering the body through the suture or an allergy to the threads with which the wound was sutured. The fistula can develop into an abscess, cellulitis or sepsis.
Infiltrate of postoperative scar.
This is a seal at the site of the suture, inside of which pus accumulates. The infiltrate is very painful to the touch, hot, red. Occurs due to infection of the suture.
Granuloma of a postoperative scar.
At the site of the scar, as a reaction to foreign bodies (suture threads), granulomas appear - nodules of dense tissue up to 2 mm in diameter, sometimes they contain pus. Granulomas are accompanied by an increase in the patient's body temperature.
Endometriosis of postoperative scars.
Occurs after gynecological operations on the uterine cavity, due to endometrial particles entering the wound. Patients feel pain in the scar area, blood is released from the suture, and dense nodules appear on the scar.
Treatment of complications of postoperative scars can be either surgical or conservative. Ligature fistula and infiltration usually require surgical intervention and re-suturing of the wound. Granulomas most often resolve on their own, but require aseptic treatment and medical supervision. When treating scar endometriosis, hormonal medications are prescribed.
Aesthetic surgery methods are used to remove keloid scars.
Introduction
The progress of tracheal surgery, like any other surgical specialty, is inextricably linked to ensuring the safety of treatment during and after surgery. This is achieved in a multicomponent way and concerns examination, adequate choice of surgical option, anesthesia, as well as the surgical technique itself and proper management of the postoperative period. An error regarding any of these components threatens the development of serious and even fatal complications. The most severe of these are vascular complications. They can have different character, localization and severity. Many studies have been devoted to the surgical safety of operations on the trachea [3, 4, 6—8, 10, 14, 17, 19, 20, 22, 24]. Over the years of development of tracheal surgery, significant progress has been achieved in this matter. In specialized highly qualified medical institutions, these operations have become quite safe. The incidence of postoperative complications and hospital mortality decreased significantly. The spectrum of complications, their etiopathogenesis were studied and preventive measures were proposed. In the structure of postoperative complications in tracheal surgery, the most dangerous are vascular complications, especially arrosive bleeding from large arterial vessels. They are the leading cause of hospital mortality.