- What is keratoplasty?
- Corneal pathology
- Causes of corneal diseases
- History of corneal transplantation
- How do you prepare for the operation?
- What types of keratoplasty are there?
- Postoperative period
Every day in our practice we see that every fourth patient comes to an appointment with a corneal disease. More than 10 million people worldwide suffer from corneal diseases. Pathology of the cornea is one of the main causes of decreased vision, blindness and low vision.
Indications
The list of indications includes pathologies that are not amenable to conservative therapy. Keratoplasty is indicated for patients with:
- corneal dystrophy (including those with minimal thickness);
- keratoconus (both in the early stages and in the late stages, including progressive ones);
- keratoglobus;
- Fuchs' dystrophy;
- the presence of scars on the surface of the cornea;
- damage to the cornea of various types;
- ulcers (wounds) of the cornea of any origin;
- eyesores of various natures, affecting visual acuity;
- bullous keratopathy associated with cataract surgery;
- congenital or acquired anomalies of the structure of the eye;
- defects of a traumatic nature.
Each indication for surgery for a particular patient is determined by the doctor.
Indications for keratoplasty
This surgery can be performed in the following situations:
- Correction of refraction, namely improvement of vision due to clouding of the cornea of the eye or destruction of its structure.
- For reconstructive purposes – maintaining the anatomical integrity of the cornea.
- For therapeutic purposes - as a way to treat infectious keratitis, refractory to any therapy with antibiotics and antifungals.
- The need for a cosmetic effect in the presence of large scars.
Keratoplasty is a last resort therapeutic measure. A transplant is performed only when other treatments are ineffective or there is no other treatment. Keratoplasty is relevant for the following pathological conditions:
- Keratoconus is a degenerative eye disease in which the cornea gradually takes on an abnormal conical shape. Pathological changes lead to significant visual impairment. In the initial stages of the disease, patients make do with glasses or contact lenses, but over time these products become ineffective and require replacement too often. Thinning of the central and pericentral zone of the cornea can lead to thinning of the stroma and acute entry of fluid into the corneal structures.
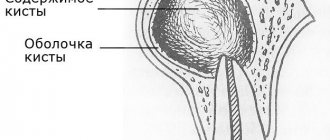
- Bullous keratopathy is secondary swelling of the cornea due to traumatic or degenerative endothelial dysfunction. The formation of so-called fluid-filled compartments occurs, which leads to deterioration of vision.
- Various types of dystrophic processes of a non-infectious nature. More often, such conditions are genetically determined. Such conditions include Fuch's endothelial dystrophy - a progressive decrease in the number of endothelial cells. Patients complain of blurred vision, especially pronounced in the morning and gradually disappearing during the day. The concept of stromal dystrophy unites a group of congenital dystrophic diseases in which the formation and accumulation of deposits occurs in the stromal layer. Over time, the deposits become denser, which leads to progressive loss of vision.
- Traumatic injuries to the eyeball with subsequent formation of massive scars often require keratoplasty.
- Infectious keratitis. A typical example is changes in the cornea as a result of recurrent eye damage by the herpes simplex virus. Symptoms can range from scar formation, vascularization, ulceration, or even corneal perforation.
Each clinical situation is considered individually, after which the specialist makes a decision on the need for transplantation or continuation of conservative therapy.
When keratoplasty is contraindicated
The list of contraindications includes:
- pregnancy;
- lactation period;
- inflammatory lesions of different parts of the eye (such as the cornea, sclera, conjunctiva) of an infectious nature: uveitis, keratitis, scleritis;
- ingrowth of blood vessels into the cornea (in normal conditions, the cornea of the eye and all its tissues are deprived of blood supply);
- chronic diseases in acute stages (complete remission should be expected);
- acute infections (you need to wait one to two weeks after the patient has completely recovered);
- autoimmune diseases.
Important! All contraindications and possible complications are identified during diagnosis.
Graft rejection and other complications
Graft failure is a potential complication of any transplantation. Due to the avascular structure of the cornea, such an undesirable scenario is often much less common in comparison with other organs and tissues. Rejection can develop either 2 weeks or a year after surgery. Patients in this situation complain of decreased vision, redness of the eye, pain and photophobia. With a timely diagnosis, adequate therapy with steroid hormones allows you to cope with the problem. Other complications include the addition of secondary flora, the formation of glaucoma and cataracts.
Keratoplasty is a high-tech operation that allows patients with previously incurable diseases to regain good vision.
Making an appointment Today: 27 registered
Varieties
There are the following types of keratoplasty:
- End-to-end (penetrating) operation
. In this type, all layers of the patient's cornea are replaced, including the epithelium, stroma, and endothelium (the back layer of the epithelium adjacent to the chamber of the eye). Penetrating keratoplasty is indicated for pathological processes affecting cells of all tissues of the cornea. - Layered
. With the layer-by-layer technique, only individual sections of the cornea are transplanted. Not the entire tissue is transplanted, but a separate layer or two (unlike penetrating keratoplasty, in which the cornea is separated completely).
There are two types of lamellar keratoplasty:
- Front
. Layered anterior keratoplasty involves cutting and subsequent transplantation of the upper epithelium (the first layer), as well as in some cases the main layer - the stroma. The posterior lining epithelial membrane usually remains intact. - Posterior with excision of the posterior endothelium
. The method is more complex, but has fewer complications.
Depending on the purpose of the procedure, the following types of keratoplasty are distinguished:
- Therapeutic surgery is necessary to restore the structure and improve the condition of the cornea, often performed in conjunction with other interventions (for example, lens replacement).
- Refractive (optical), necessary to restore the functions of the patient’s cornea and to normalize refraction - the natural refraction of light rays passing through the cornea of the eye.
- Plastic transplantation allows you to restore the cornea locally or completely if there are defects on it, but while maintaining its function and structure.
- Cosmetic transplant. The operation is optional, but is performed to transplant a transparent cornea when the patient’s natural one is cloudy (this happens with complete blindness).
For your information! Separately, keratoprosthetics is distinguished. This is a transplant of a combined material made from donor tissue and rigid plastic material in the central part. Such operations are usually performed to strengthen the cornea as much as possible, for example, after previous unsuccessful keratoplasties.
Interventions are carried out in two ways: traditional surgical and more modern and laser. The first option requires high professionalism and experience of the doctor working with the instruments. The laser method is characterized by maximum precision, therefore it allows for manipulations of any complexity, cutting out areas according to the given individual parameters of the patient.
Anatomy of the cornea
Before considering the main aspects of keratoplasty, it is necessary to understand the anatomical and functional features of the cornea of the eye.
As mentioned above, the main functional load of the described part of the eye is the joint refraction of the lens with the lens to adequately focus the rays on the retina. We must not forget the protective role - the cornea is a barrier to small foreign bodies, as well as a natural filter against radiation. It consists of five layers, the thickness in the central region is about 550 microns, at the periphery – 650 microns. Let's take a brief look at each of the layers:
- Epithelium (50 µm) - the outermost layer, consists of 5-6 rows of flat epithelial cells.
- Bowman's layer (10 µm) is an acellular structure consisting of homogeneous collagen fibers, located directly under the epithelium.
- Stroma (450 µm) – plates of collagen fibers correctly organized in space. It is this anatomical arrangement that allows us to achieve transparency and elasticity, which is necessary for light refraction.
- Descemet's membrane (12 µm) is a very thin but elastic basement membrane of the endothelium.
- Endothelium (10 µm) is the innermost layer, consisting of a single row of cuboidal epithelial cells. An important functional role of endothelial cells is to maintain corneal transparency by controlling fluid balance. This cellular material does not have the ability to regenerate; the only way to restore vision after damage is keratoplasty.
Preparatory activities
Preparation for refractive layer-by-layer or through-and-through surgery includes examining the patient to assess the condition of his eyes and body. Indications and contraindications, the type of transplantation (end-to-end or layer-by-layer) are determined. For diagnostic purposes, the doctor prescribes specialized procedures: biomicroscopy to check all structures of the eye, pachymetry to measure thickness, scraping and biopsy of the membrane for subsequent microbiological and bacteriological studies. A blood test (general, for infections), examinations by a therapist and other specialists are also prescribed.
At the patient preparation stage, the affected areas of the cornea of the eye, their diameter, shape, volume and other parameters are also determined. This is necessary for the subsequent formation of a graft of the required size. If a patient is counting on donor tissue, he is put on a waiting list. The waiting period depends on the desired characteristics of the graft. When choosing artificial material, the wait is usually less long.
Your doctor will give you detailed recommendations for preparation. If the patient is taking blood thinners, they may be temporarily stopped or changed. You should not eat food on the day of surgery. Preliminary hospitalization in a hospital is not required.
Materials for transplantation
End-to-end or layer-by-layer surgery is carried out using either donor tissue or synthetic materials (artificial). The latter option began to be used relatively recently, only in the 21st century. It has a higher survival rate and minimal risk of rejection.
Tissue is collected from the donor either posthumously within 24 hours, or after brain death is determined while cardiac activity is preserved. Healthy patients without serious illnesses are eligible to receive a donor transplant. Tissues from infants and elderly people over 70 years of age are not used.
History of corneal transplantation
The history of keratoplasty – cornea transplant operations – is quite extensive; ophthalmologists have been working on a similar task for several centuries. The first successful corneal transplant was performed on December 7, 1905 by Eduard Zirm. This technology was deeply introduced in the 1930s in the USSR by ophthalmologist Vladimir Filatov.
Currently, more and more patients need various types of corneal transplants, on the one hand, due to the increasing variety of corneal pathologies, and on the other hand, due to technological improvements in medical care in this aspect. The need for such interventions is growing exponentially.
Currently, such operations are high-tech and are carried out using the latest generation equipment and take 20-30 minutes. They are performed under both local and general anesthesia. The postoperative period is characterized by minimal discomfort and, in the case of lamellar keratoplasty, a minimal postoperative period of several days.
The material for keratoplasty is corneal-scleral flaps - medical devices placed in a special preservative environment.
Progress of the operation
Refractive transplantation (both end-to-end and layer-by-layer) is more complex than other areas of ophthalmic surgery. The operation, which can be viewed on video, includes the following steps:
- The patient sits on a chair or lies down on a couch, fixes his head on a special holder;
- Anesthesia is administered. Local anesthetic drops are usually used, but at the patient’s request (or if there is a direct indication), the surgeon can perform the operation under general anesthesia;
- An eyelid expander is installed;
- The doctor begins the operation and begins performing manipulations. With refractive laser keratoplasty, the actions are performed with a laser beam. With the traditional surgical method, incisions are made with a thin scalpel or a special vacuum or manual trephine. Penetrating keratoplasty involves cutting through the cornea of the eye. With layer-by-layer plastic surgery, the cornea is cut into half or three-quarters, then exfoliated with a keratome;
- Then the excised area is removed, and donor or synthetic material is transplanted;
- Synthetic delicate cross-shaped continuous sutures are applied along the edges with a strong thread;
- Sometimes a special treatment lens is installed to protect the eye;
- A local antibiotic is instilled.
Duration ranges from 40-60 minutes to several hours (depending on complexity). The operation can be performed on an outpatient basis without hospitalization. In this case, after assessing the results and condition, if there are no problems (if everything went easily and without complications), the patient can go home. If the intervention was complex, the person operated on remains in the hospital for some time.
Corneal diseases
Corneal diseases occur in 25% of patients visiting an ophthalmologist. The cornea is the transparent membrane of the eye, 10-12 mm in diameter, which, like a watch glass, covers the colored structure of the eye called the iris.
A decrease in the transparency of the cornea, leading to loss of vision, can be due to many reasons: burns and eye injuries, keratitis and corneal ulcers, primary and secondary corneal dystrophies, keratoconus and keratoglobus. These corneal injuries and diseases require surgical treatment.
DIAGNOSIS OF CORNEA DISEASES
TREATMENT
In the surgical treatment of corneal diseases, two main directions can be distinguished: keratoplasty (corneal transplant), when the damaged cornea is replaced with healthy donor corneal tissue, and keratoprosthesis - transplantation of an artificial cornea.
MNTK "Eye Microsurgery" has the most experience in Russia in performing keratoplasty: over 30 years of work, over 16,500 donor cornea transplants have been performed. The Eye Microsurgery MNTK operates the largest and most modern Eye Bank in Russia with the latest medical and technological support. The complex is the only medical institution in Russia where the keratoprosthesis method is widely used, using its own models of keratoprostheses.
Keratoplasty surgery is performed on patients with keratoconus, corneal dystrophies, corneal opacities, etc.
| Keratoplasty | The total treatment time for one eye is 14-21 days (preoperative examination 2-3 days, on the 4th day - surgery ( the timing of the operation depends on the availability of donor material ), postoperative follow-up treatment - 10 days) |
To treat corneal cataracts, keratoprosthesis surgery is performed.
| Keratoprosthetics | The total treatment time for one eye (one stage) is 5 days (stage 1: strengthening the cataract and implanting support elements, preoperative examination 2 days, surgery on the 2-3rd day, postoperative observation - 1-2 days; 2nd stage implantation of a keratoprosthesis (3-4 months after the 1st stage).The duration of the operation is the same as at the 1st stage. |
Keratoplasty and keratoprosthetic operations are performed on an inpatient basis and usually take from 30 minutes to 1 hour. In the operating room you will be accompanied by a surgeon, his assistant, an operating room nurse, an anesthesiologist and a nurse anesthetist. Modern methods of anesthesia used in the MNTK “Eye Microsurgery” make it possible to completely eliminate pain.
The operations are performed by highly qualified surgeons from the Department of Transplantation and Optical Reconstructive Surgery of the anterior segment of the eyeball using the most modern equipment from the world's best manufacturers.
, new technologies for the surgical treatment of corneal dystrophy and keratoconus have begun to be widely used at the Eye Microsurgery International Scientific and Research Center .
- Deep anterior layer keratoplasty, which allows you to preserve your own healthy endothelium and avoid opening the eyeball (depressurization), reduce surgical and postoperative complications and the risk of graft rejection.
- Posterior lamellar endothelial keratoplasty, intended for the treatment of corneal dystrophy, allows the portion of donor tissue to be minimized, which reduces the risk of rejection and preserves most of the native cornea.
- Reconstruction of the anterior segment of the eyeball with implantation of an artificial iris based on penetrating keratoplasty in cases of severe corneal trauma combined with loss of the lens and iris.
- An alternative to penetrating keratoplasty for initial and advanced stages of keratoconus is introstromal keratoplasty with implantation of segments. The operation is performed in the early stages of keratoconus, has an orthopedic function, strengthens the thinned area, improves visual acuity, and stops the progression of keratoconus.
- Cross-linking of corneal collagen (cross-linking) slows or stops the progression of keratoconus based on biochemical remodeling of the cornea.
Improvements in microsurgical techniques and instruments, the emergence of new advanced equipment, and new approaches to pre- and postoperative therapy have expanded the range of surgical interventions on the cornea and provided a large percentage of favorable outcomes and high results.
MODERN METHODS OF DIAGNOSIS AND TREATMENT OF KERATOCONUS
KERATOCONUS
Keratoconus is a progressive dystrophic disease of the cornea, caused by a number of genetic and acquired factors, characterized by progressive thinning of the cornea with protrusion of its central parts, the formation of myopic refraction and irregular astigmatism. The etiology of keratoconus and other types of keratoectasias is currently unknown. Active progression of keratoconus occurs in 20% of cases and, as a rule, begins during puberty. The progression of the disease leads to a significant decrease in visual acuity and the ineffectiveness of methods for its correction. Making a diagnosis, especially in the initial stages of the disease, is very difficult. The most informative study at the moment in diagnosing this terrible disease, along with generally accepted research methods, is the performance of a scanning keratotopograph PENTACAM (OCULUS, Germany), which makes it possible to evaluate both the anterior and, most importantly, the posterior surface of the cornea - since this is where the initial anatomical changes occur. topographic characteristics in the initial stages (Fig. 1).
Rice. 1. Scanning keratotopograph PENTACAM (OCULUS, Germany).
Treatment of keratoconus
Depending on the stage of the disease and some important anatomical and topographical characteristics, the ophthalmic surgeon, based on many years of experience and the latest scientific developments of the Eye Microsurgery Institute, will offer the optimal treatment method. There are three main treatments for keratoconus:
Crosslinking of corneal collagen (Fig. 2)
The idea of using a conservative method of treating keratoconus was born in Germany by a group of researchers at the Technical University of Dresden. T. Seiler and G. Wollensak took as a basis the principle of photopolymerization, which has long been used in dentistry (“light filling”). As a result of a series of works, the most effective and safe technique for cross-linking corneal collagen was developed, based on the effect of photopolymerization of stromal fibers under the influence of a photomediator (riboflavin solution) and low doses of ultraviolet radiation from a solid-state source. This technique makes it possible to stop the progression of keratoconus and avoid end-to-end corneal transplantation.
Rice. 2. Crosslinking of corneal collagen
Indications:
- Keratoconus stages I-II.
- Keratoectasia after refractive excimer laser interventions.
- Corneal marginal degeneration
- Keratomalacia of various origins - cornea melting, usually during autoimmune processes.
- Keratoglobus.
- Bullous keratopathy stages I-II.
- There is encouraging data on the use of cross-linking in the treatment of keratitis and corneal ulcers.
Contraindications:
- Intolerance to Riboflavin (Vitamin B2).
- If the thickness of the cornea in at least one dimension is less than 400 microns.
- Age less than 15 years
- Low corrected visual acuity in keratoconus, despite sufficient thickness.
- Presence of corneal scars.
- The presence of allergic conjunctivitis.
Implantation of intrastromal corneal segments
In our practice, we use domestic IRS manufactured at Scientific and Experimental Production LLC "Eye Microsurgery" from polymethyl methacrylate, which is a segment with an arc length of 160 ° (90, 120, 160, 210 °), base 0.6 mm, height 150 - 450 µm, internal diameter 5.0 mm and external 6.2 mm, with a hemispherical cross section (Fig. 3).
Rice. 3. Intrastromal corneal segment
Correction of keratoconus and high-degree complex myopic astigmatism. First, a corneal tunnel is formed in the cornea, through which a corneal segment is inserted, which leads to flattening of the central zone of the cornea. An important aspect of this operation is its reversibility – i.e. the possibility of replacing or removing a segment if vision changes with age. This is possible because the center of the cornea is not damaged and no corneal tissue is removed. The next day after the operation, the patient’s eye is absolutely calm and after a short rehabilitation the patient can resume everyday visual stress (Fig. 4 It should be noted that implantation of intrastromal segments does not affect the patient’s cosmetics and allows him to use soft contact lenses. Depending on the indications, a combination is possible cross-linking and introstromal implantation of corneal segments.
Rice. 4. Patient's eye the day after implantation of the corneal segment
3.Keratoplasty
Recently, the method of choice for surgical treatment of keratectasia in advanced stages of the disease has often become anterior deep lamellar keratoplasty, during which the corneal stroma is peeled off from Descemet's membrane. At the same time, the increase in visual acuity is comparable to that after penetrating keratoplasty. The advantages of anterior deep lamellar keratoplasty over penetrating keratoplasty are: preservation of the endothelium of the recipient's cornea, which reduces the risk of graft rejection; reducing the risk of developing cataracts in the postoperative period due to the administration of a shortened course of steroid therapy; reducing the requirements for the donor graft, since the quality of its endothelium in this case does not play such a significant role as in penetrating keratoplasty.
It should be noted that the best results can be obtained when performing keratoplasty - both penetrating and anterior deep layer-by-layer with the use of femto-laser support, which ensures ideal cutting accuracy and unsurpassed compatibility of the cut donor graft and the recipient bed, leading to a significant increase in the visual functions of patients . Thus, currently, a qualified ophthalmic surgeon has a wide range of surgical methods for treating keratoconus. However, it should be noted that the most effective treatment is considered to be in the early stages of the keratectic process, which is possible with timely correct diagnosis of the keratectasis. The most effective modern methods for early diagnosis of the keratecstatic process are: computer keratotopography, optical coherence tomography, confocal scanning microscopy, immersion confocal microscopy, analysis of elevation maps. Our institute is equipped with the most advanced equipment for the early diagnosis of keratoconus, which allows us to detect keratoconus, even at the earliest stages of development, in 100% of cases. It should also be noted that the abundance of different methods for treating keratoconus poses the task of choosing the most effective method of treatment for each individual patient. The leading specialist of our institute is Doctor of Medical Sciences. Svetlana Borisovna Izmailova, based on a comprehensive analysis of the results of treatment of patients with keratoconus, developed an algorithm for the surgical treatment of keratoconus, which allows systematizing approaches to the treatment of keratoconus and differentially selecting the most optimal and effective method of treatment depending on the stage of the disease. Thus, the MNTK “Eye Microsurgery” presents the entire range of modern therapeutic and diagnostic technologies, allowing pathogenetically oriented treatment for each patient with keratoconus at any stage - from initial to acute. We can help everyone!
Our specialists:
Malyugin B.E. – Doctor of Medical Sciences, Professor. Performs operations on mechanical and femtolaser implantation of corneal segments, various types of keratoplasty, including layer-by-layer. Proficient in technologies for intraocular correction of residual myopia and astigmatism in patients with stabilized keratoconus.
Izmailova S. B. – Doctor of Medical Sciences Performs implantation of corneal segments, including femto-assisted, UV cross-linking, penetrating and lamellar keratoplasty - mechanical and femto-laser assisted. Proficient in technologies for intraocular correction of residual myopia and astigmatism in patients with stabilized keratoconus.
Kostenev S.V. – Doctor of Medical Sciences Performs implantation of corneal segments with femto-laser assistance and UV crosslinking. Performs PRK to correct residual ametropia.
Kovshun E.V. – Ph.D. He specializes in the treatment of advanced stages of keratoconus using penetrating and lamellar keratoplasty, and performs implantation of corneal segments and UV crosslinking.
Volkova O.S. – Ph.D. Performs implantation of corneal segments, including with femto-laser assistance, and penetrating keratoplasty.
Golovin A.V. – Ph.D. Performs femto-laser implantation of corneal segments.
Pashtaev A.N. – Ph.D. Performs femto-laser implantation of corneal segments.
Moroz O.V. – Performs implantation of corneal segments.
Contact us! We will help you!
YOUR DOCTORS
Rehabilitation
The rehabilitation period is quite difficult and long. The timing and speed of restoration of the patient’s visual functions depend on the initial pathology of the organ, the success of engraftment, the doctor’s experience, general health and other factors. Complete healing occurs within a year. The stitches are removed no earlier than six months later. In the first months, vision may deteriorate, which is gradually restored.
During rehabilitation, some restrictions apply:
- In the first 7-14 days, you should not get your eyes wet.
- Avoid any contamination.
- Mechanical influences must be excluded.
- UV protection when going outside.
- Reducing eye strain. You should read less, work on the computer, and use gadgets.
- Limit any activity in the first month, and heavy physical activity until complete healing (for a year).
- Regular visits to the doctor.
- Refusal to visit baths, swimming pools, saunas for a year.
- Refractive correction method with glasses.
The surgeon will give you more detailed and clear instructions.
Corneal pathology
The cornea is a unique optically transparent lens, the first to encounter an aggressive environment, conducts and refracts rays in a special way, and participates in maintaining the shape of the eyeball. Despite the high regenerative potential of corneal epithelial cells, it is an absolutely transparent structure, which is achieved by passive nutrition of this organ, which does not have its own vessels.
It is this amazing organ that is often susceptible to a huge range of diseases, risks and dangers associated with the loss of this unprecedented transparency: here is a wide variety of hereditary forms of corneal dystrophies, senile degenerations, injuries, burns, post-inflammatory changes, consequences of iatrogenic interventions, keratoconus, etc. The result of the listed diseases and their consequences is a violation of transparency, and, as a consequence, a persistent decrease in visual functions with absolutely healthy other optical environments and a well-functioning retina.
Is there a possible complication?
Complications can occur, and their development is usually caused by medical errors, non-compliance with the recommendations given by the surgeon, as well as the individual characteristics of the human body.
One or more of the following complications may occur:
- rejection of the material, accompanied by pain, swelling, turbidity, discharge (occurs rarely - in 5-25% of cases, usually within the first month, less often - for six months);
- long-term healing and recovery;
- increased intraocular pressure (up to glaucoma);
- bacterial or fungal infections;
- cataract;
- keratoconus;
- failure, suture divergence;
- inflammation of different parts of the eye;
- iris prolapse, lens displacement.
If any complication occurs, you must immediately show the operated eye to the surgeon. So, in case of rejection, glucocorticosteroids should be applied topically every day, as prescribed by a doctor, several times. In case of infection, antibacterial drops are prescribed. Sometimes repeated intervention is required.
Where is keratoplasty performed?
The refractive correction method through keratoplasty is carried out in special ophthalmological centers located in Moscow and other Russian cities. And it is important to choose a clinic with an impeccable reputation, numerous positive reviews, and a license to carry out medical activities. The center must also be equipped with modern new equipment.
Pay attention to the choice of surgeon:
he must have a lot of experience, high qualifications and the necessary skills in keratoplasty techniques. Not all doctors perform such complex operations.
Our equipped modern clinic accepts patients with any eye diseases. We employ experienced and talented professionals. The center is equipped with all necessary equipment. You can make an appointment and receive advice, as well as qualified assistance.
Keratoplasty surgery allows you to restore the structure of the cornea of the eye or even restore vision. If you have corneal pathologies, contact the clinic: you may need a transplant.