Diode laser
Modern technologies are increasingly used in medicine. Today, laser treatment of periodontitis is commonplace. The healing properties of a narrowly targeted flow of energy are manifested in dentistry, creating the possibility of quick and painless dental treatment. The wide range of services provided with its help, coupled with relative affordability, contributes to the growing popularity of this method.
Treatment principle
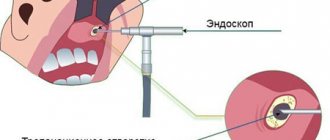
Laser treatment is based on the principle of local exposure of the beam to a specific type of tissue. The beam does not affect neighboring areas. Targeted action allows you to remove carious and inflamed areas without affecting healthy enamel, gum tissue and dentin.
Carious tissues contain more moisture. Under the influence of the laser, moisture evaporates from them intensively - tissues affected by caries are gradually destroyed. In 3-5 therapy sessions, the doctor removes all diseased tissue without affecting healthy areas.
When treating periodontitis, it is necessary to remove infected areas that have changed their structure. To do this, the dentist treats the gums with a special solution that reacts with the affected cells. The solution stains the pathological areas, after which the laser acts on them. It evaporates and destroys them without damaging healthy areas.
Principle of operation
By heating the surface of the tooth, most of the liquid is removed from it. After this, the “protected” inflamed space is released. The laser beam burns out all harmful microorganisms and frees up space for further mechanical cleaning.
Treatment of dental cysts with a laser is carried out similarly to any other operations. A cyst is a formation with dense, hard walls, inside of which there is a large amount of bacteria or dead tissue. Outwardly it may not be noticeable, but in everyday life it causes great discomfort. In particular, previously a dental cyst was treated with great effort.
This purulent sac forms in the roots, so to remove it, in any case, it would be necessary to remove the tooth, clean out the abscess and install an implant in its place. There is another method - surgical. To carry it out, an incision is made in the desired place of the gum, corresponding to the cyst, the dentist-surgeon uses instruments to pull out the bag, and then sutures the tissue.
Laser treatment is also used to treat periodontitis.
What dental diseases can laser treat?
The use of laser is equally effective in pediatric and adult dentistry. It is shown:
- in the treatment of caries;
- in bone and soft tissue surgery using a laser scalpel;
- when installing implants;
- in the treatment of inflammation and infections of the oral mucosa;
- when removing soft tissue formations;
- in the treatment of periodontal disease and periodontitis;
- as a prevention of oral diseases.
Indications for use
- Primary carious lesions in the area remote or close to the pulp;
- Secondary carious lesions that contain composites (smaller cavities or remains of composite) or cements;
- Conditioning the dentin surface to improve the adhesion of fillings in cavities that have been prepared using a laser or rotary instrument;
- Preventive sealing of molars and premolars not affected by caries;
- Extended fissure sealing after preliminary preparation of carious fissures;
- Reducing the number of microorganisms in the root canal after mechanical treatment during vital extirpation or treatment of an infected canal.
Benefits of laser therapy
Laser therapy has many advantages over traditional treatments. Let's list the main advantages.
- The laser beam acts locally and briefly, without irritating the dental nerves or causing thermal reactions, so patients do not feel pain.
- The painlessness of the treatment allows you to eliminate or reduce the amount of painkillers, which is important for patients with intolerance or hypersensitivity to anesthesia.
- The laser does not produce unpleasant sounds characteristic of a drill - patients in the dental chair do not experience stress.
- In combined treatment regimens, laser radiation enhances the effects of medications and increases the effectiveness of treatment in general.
- Laser radiation is detrimental to pathological microflora, so there are no side effects, including inflammation and infection of healthy areas.
- The rehabilitation period is reduced by 2-3 times.
Contraindications to laser use
- Diseases of the cardiovascular system in the stage of decompensation
- Diseases of the nervous system with sharply increased excitability
- Hyperthyroidism
- Severe and severe emphysema
- Functional kidney failure
- Severe diabetes mellitus in an uncompensated state and with unstable compensation
- Oncological diseases
- Heavy bleeding
- Photodermatoses and the use of photosensitive drugs
High-quality equipment and training of specialists guarantee the safety of laser treatment of teeth and gums, as well as laser teeth whitening at Dial-Dent.
Laser whitening has a lasting result and is safe for tooth enamel.
Dental laser is an excellent additional tool in the treatment of many dental diseases. However, the use of a laser does not exclude traditional treatment methods, which are perfectly mastered by Family Dental specialists.
Diseases of hard dental tissues of non-carious origin
Hypoplasia, erosion and pathological abrasion of enamel are pathologies caused by neuroendocrine disorders or heredity. Doctors developed a universal rehabilitation program (URP) based on laser exposure and conducted a study in which 185 patients took part.
Each of them received 5-7 sessions of laser therapy with a pulse frequency of 50 Hz. The duration of the scanning effect varied from 1 to 5 minutes and covered the following areas:
- apex beat zone;
- epigastric zone;
- sternum;
- right and left hypochondrium;
- subclavian fossa;
- kidneys and adrenal glands;
- suboccipital fossae.
After treatment, 52 people experienced significant improvement in their overall health. They noted improved sleep, high resistance to stress, absence of pain, irritability, and fatigue.
As for the results of treatment of hard dental tissues, it occurred 10 days faster than in patients receiving drug treatment. 150 out of 185 patients got rid of not only the underlying disease, but also sinusitis, tonsillitis, and radiculitis.
Advantages of laser dentistry
One of the most important advantages of dental laser equipment is the absence of mechanical impact. Unpleasant sensations typical for treatment with a drill are eliminated, as is the occurrence of microdamages associated with vibration.
All operations are silent, but it is the buzzing of the drill that often puts patients in a stressful state.
With laser treatment of soft gum tissue, the incision sites are scarred much faster than with conventional surgical methods, since the incision is sterilized and instantly sealed. The duration of all operations is significantly reduced.
The laser has a powerful healing effect when removing a tooth. The operation itself is performed with conventional instruments, like any other extraction, but the tissue flaps cut by the beam are minimally injured, which significantly reduces the intensity of bleeding and speeds up healing.
The laser is also used in prosthetics to form a ledge above the gum, where the tooth tissue passes into the crown. The line turns out very clear, and the result pleases with its high quality.
The main advantage of using a laser in implantology is the precise thinness of the beam, which narrows the size of the surgical trauma inflicted on the patient. Damaged capillary blood vessels are sealed instantly due to targeted thermal effects.
Laser whitening is based on the principle of splitting pigments in dentin, which leads to almost complete discoloration of all coloring substances deeply embedded in the enamel structure.
Treatment of caries
Caries is the destruction of hard tooth tissue due to chemical exposure and the activity of pathological microflora.
Another example from practice. 270 patients underwent laser treatment, and Moscow dentists diagnosed multiple caries in 150 of them. The treatment was carried out using a RIKTA laser therapy device using dental attachments. Doctors acted on the affected teeth for 1-2 minutes with a pulse frequency of 50 Hz.
In case of multiple caries, radiation was applied to the submandibular and parotid glands. This effect stimulates the production of immunoglobulin and reduces the viscosity of saliva. The duration of the procedures is 2 minutes, with a pulse of 50 Hz.
Each patient received a course of 8-10 laser therapy sessions. Over the next year, 86% of patients did not develop caries. For comparison, in patients undergoing traditional treatment, this figure was 61%.
Experience in using an erbium laser with feedback in the treatment of periodontal diseases
A. A. Glotova
periodontist at the Dental Lux dental clinic (Krasnodar)
E. N. Shastin
Professor of RAE, Head of the Dental Lux dental clinic (Krasnodar)
Just a few decades ago, treatment of carious lesions was the focus of the dental community, but periodontal disease is now the leading cause of tooth loss and bone loss in patients over 35 years of age. For this reason, the development of diagnostic and therapeutic procedures represents one of the most pressing problems in periodontics. With the advent of lasers in this area, interesting prospects have emerged that, in our opinion, will significantly change routine periodontics.
Chronic periodontitis is the most common form of periodontitis. This infectious and inflammatory disease of the supporting apparatus of the tooth occurs with progressive loss of attachment and resorption of the alveolar bone, the formation of a periodontal pocket, and can also lead to recession. The etiological factors are periodontopathogenic microflora and subgingival tartar.
The main goal of periodontitis treatment is to remove calculus from the root surface and eliminate microorganisms that cause destruction of periodontal tissue. A prerequisite is the creation of a clean, biocompatible and as smooth root surface as possible and the removal of destroyed or infected tissue. The superficial cementum layer of the infected root contains endotoxin. This is a lipopolysaccharide of gram-negative bacteria, which suppresses regenerative processes in connective tissue and prevents the periodontal ligament from reattaching to the root surface.
Antimicrobial, anti-infective treatment comes down not only to careful scraping of the surfaces of roots and pockets. It is also necessary to reduce the number of bacteria inhabiting the pocket and eliminate particularly pathogenic microorganisms.
In the treatment of periodontitis, constant monitoring of the patient's motivation, root planing, surgical procedures and antibiotics are the main methods. A valuable addition, both in conventional and surgical therapy, is the use of various laser systems.
Scaling and root planing (SRP) is an essential measure that effectively removes bacterial biofilm and tartar from the root surface. SRP can be performed using manual curettes. This technique requires considerable clinical skill, and sometimes the root anatomy complicates the task. Moreover, excessive cementum removal may result in increased subgingival surface roughness, which increases plaque accumulation. Sonic and ultrasonic scalers for SRP are also available. Several studies have reported improved effectiveness of ultrasonic scaling for calculus removal, particularly at furcation sites. However, complete removal of subgingival calculus cannot be achieved with non-surgical instrumentation by any method. In recent years, the use of laser light has been proposed as an alternative or adjunct to standard periodontal therapy. Various advantages such as hemostatic effect, controlled plaque removal and bactericidal effect against periodontal pathogens lead to improved treatment results.
The erbium laser system has great potential for effectively removing tartar from the surface of a damaged root without simultaneously overheating the surrounding tissues due to the high degree of absorption of its radiation energy (2940 nm) by water. The so-called thermomechanical, or photomechanical, effect is the basis of the tissue ablation mechanism, in which water molecules in solid tissues turn into gas when energy is absorbed. Consequently, interstitial pressure increases, which leads to ablation.
The principles of wound healing after non-surgical or traditional surgical periodontal treatment for the Er:YAG laser are as follows: it does not cause significant thermal side effects and leads to a decrease in inflammatory cell infiltration and matrix metalloproteinase-8 reactivity compared to ultrasound. Some laser damage to the root surface showed the formation of new cementum with interweaving of type 1 collagen fibers.
Professor Schwartz conducted research to study the effect of the Er:YAG laser on the surface of the root with damaged periodontium. 160 roots were treated with an Er:YAG laser: in natural conditions - 80; 80 - immediately after extraction. Energy settings range from 120 to 180 mJ. The treated root surfaces were examined under an electron microscope.
In vitro, the treated surfaces showed crater-shaped defects that reached the dentin with higher energy levels. In comparison, root surfaces treated under natural conditions showed a uniform and smooth morphology, with surface changes not correlating with energy level elevation.
The authors concluded that clinical application of the Er:YAG laser even at higher energy settings in vivo is possible. The effectiveness of the Er:YAG laser in stone removal is comparable to that of hand instruments. In addition, periodontally damaged teeth whose root surfaces were irradiated with an Er:YAG laser showed significantly higher biocompatibility in human PDL fibroblast cultures compared to those treated with manual or ultrasonic equipment alone. This may be due to the absence of a smear layer after laser therapy.
(Fig. 1a) (Fig. 1b) (Fig. 2)
(Fig. 3a) (Fig. 3b) (Fig. 4)
Rice. 1 a, b. The patient came to the clinic with complaints of bleeding, burning gums, and tooth mobility.
Rice. 2. Periodontal examination.
Rice. 3 a - c. Diagnosis: chronic generalized severe periodontitis (type 2B).
Rice. 4. Initial therapy.
The Er:YAG laser is able to remove calculus at 100 mJ, with root surface roughness comparable to that observed with manual scaling. The temperature rise in the pulp can be called tolerable (no more than 4.5 ° C), water cooling is also available and the 15 s interval is observed, while the damage caused to hard and soft tissues is negligible.
In terms of the absolute amount of solids removed, there is a clear relationship with the energy used and the angle of the nozzle relative to the root. The higher the power value and the more obtuse the angle between the nozzle and the root surface, the more material is removed.
(Fig. 5a) (Fig. 5b) (Fig. 6a)
(Fig. 6b) (Fig. 7a) (Fig. 7b)
Rice. 5 a, b. Treatment with handpiece P 2061.
Rice. 6 a, b. Condition after 3 days.
Rice. 7 a, b. Condition after 7 days.
The bactericidal effect of the Er:YAG laser on periodontopathogenic microbial flora was also the subject of an in-vitro study by Folwaczny et al. The root surfaces of 125 extracted teeth were inoculated with a suspension of Escherichia coli, Staphylococcus aureus, Actinobacillus actinomycetemcomitans, Eikenella corrodens and Peptostreptococcus micros. This was accompanied by laser irradiation at various energy parameters. Bacteriological assessment revealed a high bactericidal effect of the Er:YAG laser on the studied microorganisms.
The KaVo KEY 3 erbium laser used in our clinic has Feedback System technology. Feedback System is an intelligent feedback system. A 655nm InGaAsP (indium gallium arsenium phosphorus) diode laser was incorporated into an Er:YAG laser to induce fluorescence in subgingival calculus. When a low-power diagnostic beam (pilot beam) hits tissues containing pathogenic microorganisms, a fluorescent glow appears and the laser emits a sound signal. The glow is registered by an electronic system, and a control pulse is generated that turns on the laser. If the fluorescent signal is above the threshold level, then the laser is activated to remove infected tissue (subgingival deposits), and if the signal is below the threshold level, the laser beam is turned off, that is, if the root surface is cleared of stones, the laser stops and the sound disappears. The display also has a constant digital display, the indicators of which help the doctor determine the size of subgingival deposits and residual plaque. Thus, it becomes possible to remove stones from the root surface without damaging healthy tooth tissue. The controlled illumination (feedback system) showed effective removal of subgingival calculus in preliminary histological results and predictable protection of the root surface in comparison with manual instruments. The use of an erbium laser with feedback eliminates the most important disadvantage of closed curettage, “working blindly,” that is, the lack of controlled removal of subgingival dental plaque: with standard instrumentation, the doctor is guided only by manual skills.
Thanks to all of the listed properties of the erbium laser with feedback, its use in the treatment of periodontal diseases can improve treatment results compared to standard non-surgical instrumentation and significantly reduce the need for surgical methods for the treatment of periodontitis.
Clinical case No. 1
The patient came to the clinic with complaints of bleeding, burning gums, and tooth mobility (Fig. 1 a, b).
Vestibularly, in the area of the 16th tooth, there is a painful round formation on the gum, there is a fistulous tract, upon probing of which purulent discharge is obtained. On palpation, the pain intensifies, purulent discharge comes out through the fistulous tract and the vestibular periodontal pocket of the 16th tooth. The greatest probing depth was 9 mm vestibular-mesial. In addition, there is a lesion of the furcation on the buccal side of the 16th tooth of the 3rd degree. Mobility 1st degree (Periotest +15).
A periodontal examination was carried out using the Florida Probe hardware and software complex (Fig. 2).
Horizontal resorption of bone tissue along ½ the length of the tooth root. Vertical bone pocket mesially. Loss of the vestibular cortical plate, damage to the furcation between the mesial and distal buccal roots of the 3rd degree.
(Fig. (Fig. 9a) (Fig. 9b)
(Fig. 9a) (Fig. 9b)
(Fig. 10a) (Fig. 10b)
Rice. 8. Periodontal examination after 3 months.
Rice. 9 a - c. X-ray examination after 1 year. Rice. 10 a, b. Examination before treatment and 3 months after initial therapy.
Diagnosis: severe chronic generalized periodontitis (type 2B) (Fig. 3 a - c).
Initial therapy (Fig. 4):
- Professional oral hygiene.
- Closed curettage using Er:YAG laser.
- Antiseptic treatment with solutions of 0.05% chlorhexidine, 3% hydrogen peroxide.
- Total FotoSan therapy.
Treatment was carried out with a P 2061 handpiece, power 120 mJ, frequency 10 Hz, at an angle of 15-20° relative to the tooth axis (Fig. 5).
A periodontal examination using the Florida Probe hardware and software complex took place 3 months after treatment (Fig. 8).
X-ray examination was completed after 1 year (Fig. 9).
Conclusion: thanks to the correction of individual hygiene, high motivation for treatment in the patient and the use of the Er:YAG laser, we were able to reduce the number of periodontal pockets by 60% already 3 months after the start of treatment, achieve remission and change the prognosis of tooth 16 from poor to satisfactory using exclusively conservative methods methods of treatment.
Clinical case No. 2
A 32-year-old patient came to the clinic with complaints of pain and bleeding in the area of the chewing teeth on the upper and lower jaws. A periodontal examination was carried out using the Florida Probe hardware and software complex, tooth mobility was determined using the Periotest device, and cone beam computed tomography was performed. Diagnosis: aggressive localized severe periodontitis (type 3A).
Initial therapy:
- Professional oral hygiene.
- Closed curettage using Er:YAG laser. Treatment was carried out with a P 2061 handpiece, power 120 mJ, frequency 10 Hz, at an angle of 15-20 ° relative to the tooth axis.
- Antiseptic treatment with solutions of 0.05% chlorhexidine, 3% hydrogen peroxide.
- Total FotoSan therapy.
Examination before treatment and 3 months after initial therapy (Fig. 10 a, b).
The patient refused the proposed surgical treatment.
X-ray examination before treatment and 6 months after initial therapy. Area 36, 37 teeth (Fig. 11 a, b).
X-ray examination before treatment and 6 months after initial therapy. Area 16, 17 teeth (Fig. 12 a - d).
X-ray examination before treatment and 6 months after initial therapy. Area 26, 27 teeth (Fig. 13 a - d).
Conclusion: despite the patient’s refusal to undergo surgical treatment and the unfavorable prognosis of teeth 16, 26, 27, 36, thanks to the use of the Er:YAG laser we were able to save all teeth and achieve bone tissue formation without regenerative surgeries and a significant reduction in attachment loss.
When a low-power diagnostic beam (pilot beam) hits tissues containing pathogenic microorganisms, a fluorescent glow appears and the laser emits a sound signal. The use of the Er:YAG laser with feedback in periodontics is just beginning. The advantages outweigh the disadvantages. Laser is definitely an alternative to standard treatment as it provides almost painless and fast treatment. The disadvantage of using the Er:YAG laser is that it leaves micro-roughness, but this cannot be eliminated using other methods. Also, the disadvantages of the Er:YAG laser include expensive equipment, the need for a periodontist to have special skills and theoretical knowledge to use this technique. This only means that each method has its drawbacks.
(Fig. 11a) (Fig. 11b) (Fig. 12a)
(Fig. 12b) (Fig. 12c) (Fig. 12d)
(Fig. 13a) (Fig. 13b) (Fig. 13c)
(Fig. 13d)
Rice. 11 a, b. X-ray examination before treatment and 6 months after initial therapy. Area 36, 37 teeth.
Rice. 12 a - d. X-ray examination before treatment and 6 months after initial therapy. Area 16, 17 teeth.
Rice. 13 a - d. X-ray examination before treatment and 6 months after initial therapy. Area 26, 27 teeth.
At the same time, the Er:YAG laser has an excellent bactericidal effect against periodontal pathogenic microflora. The feedback system allows for controlled removal of subgingival deposits. The Er.YAG laser thus facilitates stone removal and offers better conditions for fibroblast adhesion than conventional instrumentation. The presence of water cooling eliminates thermal damage to tissues. Thanks to all these properties, the use of an Er:YAG laser in the treatment of patients with severe forms of periodontitis can significantly reduce the indications for surgical procedures, which makes it possible to achieve good results in the treatment of periodontal diseases using minimally invasive methods.
How laser therapy affects tissue: biopsy results
Research on the effectiveness of laser therapy is carried out not only by measuring the effectiveness in patients, but also in laboratories, at the cellular level. One of these experiments made it possible to track changes in the cellular structure of the periodontium over 5 sessions of laser exposure and, based on its results, determine the effectiveness of therapy.
Histological and cytological studies of tissues before the start of treatment showed that the mucous membrane was affected by the inflammatory process, wound healing was sluggish, and there were practically no full-fledged cells.
After two laser sessions, the healing process intensified. After 4 sessions, the studied samples already showed signs of bright coagulations, a gradual restoration of erythrocytes and leukocyte cells.
After the 5th session of laser therapy, a biopsy showed the presence of full-fledged cells - red blood cells, leukocytes, and fibroblasts. The results indicate the patient's complete recovery.
Bactericidal action.
Periodontitis is an inflammatory disease in which bacterial flora plays a significant role. In all pathological pockets, there are conditions for the free existence of microorganisms. That is why the bactericidal effect when exposed to a diode laser during the treatment of periodontitis should not be underestimated. Multiple clinical studies have been conducted that have shown that the diode laser has an excellent bactericidal effect. It is important to note the ability of laser radiation to penetrate the tissues of the body and have an antimicrobial effect there too, because many pathogenic microorganisms penetrate into nearby gum tissue, and this, in turn, saves us from carrying out additional antibacterial treatment.
Advantages of contacting PROFI-Dent
PROFI-Dent is one of the best laser dentistry clinics in Moscow.
We can confidently be called a shining example of an exemplary modern dental practice that fully complies with international medical standards:
- advanced equipment;
- a team of experienced, competent doctors of all specialties;
- high quality of treatment;
- affordable prices for laser dentistry and other types of services;
- convenient location;
- Individual approach to patients in terms of treatment, payment process and specialist visit schedule.
Come to us and make your dream of a perfect smile come true!