The appearance of a fistula on the gum, or apical periodontitis, indicates advanced purulent inflammation in the area of the apex of the tooth root. The pathology is a painful convex neoplasm, rising above the periodontium, with a passage from which pus and blood are discharged. The affected area is localized next to the diseased tooth.
Fistula almost always occurs as a result of untreated pulpitis and caries. Over time, inflammation becomes chronic and is asymptomatic, but due to decreased immunity it enters the acute phase.
Reasons for appearance
- Caries and its complications (periodontitis, pulpitis, etc.). If not treated promptly, the infection penetrates deep into the root canal and affects the nerve and blood vessels in the pulp. Pulpitis occurs. If a person continues to ignore night pain and other symptoms, necrosis of the periodontium and bone tissue occurs, and a cyst forms. Due to tissue swelling and a large amount of exudate, a fistula appears through which there is a constant outflow of pus.
- Errors during treatment (irregularities during canal filling, etc.). Untreated or improperly treated pulpitis leads to periodontitis. This disease can also be caused by infections of periodontal pockets due to periodontitis and gingivitis, as well as infection during treatment or removal if aseptic rules are not followed. Another reason is poor-quality canal preparation and violation of the integrity of the root walls. Through the hole, bacteria enter the cavity and cause inflammation. The danger of the condition lies in infection of the soft tissues and periosteum surrounding the tooth.
- Granuloma. Inflammatory lesions of the periosteum and root apex develop over several weeks. At first there may be no complaints. The color of the tooth gradually changes, and pus accumulates inside. Against the background of illness or stress, the development of pathology sharply accelerates, which leads to the formation of a fistula. The temperature rises, the sublingual lymph nodes enlarge, and a sharp throbbing pain appears.
- Improper teething. An abnormal structure of the gums or too early loss of baby teeth can provoke the formation of a cyst, which gradually grows and leads to perforation of the soft tissue.
Types of gum fistulas
In modern dental practice, there are two types of gingival fistulas:
- external;
- internal.
An external fistula is a flow channel ending with a hole on the surface of the gum, through which purulent and other pathological masses are discharged into the patient’s oral cavity. In turn, internal fistulas are called passages that do not have access to the gum surface, do not interact with the external environment and remove pus from the source of inflammation into free anatomical spaces in the thickness of the tissue.
Treatment of fistula
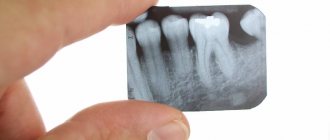
Before starting any therapeutic procedures, the doctor takes a picture of the affected area to determine the position of the fistula, the condition of the roots and the affected area. Treatment is carried out only in a clinic in several stages.
- To eliminate the inflammatory process and the source of infection, antibiotics are prescribed. The gums are also treated with antimicrobial gels, ointments, and aerosols.
- After treatment of inflammation and stabilization of the patient's condition, surgical treatment is performed. Under local anesthesia, the doctor excises necrotic tissue, treats the root canals and fills them, if it is still possible to save the tooth.
- Oral care, compliance with doctor’s prescriptions, limiting the consumption of hot or cold, spicy and salty drinks and food.
Treatment of gum fistula in pregnant women requires consultation with an obstetrician-gynecologist. When choosing therapy, possible risks of complications and damage to the health of the fetus are taken into account. If treatment is not possible, therapy to relieve symptoms until delivery is carried out.
Prevention of gingival fistulas
The main measures aimed at preventing the formation of gingival fistulas are:
- compliance with all requirements of individual oral hygiene;
- Regular visits to the dentist and professional teeth cleaning;
- proper nutrition;
- healthy lifestyle.
It is important to understand that the effectiveness of the treatment of fistulas on the gums directly depends on the timely detection of the pathological process and the establishment of the causes of its occurrence. It is for this reason that the detection of any symptoms indicating the presence of a fistula in the gum tissue is the basis for a visit to the dental clinic and receiving the necessary medical care.
Treatment of a fistula on the gum at home
It is impossible to treat a fistula without the help of a doctor. There are methods that can bring some relief if the pain strikes you at night and you cannot urgently see a dentist.
- rinsing with warm (your body temperature) infusion of chamomile and oak bark;
- for purulent discharge, rinsing with antimicrobial agents and a soda-saline solution is suitable.
Traditional methods should be completely abandoned, as there is a risk of spreading infection and worsening the situation.
Diagnostics
First of all, this is a visual inspection. An external fistula is visible to the naked eye. If the fistula in the jaw is hidden, an x-ray is taken. With the help of X-ray examination, the focus of inflammation and the depth of the pathological process of damage to the periosteum are accurately identified. It is important to distinguish a fistula from gum tissue, purulent tissue inflammation and other pathologies.
Self-medication of such a disease at home and self-diagnosis are unacceptable. Treatment is carried out under the supervision of a doctor, which he prescribes based on the diagnostic results.
Complications and prognosis
With timely treatment and following the dentist’s recommendations, there is a high chance of saving the tooth. In advanced cases, complications arise:
- osteomyelitis;
- phlegmon;
- granulomas;
- disruption of the gastrointestinal tract;
- sepsis.
The fistula does not go away on its own. Surgical and drug treatment is mandatory. When you contact the VIMONTALE clinic, you can be sure that you will receive professional assistance. The center's doctors use only the latest technologies and materials in their work.
Expert of the article you are reading:
Lozinskaya Alla Nikolaevna
Pediatric dentist, general dentist.
You may also be interested in:
Treatment of dental canals Dental treatment during pregnancy Dental consultation Treatment of dental cysts Increased sensitivity of teeth: causes and methods of treatment Filling of dental canals Treatment of pulpitis Treatment of flux (periostitis)
Show more
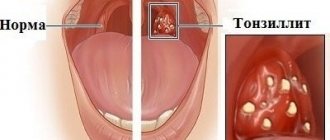
What is a fistula, what does it look like, symptoms
Externally, the fistula is a convex formation with a noticeable white spot on it. This means that the pathological process is accompanied by the formation of pus in large quantities.
There are two types of fistula:
- External, when the gum fistula comes to the surface;
- Internal, when the process remains hidden inside the gum, due to the fact that the fistula channel does not reach its surface. The inflammatory process can only be detected by x-ray examination.
Symptoms of a dental fistula are detected primarily by visual examination. There is a noticeable bulge on the gum, from where pus comes to the surface. There are other signs:
- The pain is cutting, stabbing, spasmodic. Becomes stronger with impact (for example, when chewing), weakens slightly after some of the purulent contents come to the surface;
- Putrid odor;
- Foreign tastes in the mouth;
- Tooth mobility with pathology;
- Swelling of the gums in the area of inflammation;
- Discharge of mucus with pus;
- Increased temperature, symptoms of intoxication of the body;
- Inflammation of the lymph nodes.
What causes the development of a fistula duct?
Fistulas extending into the intestines or anorectal area may be the result of the following diseases:
- Proctitis and paraproctitis. These diseases are accompanied by inflammation that spreads to the mucous membrane of the rectum and its fatty tissue.
- Crohn's disease. This disease causes inflammation in all parts of the gastrointestinal tract with the formation of granulomas.
- Sexual infections (syphilis, chlamydia, AIDS).
In women, an anorectal fistula can form after trauma received during a complicated childbirth. But the general cause is always the same - it is an inflammatory process, which is often a consequence of infection.
Paraproctitis: insidious fistula and false shame
This disease is one of those that people are embarrassed to discuss with friends and acquaintances. Moreover, the visit to the doctor is delayed from day to day. What can I say - it’s a shameful place, and that’s all... The disease is insidious with both severe physical pain and moral suffering. But this, unfortunately, is not all - without timely treatment, paraproctitis can poison a person’s life for many years, ultimately resulting in very dire consequences. And all because it was once awkward to cross the threshold of a proctologist’s office.
Anatoly Ivanovich Vanin, the head of the proctology department of the polyclinic of the Medical Center of the Administration of the President of the Russian Federation, Candidate of Medical Sciences, tells us why paraproctitis is dangerous and how to cure this disease - successfully and without false shame.
“Let me remind you that “para” in Greek means near, around, and proctitis is inflammation of the mucous membrane of the rectum,” said A.I. Vanin. — Thus, paraproctitis is an inflammatory disease of the tissue surrounding the rectal area, the lower part of the rectum.
The main reasons are stress, a decrease in the body's immune defense, a sedentary lifestyle, excessive use of antibiotics, severe hypothermia, nutritional errors, most often dry food, on the go, and as a result - constipation or, conversely, loose stools. Paraproctitis occurs regardless of age, but more often in men, because they smoke a lot and drink often. However, recently more and more women and girls are becoming ill: the desire to wear tight-fitting trousers, especially jeans made of thick, coarse fabric, as well as underwear, which, cutting into the crotch, injures the skin, is affected. Such abrasions become susceptible to infection, including viral infections. When hypothermia occurs - this is when girls flaunt in short skirts and thin tights in cold weather - herpes appears, which also provokes paraproctitis. Elderly people usually suffer from chronic paraproctitis if they suffered an acute form of the disease in their youth.
How does the disease occur? In the lower part of the rectum (in the anus) there are mucous glands that moisten the surface of the intestine with their secretions, facilitating the exit of feces if it is dry. With constipation, the mucous membrane is damaged, abrasions and cracks form, which become infected. Let me note that one gram of feces contains millions of units of different flora. This is where all the trouble begins.
The same thing happens when the stool is liquid - the acidic mass causes loosening of this area, also with possible infection. And even with normal bowel movements, something similar is possible - there seem to be no special complaints, but the body is weakened, and then the person just ate hot sauce, mustard, horseradish. The mucous membrane instantly becomes irritated and burns occur. The disease then develops according to a well-known scenario: the infection, along with inflammatory manifestations, spreads to the perirectal tissue - the connective tissue surrounding the rectum.
Paraproctitis begins with itching and slight discomfort in the anal area, then the disease gains momentum, purulent streaks form, which can turn into various fistulous forms and break out to the surface of the skin. If there is no breakthrough, the purulent mass comes out along with mucus and other unpleasant putrefactive discharges through the anus. Acute paraproctitis develops suddenly: the temperature rises, sharp pain appears in the rectal area, giving no rest, and after a sleepless night the person consults a doctor. True, there are erased forms of the disease - the patient does not seem to complain of severe pain, but the inflammatory infiltrate is palpable. In this case, to make an accurate diagnosis, you need to do an ultrasound, computed tomography or magnetic resonance imaging. A blood test alone is not enough, since the picture may be normal, although leukocytosis is sometimes observed.
In the chronic form of paraproctitis, fistulas do not heal for a long time. And then smears are taken from the patient to determine the cause of this protracted process, since the fistulous form of chronic paraproctitis can be caused by tuberculosis, syphilis, cancer, Crohn's disease, and other diseases. But more often the banal fistulous form is affected - with the release of E. coli and pus.
There are also internal incomplete fistulas, when the infection enters the anal fissure. Inflammation of perifocal tissue leads to abscess formation. The pus cannot come out due to the very dense thick skin. In this case, it is necessary to open and drain the abscess. If pus comes out through the internal opening of the fistula, then the discharge comes from the anus. Fistulas are located differently in all patients. In some - 2-3 cm from the anus - they can be felt with your fingers, seen in the mirror, in others - in the upper parts of the rectum.
The most common treatment for paraproctitis is ichthyol ointment and suppositories. They reduce tissue tension, relieve pain, help patients adapt to their condition; some even refuse surgery.
Initially, we try to puncture the abscess - release the pus, and then relieve the inflammation. The fistula is washed with a 1% dioxidine solution, and at the same time the patient is prescribed an anti-inflammatory drug - sumamed (0.5 g once a day for 3 days in a row). Fistula lavage is performed on an outpatient basis. Typically, after three procedures, the fistula closes in most patients. This is followed by taking medications that support the immune system.
But it happens that the fistula remains, however, without obvious purulent discharge. Treatment continues at home. Sitz baths are recommended: 1 tbsp. spoon of sea salt and baking soda per 5 liters of warm water. The duration of the bath is 10 minutes. Such procedures help the discharge of pus and clean the fistula well. After the bath, suppositories or ultraproct ointment are introduced. You can make microenemas from mumiyo: dissolve 1 tablet in 0.5 cups of hot water, administer warm.
I’ll tell you about one amazing case of recovery, which was helped by... a honey fair organized by Moscow Mayor Yuri Luzhkov in Manege. The patient came to us for procedures for a whole month, and to no avail: there was no pus, but the fistula remained. Here we just received information from this fair about the healing properties of sweet clover honey. They began to give the patient microenemas - 1 tbsp. a spoonful of honey in 0.5 cups of water. And everything healed in two days. Just a miracle!
I must note that such enemas - both with honey and with propolis oil solution - are very effective. The intestine even begins to squelch with pleasure: she likes warm, sweet things so much! Microclysters (1 tablespoon per 0.4-0.5 glasses of water) are done at night, and in the morning after stool, UltraProct suppositories are administered.
Sometimes you have to wait a long time for the abscess to break through. Then we recommend using the same ichthyol ointment, cakes made from baked onions, potatoes, and carrots. They help the fistula break through and pus drain. The patient chooses which flatbread is better, as they say, “at random” - whichever works more effectively, he “cooks” from it.
When all methods of conservative treatment have been exhausted, but the disease does not go away, we refer the patient for surgery, of course, if there are no contraindications. It is called Gabriel's operation, named after the surgeon who first performed it: a speculum is inserted into the anus, the mucous gland and fistula are excised. The treatment is very radical. True, scars appear after it, and even with hard stool, the lack of mucus causes certain inconvenience. Therefore, we try to injure this area as little as possible and, if possible, operate in extreme cases. It is better to use folk remedies and be observed at the clinic for a year. If the fistula heals, you can forget about the operation for decades.
However, frequent recurrences of the fistula are a big risk factor for oncology. Therefore, the patient must undergo an annual medical examination or examination by a surgeon. As a rule, such prevention is justified. During this period, one should not forget about maintenance therapy: make baths, lotions, pads, microenemas, follow a diet, especially for those who suffer from constipation and hemorrhoids. Here are some recommendations.
- As a laxative, drink 1 glass of freshly prepared carrot juice with pulp on an empty stomach. For hemorrhoids, steam and drink carrot tops as tea.
- Juice from ripe rowan berries - 0.5 cups of Zraz a day before meals. Apply the remaining pulp to the hemorrhoids in the form of a compress.
- Drink a mixture of carrot and spinach juices in a ratio of 10:3 3 times a day before meals. The daily dose is 2 glasses.
- Sauerkraut brine - 1 glass 3-5 times a day before meals for hemorrhoids, constipation and heavy bleeding.
- Grate raw potatoes with peel, squeeze out juice, 1 tbsp. Inject a spoonful of juice into the anus with a syringe at night. The course of treatment is 10 days.
- Consume 100-150 g of boiled red beets on an empty stomach for chronic constipation and digestive disorders. For spastic constipation, a salad made from boiled beets and vegetable oil is useful - also on an empty stomach.
- For prolonged constipation, beet broth is used for enemas: pour 20 g of beets with 2 glasses of water, boil for 30 minutes.
- Pour boiling water over washed prunes in the evening. In the morning, eat a few plums on an empty stomach and drink the resulting liquid (without sweetening it) as a laxative.
- Warmed water from pickled lingonberries, taken on an empty stomach, is also a good laxative.
Badger and bear fat are effective in treating the rectum. Turundas or tampons should be soaked in fat and inserted into the anus overnight. If the mucous membrane of the anal canal is erosive, you can make thin sticks from fresh potatoes rich in starch. It envelops well, relieves irritation, heals erosions and cracks in the anal rectum. The sticks are inserted overnight.
Now - about mucous glands and mucus. I am convinced that the removal of any organ, including mucous glands, is an intervention in nature: there is nothing superfluous in the body. However, if the glands are constantly inflamed, their excision is a necessary and necessary measure.
Sometimes patients complain of copious mucus secretion. However, in this way not only inflammatory processes of the mucous glands can manifest themselves, but also concomitant diseases. For example, the growth of mucous membrane in the intestine, like a villous tumor, which produces up to one liter of mucus per day, secreted through the rectum. And although the tumor is benign, the body, in fact, begins to rot. Villous tumors can occur in the rectum and in the overlying intestines. The literature describes a case where the colon was completely affected by it. Therefore, copious mucus discharge should definitely alert you. Often, patients are frightened mainly by the release of blood.
Excessive mucus, when it, as we say, comes out in “buckets”, and with blood, can also occur with ulcerative colitis, most often caused by stress and other reasons. Patients with ulcerative colitis should be observed by a gastroenterologist for at least 10 years: colorectal cancer may develop.
Concluding the conversation, I will say that the specialty of a proctologist is now, alas, gaining power and strength, since many of our diseases depend on the state of medicine and society, and a person’s attitude towards his health. Of course, we are far from Japan, where they thought of, for example, installing special sensors on toilets that detect the presence of blood or mucus in flushed feces. A dispatcher is sitting in some Japanese housing complex and sees on the instruments: in such and such an apartment one of its residents has intestinal problems. He comes and says: someone is sick. And doctors begin to check the whole family.
Many of us are embarrassed to see a doctor in a timely manner - they delay until they press properly. Why be ashamed? If there is slight itching or mucous discharge, you need to go to the clinic. As a last resort, at least tell your loved ones about the unpleasant sensations - this will make it easier to overcome false shame and begin treatment. Paraproctitis and its consequences - fistulas - are completely curable when time is not lost in doubt and torment.
Indications for fistula excision
A specialist who provides consultations in this area is a proctologist. You need to make an appointment if you notice the following symptoms:
- the appearance of pus and mucus from the anus;
- bleeding from the anus;
- unpleasant odor;
- wounds form near the anus that do not heal for a long time;
- digestion is impaired;
- problems during bowel movements;
- bowel problems: frequent diarrhea or constipation;
- pain when urinating;
- pain syndrome - it intensifies when the patient strains the abdominal cavity, including when sneezing or coughing;
- there is a feeling of discomfort, as if there is a foreign body in the posterior hole;
- increase in temperature and pressure;
- weakness of the whole body.
- a medical history of chronic or acute intestinal diseases, for example, enteritis, Crohn's disease, hemorrhoids, anal fissure, papillitis, proctitis, cryptitis, intestinal cancer and ulcerative colitis.
If the rectal fistula is not excised in time, the formation can become malignant.
What can a doctor do?
Therapy for patients with external fistulas is based on:
- local treatment;
- general therapeutic;
- operational.
Local therapy refers to the treatment of the resulting wound, as well as the protection of surrounding tissues from the effects of fluid that is released from the canal. For example, if the fistula is on the leg, abdomen, etc., then the purulent area is treated with various means (ointments, pastes and powders). They are applied at the external opening of the canal, thereby preventing the skin from coming into contact with pus, mucus, etc.
In addition, chemical agents can be used that prevent irritation of external tissues by neutralizing secretions from the fistula passage. For this, it is recommended to use inhibitors of proteolytic enzymes (for example, Gordox, Contrikal, etc.).
Mechanical methods of protecting the skin are aimed, first of all, at reducing or completely stopping discharge from the canal using special devices.
For the general treatment of purulent and other fistulas, they are constantly washed with an antiseptic solution.
Tubular granulating passages quite often close on their own after eliminating the causes of their occurrence (for example, removal of bone sequestration, ligature, etc.). But labiform fistulas never go away on their own. To treat such deviations, only surgical intervention is used to excise them, suturing the external holes, or resection of the affected organ.
It should also be noted that in some cases, surgeons create fistulas artificially specifically so that the patient can eat, or in order to remove accumulated secretions from any internal organ. These channels can be either permanent or temporary. After the patient's condition improves, the temporary canals are closed surgically.
In addition to external ones, internal fistulas (interorgan) are also created artificially. As a rule, they are imposed either for a long time or for life.
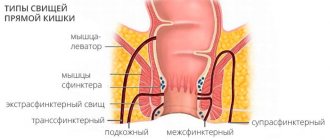
Technique
Depending on the type of paraproctitis, our proctologists at the Miracle Doctor clinic use various techniques. If the disease:
- intrasphincteric
- surgery is performed to remove the rectal fistula (Gabriel's operation); - transsphincteric
- the Gabriel technique is used or excision of the problem area with sphincteroplasty; - extrasphincteric
- removal of pathologically altered tissues using a ligature according to the Hippocratic technique.
Previously, the patient receives a consultation with an anesthesiologist, who, based on his health characteristics, selects the appropriate anesthesia. This is either general anesthesia or epidural anesthesia. Spinal or epidural anesthesia helps eliminate pain and relieve muscle spasm, so there is no need to administer additional drug to relax the sphincter tissue.
After anesthesia, the surgeon inserts an anal speculum into the rectum through the anus, and into the fistula tract a probe and a dye that tints the problem area.
The technique for removing an intestinal fistula depends on the location and size of the pathology. The surgeon’s task is to restore the sphincter and intestinal mucosa by completely removing the inflamed area.
What can you do
Of course, treatment of such a deviation requires mandatory consultation with an experienced doctor. Indeed, if treated untimely and incorrectly, a fistula can lead to serious complications that can endanger a person’s life.
But, despite this likelihood, adherents of alternative medicine still use numerous folk methods to close the resulting fistulas. Let's look at some of them in more detail.
Treatment of ligature fistula with aloe
To prepare the medicine, you need to take 10-12 fleshy arrows from the presented plant, and then wash them in warm boiled water. Next, the aloe needs to be finely chopped and placed in a liter jar. Pour 300 g of any honey into the container, cover loosely and place in a dark place for 7-10 days. In this case, after 4-5 days it is advisable to mix the mass well. Finally, the tincture must be strained several times and taken a dessert spoon three times a day.
Ointment for external fistulas
This ointment is good for healing and treating fistulas of the vagina and rectum. For this we need water pepper grass, oak bark, lard and flax flowers. All imposed plants must be chopped, and then placed in some container and immediately poured with melted lard. In this case, the ratio of fat and herbs should be one to two.
After these steps, you need to place the filled dish in the oven and turn on low heat. It is advisable to heat the ointment for at least 7-11 hours. Finally, the medicine must be cooled at room temperature. The method of treatment with this ointment is quite simple. To do this, you need to make a cotton swab, generously lubricate it with the product, and then apply it to the fistula opening. It is advisable to change dressings every five hours.
Decoctions for external fistulas
Infusions and decoctions of medicinal chamomile are used only externally - for washing holes. To prepare them, you need to take 1 large spoon of dried flowers, brew them with one glass of boiling water, and then leave for 60 minutes and filter.
Also, decoctions made from calendula are used to wash fistulas and create compresses.