- Indications for tooth extraction
- Contraindications for removal
Once upon a time, tooth extraction was considered one of the most common dental procedures. However, today doctors have radically changed their approach to treatment and are trying to avoid it even in the most hopeless situations. Despite the fact that modern technologies make it possible to implant a tooth immediately after extraction, natural teeth are still considered the best option. Therefore, such an operation is performed exclusively for medical reasons, which are divided into urgent and planned. Urgent indications include situations when pathological processes occur in the soft or hard tissues of the oral cavity that pose a potential threat to the patient’s health. Planned appointments are those that can be postponed indefinitely, that is, until the next visit to the dentist.
Reasons for performing tooth extraction surgery
Indications for an operation that involves removing the incisor from the alveolar socket are divided into two groups:
- emergency;
- planned in advance.
Emergency indications for performing tooth extraction are:
- acute inflammatory processes of a purulent nature (including those spreading to bone tissue);
- severe damage of no functional significance;
- severe acute pain in the absence of opportunities for conservative therapy;
- damage to the dental crown that cannot be repaired by placing a filling or dental prosthetics.
Indications for planned tooth extraction are:
- the formation of basal cysts and the development of periodontitis in the tissues surrounding the incisor with impassable root canals;
- periodontitis, accompanied by severe tooth mobility;
- the presence of supernumerary, impacted or incorrectly located teeth that injure the mucous epithelium of the oral cavity, promote the development of inflammation, provoke pain, impair diction or interfere with food intake;
- tumor growths in jaw tissues;
- the presence of teeth that prevent prosthetics or orthodontic treatment.
Removal of baby teeth
The reasons for removing baby teeth are their complete destruction, root fracture, or general inflammatory process. The decision about extraction is made by the doctor after examining the patient. The procedure is performed under local anesthesia or drug sedation.
Removal of baby teeth
The forceps are applied to the crown and are loosely fixed. Then the dentist uses a rotating motion to remove the tooth from the socket. The wound is clamped with a tampon. The development of bleeding and fever are unlikely.
Surgical technique
In modern dentistry, two tooth extraction techniques are used:
- simple;
- involving additional surgical procedures.
Simple removal is performed in cases where the coronal or root part of the damaged incisor is perfectly visualized and is well fixed in the forceps.
In such situations, the extraction procedure consists of the following steps:
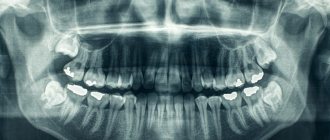
- collecting anamnesis (the doctor makes sure that the patient has no contraindications to the procedure, carefully examines x-rays);
- anesthesia;
- peeling the gums from the enamel using a special tool;
- fixing the forceps on that part of the incisor that is located above the bone of the alveolar process;
- rocking it, accompanied by destruction of the ligamentous apparatus holding it in the alveolus;
- extraction of the tooth and all mobile fragments of bone tissue from the alveolar socket;
- removal of cysts, granulomas, sanitation of purulent foci in the area of the removed incisor (if indicated);
- treating the hole with antiseptics and anti-inflammatory drugs;
- suturing.
Indications for surgical tooth extraction may include:
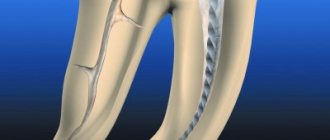
- curvature of tooth roots, preventing safe tooth extraction;
- complete destruction of the part of the incisor rising above the alveolar process;
- increased fragility of the dental crown;
- incomplete eruption;
- its presence in the gum in a horizontal position.
Performing operations of this type may be accompanied by incision of the gum tissue, removal of the bone hiding the unerupted incisor using an osteotome or drill, sawing the crown into several parts and taking other measures to facilitate the extraction of problem teeth.
Tooth root removal using forceps, elevators and drills
Forceps are usually used for simple tooth extraction. A separate instrument is used for molars, premolars, incisors and canines, upper and lower teeth. Also, all forceps are divided according to the location of the tooth - for the right and left sides of the mouth.
Types of elevators - straight, angular, bayonet-shaped
An elevator is a lever tool. Used for difficult molar removal. There are several types of them - straight, angular, bayonet-shaped. Their task is to facilitate the operation.
The technique is the same - anesthesia, applying an instrument, loosening the tooth, removing it from the socket.
The use of a bur is indicated for extracting the root, part of the molar remaining in the socket. And only if tongs and elevators are not enough. To do this, remove the outer part of the hole, and then remove the remaining root with forceps. The procedure is performed under local anesthesia, then stitches are applied.
In what cases should teeth not be removed?
Contraindications to the operation are:
- acute infectious diseases;
- menstruation in women;
- hypertensive crisis, severe arrhythmia and other cardiac disorders;
- I and III trimesters of pregnancy;
- taking medications that reduce blood clotting;
- hemophilia and other blood diseases;
- epileptic seizures;
- schizophrenia and other mental illnesses.
If the listed pathologies and conditions are identified, the issue of tooth extraction is considered on an individual basis.
Contraindications for removal
This operation has no absolute contraindications, however, there are situations when, if possible, it is recommended to postpone it for some time. These include acute infectious, inflammatory and cardiovascular diseases in the acute stage, pregnancy, central nervous system lesions, malignant tumors, and circulatory disorders. If it is impossible to delay removal, the doctor must evaluate the patient’s condition and select appropriate medications and surgical methods for him. All manipulations are best carried out in a hospital setting, so that if any serious complications occur, the patient can be provided immediate assistance.
Features of hygienic care after surgery
For patients undergoing surgery to remove one or more teeth, it is recommended:
- stop eating food for 2.5 hours;
- do not chew food on the side of the postoperative wound until it is completely healed;
- temporarily stop consuming too hot drinks and food;
- refrain from brushing for 1.5 days;
- give up active physical labor for 3 days.
If complications develop (the appearance of prolonged bleeding, inflammatory processes, purulent discharge, etc.), you must immediately contact specialists at a dental clinic and undergo a course of therapy according to the regimen they have developed.
Tooth extraction during pregnancy
Treatment and removal of teeth is permitted during pregnancy, but for acute indications. It is better to undergo examination and necessary procedures at the planning stage.
The tooth extraction technique is the same for all patients. The chair is installed at an angle of 15 degrees. Local anesthesia is indicated; general anesthesia is prohibited during this period. After the teeth are removed, the doctor will prescribe antibiotics. The patient should agree on the drug with the gynecologist.
And most importantly! If the inflammatory process has begun and the patient experiences pain, then treatment can and should be carried out in full. Up to tooth extraction according to indications.
Anesthesia
Our goal is to make any oral procedure as comfortable as possible for the child. To do this, we can use any of the methods of pain relief in dentistry accepted in the world today:
- topical anesthesia (applying the drug to the gum);
- local anesthesia (injection of anesthetic using a carpule needle);
- in some cases, xenon-oxygen anesthesia is used (precedes local anesthesia to reduce anxiety).
What to do if there is bleeding after tooth extraction
Normally, bleeding should stop within 15–20 minutes. If the tampon on the hole is saturated with blood, then it needs to be changed. If the bleeding does not stop or intensifies, consult a dental surgeon immediately. If you have any blood diseases or bleeding disorders, you should inform your doctor about this before surgery.
Tooth extraction is a full-fledged operation. Therefore, it is carried out according to indications. After the procedure, the patient must follow all doctor’s instructions. Only in this case the risk of complications is minimal and a quick recovery occurs.
Removal methods
The technique of tooth extraction is carried out in a simple or complex way, depending on the condition of the crown, roots, and anatomical location. If the crown is preserved, then a simple extraction method using forceps is most often sufficient for the procedure.
When the crown is severely damaged or the case is atypical (an incorrectly grown wisdom tooth), dentists resort to surgical removal using an elevator, gouging and sawing tools.
Dentistry does not stand still, and tooth extraction techniques are constantly being improved. Today this operation can be performed using ultrasound. This method has undoubted advantages over traditional ones:
- Ultrasonic exposure is aimed only at hard bone tissue, and therefore does not injure gums, nerves and blood vessels;
- there is no or minimal pain during the intervention;
- Using ultrasound surgery, you can remove a tooth if there are general contraindications, for example, pregnancy or hemophilia (poor blood clotting).
The main disadvantage of this technique is its high price compared to traditional methods.
Indications for removal of primary teeth in children
At the age of 5–6 years, temporary teeth begin to fall out, giving way to permanent teeth. But sometimes you have to resort to removing a temporary tooth in the dentist’s chair. Here are the main indications for the removal of temporary teeth:
- Advanced caries. If a tooth is so damaged that it cannot be restored, the doctor decides to remove it.
- Cyst at the base of a temporary tooth.
- The temporary tooth becomes loose but does not fall out, injuring the gum tissue and causing inflammation.
- The temporary tooth does not fall out for too long, preventing the normal growth of the permanent tooth.
- Serious tooth injury - chip or crack, root fracture.
- Phlegmon, periodontitis, sinusitis.
Planned indications.
There are a number of reasons why tooth extraction is inevitable, but the procedure can be postponed for a while and carried out when it is convenient for the patient.
Such indications include:
- chronic periodontitis outside the acute stage (if it is impossible to carry out therapeutic treatment of the tooth)
- tooth root cracks
- chipping of the tooth wall deep under the gum
- severe destruction of the crown part of the tooth by caries (if it is impossible to restore it with either a filling or an artificial crown)
- tooth root caries
- mobility of teeth III-IV degrees with periodontitis
- orthodontic indications (to correct bite)
- supernumerary, incorrectly positioned and impacted (not erupted) teeth
- teeth that injure surrounding soft tissues when it is impossible to move them (for example, wisdom teeth)
Emergency indications.
Urgent tooth extraction is required if it has caused the development of:
- acute purulent inflammation spreading to the bone (periostitis, osteomyelitis)
- cellulitis or abscess of surrounding soft tissues
- sinusitis (inflammation of the paranasal sinuses)
- lymphadenitis (inflammation of regional lymph nodes)
if the tooth is not subject to conservative treatment or does not represent functional value, and also
- for severe toothaches when adequate treatment is impossible
- with a longitudinal tooth fracture
- in case of a fracture of the coronal part with exposure of the pulp, if the crown cannot be restored by filling or orthopedic treatment.
Procedure for removing a permanent tooth
The procedure begins with examining the patient, studying his medical history, assessing the results of the X-ray examination and drawing up a treatment plan. The operation to remove a permanent tooth can be simple or complex.
A simple extraction lasts no more than 10-13 minutes and includes the following steps:
- treating the patient’s oral cavity with an antiseptic drug;
- use of local anesthetics;
- separation of gingival tissues from the dental neck using a special tool (raspator, smoother);
- fixing the forceps on the dental crown;
- dislocation of the problematic tooth using the method of rotation or rocking and carefully removing it from the alveolus;
- medicinal treatment of the formed hole;
- suturing;
- prescribing antibacterial, antihistamine, anti-inflammatory and analgesic drugs to the patient.
In case of complex removal, the surgeon has to take additional measures aimed at providing access to the problem area (cutting the gum, drilling out the bone tissue around the tooth root with a bur, etc.). In this case, the duration of the surgical intervention can increase to several hours.
Post-operative oral care
Improper care of the alveolar socket after removal of a permanent tooth is the most common cause of postoperative complications (severe bleeding, alveolitis, etc.). Therefore, after the procedure is completed, the doctor gives the patient a number of recommendations to prevent the development of pathological processes in the area of surgical intervention.
So, a patient who has undergone surgery is prohibited for 3-5 days from:
- include foods that are too hot, salty or spicy in your diet
- rinse your mouth intensively;
- apply warm lotions and compresses to the cheek on the side of the extracted tooth;
- take hot baths, visit a solarium or sauna;
- brush your teeth (only on the day of surgery);
- play sports, do work involving heavy lifting;
- open your mouth wide;
- actively grimace;
- chew food on the surgical side;
- touch the alveolar socket with your tongue, pick it with a toothpick or other objects;
- smoke;
- drink alcoholic and low-alcohol drinks.
In addition, the patient is instructed to attend all preventive examinations prescribed by the surgeon.
Contraindications for surgery
Reasons for refusing to perform an operation may include:
- decompensated diabetes;
- hypertensive crisis;
- exacerbation of certain mental illnesses;
- blood diseases (leukemia, hemophilia, etc.);
- severe arrhythmia and other heart rhythm disturbances;
- stroke or myocardial infarction suffered within 11-12 months preceding the operation;
- viral diseases of the respiratory system, occurring in an acute form;
- stomatitis, gingivitis and other infectious diseases of the oral cavity.
Almost all of the contraindications listed are relative. If they are detected, the question of the advisability of surgical intervention is resolved on an individual basis, taking into account the prevailing circumstances. If necessary, the operation is performed in a hospital setting (in the maxillofacial surgery departments of hospitals) under the supervision of experienced resuscitators and other specialists.
Healing process
If there are no complications, then after tooth extraction, complete healing of the gums occurs within 4 months in the following order:
- On the first day after surgery, a blood clot forms in the wound, which is necessary for the further healing process. The wound should not be disturbed with the tongue or rinsed.
- On the third day, a thin layer of epithelium forms. It is easily damaged, so you should brush your teeth carefully and avoid chewing hard food on the side of the extracted tooth.
- On days 4-8, the blood clot is actively replaced by connective tissue. By this time, there should be no open wound on the surface of the gum.
- On days 14-16 after extraction, the wound is completely overgrown with epithelium, the edges of the gums shift, instead of connective tissue, bone tissue begins to form in the socket.
- After 2-3 months, the process is completely completed, young bone tissue fills the entire hole.
- At 4 months, the bone tissue acquires the same structure as in the upper and lower jaw.
Complications arise if the wound becomes infected due to the doctor’s fault during surgery (ingress of pus, pieces of carious teeth) or due to the fault of the patient who did not follow the recommendations for care in the postoperative period. In these cases, gum healing is slower and accompanied by pain.
In advanced cases, the formation of abscesses and phlegmons with the threat of blood poisoning is possible. Therefore, if the pain in the wound does not subside after a few days, and the gums are inflamed, you should consult a doctor.