The hemostatic sponge is an important tool in the home and travel first aid kit and the best assistant to the surgeon. When used, it is possible to quickly stop bleeding. Today, hemostatic sponges come in a huge variety. They can be easily selected in size depending on the conditions of use.
Features of wound healing after tooth extraction
Before moving directly to hemostatic sponges, what they consist of and how to use them, you need to understand how the wound heals after removal and what can go wrong here. More on this later.
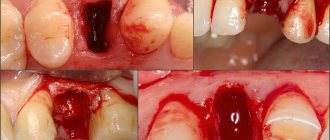
Why is there bleeding after removal?
Bleeding is a natural reaction to surgery. After all, when a tooth is removed, the smallest capillaries that penetrate the gums and ligamentous apparatus - the periodontium, which attaches the roots to the bone socket - are torn. And with difficult removal, the bleeding may be even stronger, because... The dentist makes incisions in the gums and drills into the jaw bone - the tissue is more damaged.
Bleeding is a natural reaction to surgery
Read on the topic: How long can a tooth hurt after extraction - normal and pathological.
How long does bleeding last normally?
Normally, the blood stops within 15-20 minutes (less often, within 45 minutes) and a blood clot forms in the socket. It seals the hole like a cork, preventing germs from penetrating inside. If the patient has problems that affect blood clotting, then the bleeding time is prolonged, and a clot may not form at all. And this is already fraught with inflammation of the bone socket (the pathology is called “alveolitis”). Therefore, according to indications, the dentist applies a hemostatic drug to the area of the extracted tooth.
On a note! Bleeding may appear again for a short time (and there will be quite a bit of blood) after the anesthetic wears off - if it contained adrenaline. This substance narrows the blood vessels in the intervention area, and as they expand normally, slight bleeding occurs. It goes away quickly.
Why does the bleeding not stop for a long time?
As a rule, after tooth extraction, the dentist says that you should not eat or drink for 2 hours. But few people say that you should not rinse your mouth or suck drinks out of a straw. In the first days, only oral baths are allowed, and it is better to drink in the usual way. Also, do not touch the wound with a brush. It is better to chew food on the healthy “side” of the jaw. Otherwise, there is a risk of moving or “pulling” the clot out of the hole - which will provoke new bleeding or even inflammation, which will result in long-term treatment.
The following groups of patients are also at risk:
- who has not formed a blood clot,
- with blood diseases,
- who takes blood clotting medications,
- having high blood pressure,
- women during menstruation or menopause,
- exposing themselves to physical activity immediately after removal and during the recovery process,
- if there was already inflammation at the extraction site (for example, pericoronitis above a wisdom tooth),
- during complex operations: when several teeth were removed at the same time, or manipulations were performed with increased tissue trauma.
Bleeding may occur during physical exertion after removal.
When you need urgent help
If the bleeding is profuse and does not stop for a long time, if after normalization of the condition the blood begins to ooze heavily again, this is a reason to consult a dentist. In a situation where the patient, in the presence of continuous bleeding, feels weakness, apathy, if the temperature has risen sharply (above 39 degrees Celsius), it is better to call an ambulance or go to the hospital on your own.
Any surgical intervention is inevitably associated with bleeding. At the same time, the main source of blood loss in operations on the liver, spleen and kidney when large vessels are intact is capillary-parenchymal bleeding, to stop which they resort to a variety of hemostatics: local hypothermia, thermo- and ultrasonic coagulation, laser irradiation, the use of hemostatic films, adhesives, gels , sponges, etc. [1].
The use of hemostatic materials alone in practical surgery is limited due to their low hemostatic activity and the occurrence of adhesions in the abdominal cavity. Toxicity, traumatic and antigenic properties, as well as the locally irritating effect of other drugs (for example, based on oxycellulose) contribute to the occurrence of an inflammatory process, necrosis of organ parenchyma, which predisposes to the development of infection [2]. However, according to many authors, sponges based on collagen, the most well-known and long-used traditional hemostatic agent, in combination with various substances, turn out to be the most effective compared, for example, with gauze packing (a physical method of hemostasis) and make it possible to stop bleeding in 1. 5-2, sometimes 3 times faster [3, 4]. In this regard, the development and study of new hemostatic sponges based on collagen, containing various substances that affect hemostasis, are urgent tasks with the goal of increasing the rate of onset of hemostasis, as well as expanding the scope of effective use of application procedures.
Achieving this goal involved consideration of known methods for assessing the effectiveness of the use of local hemostatic agents.
However, during the study of the problem, the presence of generalizing indicators was not revealed that would make it possible to give an integral assessment of the application of the corresponding method. For the most part, quantitative indicators are used here, expressed in the form of bleeding time, changes in sponge mass and similar characteristics. During the course of this work, no other indicators were found. In this regard, the task was set to develop a methodology that would allow assessing the effectiveness of using collagen sponges using quantitative, qualitative and integral indicators.
The purpose of the study was to study the effectiveness of new samples of hemostatic implants based on collagen and hemostatic agents deposited in them; development of a method for assessing the effectiveness of collagen hemostatic sponges in stopping parenchymal bleeding in surgical practice; study of new drugs based on collagen sponges in a comparative aspect.
As materials for experimental studies, samples of hemostatic collagen sponges with a length, width and height of material of 1 cm were used, weighed on a torsion balance, containing: hemoblock 2%; hemoblock 5% [5]; hemoblock and tranexamic acid; platelets and tranexamic acid [6, 7]; cryoprecipitate 10%; cryoprecipitate and tranexamic acid; chitosan and caprofen [8, 9]; tranexamic acid 9%. Hemostatic collagen sponges Belkozin and Zelenaya Dubrava were used as comparative samples.
In vivo experiments
were carried out on 110 white Wistar rats of both sexes weighing 180-200 g. For the study, animals without external signs of the disease were used, which underwent a quarantine regime in the vivarium of the Federal State Budgetary Educational Institution of Higher Education "Kursk State Medical University". All animals were kept under identical conditions on a standard diet.
Experiments on animals were carried out under aseptic conditions in the operating unit of the Department of Operative Surgery and Topographic Anatomy named after. HELL. Myasnikov Federal State Budgetary Educational Institution of Higher Education "Kursk State Medical University".
Operations and manipulations with animals were carried out using general anesthesia (xylazine hydrochloride, zoletil), and removal from experiments was carried out by overdose of anesthesia, in accordance with the Convention for the Protection of Vertebrate Animals Used for Experimental or Other Scientific Purposes (adopted by the Council of Europe in 1986, Strasbourg, France), and Council Directive 86/609/EEC of 24.11.86 on the harmonization of the laws, regulations and administrative orders of the Member States regarding the protection of animals used for experimental and other scientific purposes.
For a comparative assessment of the time to stop bleeding and the amount of blood loss in an acute experiment, rats underwent a median laparotomy under general anesthesia (Fig. 1,
Rice. 1. Simulation of a liver wound. 2
).
Rice. 2. Simulation of a spleen wound.
The liver and spleen were removed alternately into the surgical wound. After careful hemostasis of the edges of the laparotomy wound and its delimitation with polyethylene, a dry sterile napkin with a known mass was placed under the intended area of organ injury.
The liver wound was made on one of its lobes by cutting off the edge in such a way that the length of the wound was 1 cm (tangential to the circumference of the liver lobe), and the depth was 0.5 cm (in the place furthest from the edge) (Fig. 3).
Rice. 3. Application of hemostatic material to the area of the liver wound. The spleen wound at one of its poles was modeled similarly (length - 0.5 cm, depth - 0.3 cm) (see Fig. 1,
2
).
The resulting capillary-parenchymal bleeding was immediately stopped by applying hemostatic material to the wound area. After the experiment, the sponge was weighed (see Fig. 3, 4
).
Rice.
4. Application of hemostatic material to the area of the spleen wound. As a control, we used the above technology without the use of hemostatic materials, using a gauze pad, Belkozin collagen sponge, and Zelenaya Dubrava collagen sponge. Simultaneously with the application of the wound and the application of hemostatic material, time was started using a stopwatch to record the period of bleeding cessation. To determine the time of final bleeding cessation, the moment of cessation of bleeding from the drug or control wound was noted.
The amount of blood loss was measured using the method of E.M. Levite. To do this, the difference in the mass of the sterile material before the operation and after it was soaked in blood during the operation was determined and calculated by the expression:
m2–m1=m,
where m2 is the mass of the material after complete hemostasis (the blood flowing from the wound was absorbed into the material); m1 is the mass of the material before the experiment; m is the amount of blood loss.
The obtained data were statistically processed with the calculation of average values, standard errors of means and significance of differences. Differences for which the p
was less than or equal to 0.05. The significance of the differences was assessed using the Mann-Whitney test, as well as by calculating the confidence interval [10, 11].
In addition, a visualization coefficient was introduced, which made it possible to numerically express the ability of a particular sponge to absorb blood during the corresponding physical process. This coefficient (hereinafter K) was calculated as the difference between the rate of blood flow (ic) from the wound and the rate of its absorption by the sponge (pg). In this case, the rate of blood flow was determined as the volume of blood expended per unit of time, and the rate of blood absorption by the sponge was determined as the ratio of the difference in the weight of the sponge before and after the experiment to the time of bleeding.
TO
=
C
ik–
C
pgmg/s;
In order to track the dynamics of changes in the rate of blood flow per unit of time, we introduced an indicator of the deceleration of blood flow (hereinafter - H), which was calculated as the ratio of the K indicator to the bleeding time.
When studying in an acute experiment on rats in the comparative aspect of the time to stop bleeding on a model of experimental injuries of the liver and spleen using the studied samples, the results presented in table were obtained. 1,
Table 1. Average indicators of time to stop bleeding in a standard liver injury model, average K- and H-indicators (M±m), statistical analysis Note. Here and in the table. 2:* - p - significance of differences in mean values in relation to control groups (1, 2, 3, 4) was calculated using the Mann-Whitney test. Data were considered reliable at p≤0.05; ** - significant differences relative to control groups with a probability of 95% when comparing confidence intervals. CI—confidence interval, TC—tranexamic acid. 2
.
Table 2. Average indicators of time to stop bleeding in a standard splenic injury model, average K- and H-indicators (M±m), statistical analysis
Analysis of the results showed that the drugs have hemostatic properties, significantly reducing bleeding time relative to the control. After a comparative assessment, it was concluded that a highly effective drug is a hemostatic sponge with tranexamic acid 9% ( p
≤0.05), since this drug received high ratings for quality properties (Table 3)
Table 3. Assessment of the qualitative properties of the drug Note.
A - adhesion to the wound surface (adhesion); AbP—absorption capacity in experiments on the liver, mg; AbS - on the spleen, mg; U - ease of use; * - light drug; ** - crumbles, crumbles when cutting or using. Rating scale: 1 - absence of attribute; 2 - unsatisfactory; 3 — satisfactory; 4 - good; 5 - excellent. and has the lowest K-indices both in experiments on the liver (1.072±0.130832) and in experiments on the spleen (1.08±0.044835) with a bleeding time of 50.7±1.9 s and 68.4 ±2.9 s respectively. The least effective drug was a hemostatic sponge with chitosan and caprofer (K = 1.981 ± 0.054921, K = 2.424 ± 0.135248 for the liver and spleen, respectively), which also had a low rating for use, since it crumbled, crumbled when cut, stuck to gloves, was extremely light in weight, and poorly applied to the wound surface. At the same time, the H-index in experiments on the liver in both cases was approximately the same (≈0.02), while the K coefficient and the average bleeding time differed by almost 2 times.
The current situation indicates that, under conditions of the same rate of slowing down blood flow, a sponge with chitosan and caprofer absorbs 2 times more blood volume, since it requires 2 times more time to create hemostasis than a sponge with tranexamic acid 9% . This fact indicates the insufficient effectiveness of the active substance included in this sponge. The results obtained in experiments on the spleen confirm this fact (bleeding time 131.5±15, K=2.424±0.135248).
The next most effective drug is a hemostatic sponge with cryoprecipitate 10%, which, among other things, has one of the highest H-values (H = 0.025) in experiments on a standard spleen injury model (reliable data). This is followed by a hemostatic sponge with cryoprecipitate and tranexamic acid ( p
≤0.05; unreliable differences in splenic injury when compared with Belkozin). With minimal differences, next comes a hemostatic sponge with a hemoblock of 5%, which, like the sponge with cryoprecipitate 10%, has H = 0.025 in experiments on the spleen. It is inferior to a hemostatic sponge with a hemoblock and tranexamic acid (unreliable differences in liver injury in relation to Belkozin, Zelenaya Dubrava). Despite the fact that it has the highest H-value in experiments on the liver (H = 0.035), it also has a fairly high K coefficient, which indicates that it absorbs a large volume of blood while slowing down the rate of bleeding from the wound quite quickly (Fig. 5) .
Rice. 5. Average values of H- and K-indices in experiments on a model of standard liver injury. In experiments on the spleen, this material performs worse: it has one of the lowest H values against the background of a high K value (Fig. 6).
Rice. 6. Average values of H- and K-indices in experiments on a model of standard spleen injury. The hemostatic sponge with platelets and tranexamic acid performed somewhat worse (an unreliable difference in the data is determined only for Belkozin). In seventh place is a hemostatic sponge with a hemoblock of 2% ( p
>0.05 relative to Belkozin; non-significant differences are determined in case of spleen injury with Belkozin, Zelenaya Dubrava).
in vivo studies
in an acute experiment on rats, when studying in a comparative aspect the time to stop bleeding, the amount of blood loss on a model of experimental standard injuries of the liver and spleen, quantitative, qualitative and integral indicators allow us to conclude that all experimental samples have reliable hemostatic properties, expressed to varying degrees. The activity of the latter is associated with the hemostatic agents included in the sponges. Contrary to the expected results, monocomponent sponges turned out to be more effective: hemostatic sponges with tranexamic acid 9% and cryoprecipitate 10% performed better, followed by their combination. The same pattern was revealed with sponges containing hemoblock: a single drug (hemoblock 5%) turned out to be more effective than the combination of hemoblock and tranexamic acid. Apparently, these phenomena are associated with the mechanism of drug preparation, their interaction (destruction), and the nature of the substrate impregnation (layer-by-layer or continuous). The low hemostatic properties of the hemostatic sponge with chitosan and caprofer can be associated with the absorption properties of the polysaccharide included in the composition, which needs time for the fibers to swell.
These samples can be used during operations on parenchymal organs, which will significantly reduce postoperative complications associated with the presence of delayed bleeding. However, to make a final decision, it is necessary to carry out a wider range of studies in order to study such properties as biodegradation, bioinertness, the severity of the adhesive process at the implantation site, the presence of local and systemic effects after using materials. The methodology for assessing the quality of hemostatic sponges developed during the study can be used in similar studies, and the qualitative K-index can serve as a criterion for classifying sponges and act as a marker of the degree of sorption.
Based on the results of the study, we can conclude that all presented samples reliably have hemostatic properties, most of which are superior to analogues available on the market. A new technique has been developed that makes it possible to evaluate the properties of hemostatic sponges in an acute experiment using integral indicators.
The authors declare
no conflict of interest.
Information about authors
Bezhin A.I. (Bezhin AI)
— Doctor of Medical Sciences, Head of the Department of Operative Surgery and Topographic Anatomy named after. HELL. Myasnikov KSMU; Kursk, st. K. Marksa, 3, 305041; e-mail
Soldatova Daria Sergeevna (Soldatova DS)
- doctor - pediatric surgeon of the Regional Children's Hospital No. 2, candidate of the Department of Operative Surgery and Topographic Anatomy named after. HELL. Myasnikov KSMU; Kursk, st. Khutorskaya, 43 "a" 305029; e-mail;
https://orcid.org/0000-0002-9278-2737
Litvinenko I.V. (Litvinenko IV)
— 3rd year student of KSMU; Kursk, st. K. Marksa, 3, 305041; e-mail
Ryzhov A.S. (Ryzhov AS)
— 3rd year student of KSMU;
Kursk, st. K. Marksa, 3, 305041; e-mail
Istranova E.V. (Istranova EV)
— Ph.D., leading researcher at the Institute of Regenerative Medicine, Sechenov University; Moscow, st. Trubetskaya, 8, building 2, 119991;
Istranov L.P. (Istranov LP)
— Doctor of Pharmaceutical Sciences, Professor, Chief Researcher at the Institute of Regenerative Medicine, Sechenov University; Moscow, st. Trubetskaya, 8, building 2, 19991; e-mail: [email protected]
What is a hemostatic sponge
Now let's move on to why a hemostatic sponge is placed in the hole left after tooth extraction? Let's first understand the terminology. “Hemo” means “blood” and “stasis” means stopping. Those. a hemostatic sponge is needed to stop bleeding. In simple terms, this is a kind of replacement for a blood clot. The hemostatic sponge in the tooth socket not only seals the open cavity, but also has a hemostatic effect. Firstly, it puts pressure on small vessels, stopping bleeding. Secondly, it absorbs excess blood, increasing several times. The bleeding stops within 2-3 minutes.
On a note! By the way, local hemostatic agents are used not only in dentistry, but also in other areas of medicine - for example, hemostatic bandages successfully replace tourniquets that are applied for bleeding.
Recommendations
The collagen sponge should be removed from the packaging immediately before use. It is important to follow the rules of asepsis to prevent accidental infection in the wound. The hemostatic agent is carefully applied to the bleeding area and held for a couple of minutes. Deep wounds are tightly packed and then bandaged.
After the collagen sponge is saturated with blood, it will slightly increase in size. This will ensure that it adheres tightly to the damaged bleeding area. In cases where it is necessary to close damaged areas of parenchymal organs, a sponge of a suitable size is placed in the existing cavities. To stop bleeding, it is allowed to form several layers from it. After this, it is fixed using a U-shaped seam.
You can now buy a collagen hemostatic tube in pharmacies at an affordable price. It is presented by manufacturers in a wide range. You can also pick up the product in specialized online stores. Now you can use the booking service or order delivery of the product to the specified address.
Before using a collagen-based hemostatic sponge, you should carefully read the manufacturer's instructions. The product should be stored in a dry place where the temperature is maintained in the range of 10°C - 30°C. With high humidity, the sponge quickly becomes unusable. The shelf life of the product, subject to the required conditions, is 5 years.
Appearance and release form
The hemostatic sponge looks like a cube or plate, which looks like a small sponge or a piece of yellow or white foam rubber. Although in fact it consists mainly of natural collagen with various medicinal additives. The plate is quite soft and easy to cut, which allows the dentist to cut the desired size according to the shape of the hole.
The plate is quite soft and easy to cut
Manufacturers produce both small (1x1 centimeter) and large sponges (10x10 cm). The plates are tightly sealed in transparent bags, and the cubes are sealed in dark, opaque bottles. Hemostatic powders and gels are also produced. Absolutely all collagen hemostatics dissolve on their own in the wound over time.
Types of hemostatic sponges
According to the manufacturing method, hemostatic sponges for teeth are of the following types:
- from donor blood plasma - amben,
- from bones/tendons/blood of cattle - collagen and gelatin.
You need to understand that a hemostatic agent not only stops bleeding (due to aminocaproic acid, for example) and stimulates the formation of a blood clot, but also has an antiseptic effect. It can also accelerate regeneration and relieve inflammation. It all depends on the active components that make up the hemostatic sponge. The drug can be impregnated with the following substances:
- antiseptics: chlorhexidine, furatsilin, silver suspension, boric acid, iodoform,
- local anesthetics: for example, lidocaine,
- preparations for bone regeneration: calcium phosphate,
- antibiotics: metronidazole, chloramphenicol, neomycin, gentamicin, etc.,
- natural substances: propolis, eugenol, etc.
Hemostatic sponges for teeth come in different types
Manufacturers of hemostatic sponges
Popular manufacturers of hemostatic agents used by dentists in our country are domestic companies. Let's consider them further:
- Alvostaz compress from Omega-Dent: available in the form of cubes, flagella, powders and solutions. The compresses are numbered - “1” with iodoform, “2” with metronidazole and chlorhexidine, “3” with neomycin and chloramphenicol,
- "Gemasept" with gentamicin from the Russian Research Institute of Hematology and Transfusiology of the Federal Medical and Biological Agency",
- “Collagen hemostatic sponge” with silver and boric acid from “Zelenaya Dubrava”,
- “Hemostatic sponge” with furatsilin and boric acid from “Belkozin”.
Biological dressing Digestol
Biological dressing "Digestol" - Self-absorbing collagen wound coverings with a cleansing and antibacterial effect, are highly porous white or cream-colored plates with a specific odor, made from a mixture of natural collagen biopolymer and trypsin-like enzymes digestase and collagenase (from the hepatopancreas of the Kamchatka crab). Ingredients: collagen at least 80%, digestase enzyme (collagenase) at least 1%, purified water Area of application: Complex treatment of purulent wounds, trophic ulcers, treatment of infectious and inflammatory diseases of the oral cavity, complications of diabetic foot syndrome. It has a rapid hemostatic effect by stimulating platelet aggregation and an antimicrobial effect by destroying the walls of bacteria. For the complex treatment of purulent wounds, burns, trophic ulcers, bedsores, gunshot wounds, treatment of infectious and inflammatory diseases of the oral cavity, complications of the “diabetic foot” syndrome in surgery, tamponing of sockets in dentistry. Has a cleansing and antibacterial effect. It has a rapid hemostatic effect by stimulating platelet aggregation and an antimicrobial effect by destroying the walls of bacteria. Dimensions 100x100x5 No. 1, 50x50x5 No. 1, 10x10x5 No. 10. pH of the aqueous extract: 5.0-7.5 Sterile, single use Sterilization: radiation Guaranteed shelf life of the plates from the date of sterilization: 3 years. Manufacturer: ZAO “Zelenaya Dubrava” , Russia Price: on request
Indications for use
A hemostatic sponge can be useful after tooth extraction, especially wisdom teeth. Because the “eights” often do not erupt completely, and the dentist has to perform a mini-operation to get to them and remove them along with the roots. When a tooth is removed, a hemostatic agent is placed 3-4 months before implantation to completely eliminate the possibility of complications and problems with the formation of new bone in the socket.
Also, hemostatic sponges or powders are used during operations on the gums1 - plastic surgery, curettage of gum pockets (removal of deep “deposits” of tartar), and when cutting off dead areas of the jaw bone due to osteomyelitis. In the latter case, bone blocks and materials for regeneration of bone substance are additionally planted. In general, the doctor always assesses the patient’s condition in advance - asks about diseases and other conditions, and about the medications taken. If there is a risk of bleeding or poor regeneration, then rest assured, a hemostatic sponge will definitely be placed in the hole.
These sponges are used for bone augmentation
It is important to know! A few days after tooth extraction, it may be necessary to apply a hemostatic sponge if the dentist sees a tendency to worsen. For example, a clot has fallen out or the gums/bone have become inflamed.
How to use the drug correctly
How to use the sponge? The hemostatic sponge is placed into the socket of the extracted tooth only by the dentist. Home use is not recommended due to the risk of infection deep into the tissues. The application procedure is given step by step below:
- tooth extraction or treatment of the hole a few days after removal: in the latter case, purulent masses are removed, irrigation is carried out with an antiseptic,
- a piece of the hemostatic plate is cut off with sterile scissors or a hemostatic cube is taken with tweezers,
- the drug is placed in the hole and pressed with a flat instrument: if the hemostatic agent is pre-saturated with thrombin, the hemostatic effect is enhanced,
- if necessary, an additional piece of hemostatic is applied,
- if necessary, a small tampon is placed on top of the hole (it will be removed the next day),
- suturing the gums - a seam in the shape of the letter “P”: also, if necessary, in most cases you can do without stitches.
A piece of the hemostatic plate is cut with sterile scissors.
Analogs
Some patients believe that a hemostatic sponge is not able to stop bleeding and alleviate the patient’s plight. In reality, the effect of this medication is selective, and it is also important to consider the risk of side effects. In such clinical pictures, the attending physician introduces a replacement and suggests using an analogue of the specified pharmacological group. Here is a replacement worthy of modern pharmacology, which can also be purchased over the counter, but after consulting with your doctor first:
- Kaprofer;
- Alginatol;
- Natalsid;
- Eavisel;
- Polyhemostat;
- Tissucol Keith;
- Posterisan;
- Feracryl;
- Tachocomb;
- Styptic pencil;
- Tissucol.
Is it necessary to remove the hemostatic agent?
Patients often wonder what to do with a hemostatic sponge after it has been placed in the socket of an extracted tooth? How long should I keep it on, and will it dissolve on its own? The rules of conduct are as follows: carefully but thoroughly observe oral hygiene, and also take medications prescribed by the dentist. There is no need to specially remove the hemostatic agent - after all, it consists of components that will completely dissolve during wound healing. And instead of a hemostatic agent, its own tissues form in the hole.
“When my wisdom tooth was removed, they stuffed it into the wound like a piece of foam rubber. I then saw the houses through the seams. I was also surprised - what is it? And at the next appointment, my dentist told me that this is a special sponge that absorbs blood and protects against infection. And when it resolved, I didn’t even notice)) It probably completely disappeared in a couple of weeks.”
Ekaterina R., review from irecommend.com
Contraindications and side effects
The only contraindication to the use of a hemostatic sponge after tooth extraction is an individual allergy to any of the components of the drug. In particular, for antibiotics that are used to impregnate the hemostatic agent. Therefore, be sure to tell your dentist if you are allergic and to what medications. Hemostatic agents should also be used with extreme caution in children.
There are no side effects, because There are no toxic substances or components that affect perception in hemostatics. But if itching, inflammation, or swelling appears, feel free to contact your dentist. These manifestations can be caused either by a newly manifested allergy or by incipient complications - if, for example, the treatment was carried out poorly or the patient did not follow the doctor’s instructions.
1Skulean A. Periodontal regeneration, 2012.
Precautionary measures
Absorbable GG is not used for heavy bleeding resulting from damage to large vessels. A contraindication to the use of a sponge is the patient’s individual intolerance to certain components of the product (for example, Furacilin). When used independently, it is not allowed to place (remove) GG into the inner layers of the socket; only surface application is permissible. When the hemostatic effect is achieved, the sponge is carefully removed from the postoperative wound.