Tooth extraction is a dental operation that is performed strictly for medical reasons. Reasons for tooth extraction may include severe traumatic tissue damage, incorrect position in the jaw, the formation of a large cyst, or advanced pulpitis.
Tooth extraction can be simple or complex. Even when the procedure is performed by an experienced dentist, negative consequences cannot be ruled out. One of the possible complications of the operation is inflammation of the periosteum, or periostitis.
Classification of osteomyelitis of the jaw
The inflammatory process requires urgent and competent treatment; for this, the doctor prescribes medications and performs surgery to clear the tissue of necrosis.
Lack of therapy leads to severe complications, for example, the development of meningitis. According to the course, the pathology is acute, subacute and chronic. Depending on the cause of osteomyelitis, the following types are distinguished:
- traumatic;
- hematogenous;
- ray;
- odontogenic;
- after tooth extraction.
The traumatic type occurs as a result of injury, for example, after a broken jaw or injury. If bacteria enter the affected area, an inflammatory process begins. In the hematogenous form, pathogenic organisms enter the jaw tissue through the bloodstream from other foci of inflammation.
The radiation type is a complication of radiation therapy for oncological disorders and is quite rare. Most often, odontogenic osteomyelitis occurs, associated with complications of caries.
Under the influence of the inflammatory process, destruction of bone tissue inevitably occurs, that is, destruction. According to the degree of bone damage, the following types of pathology are divided:
- Destructive is characterized by the formation of sequesters, areas of dead tissue.
- Destructive-productive. Small sequesters and foci of osteosclerosis are formed, and the periosteum thickens.
- Hyperplastic. Occurs in children 7-12 years old, accompanied by necrosis, vascular thrombosis, and facial deformation.
In the chronic destructive form, the jaw bone becomes thinner, resulting in pathological fractures.
What to do if the periosteum of a tooth is inflamed?
The treatment tactics for flux depend on the stage of the disease, its location and other factors. In the early stages, when pus has not yet accumulated in the gums, inflammation can still be cured with antibacterial drugs, which are prescribed in combination with painkillers.
But with purulent inflammation, surgical intervention cannot be avoided. Under local anesthesia, the doctor opens the abscess, washes out its contents, and then treats the affected area with antiseptics. After this, a drainage is installed in the wound to ensure a constant drainage of pus, and the doctor prescribes treatment with antibiotics and antiviral drugs to the patient. After some time, the pain and swelling should disappear, and after a few days the incision will heal. True, sometimes periostitis can progress, gradually developing into an abscess - in such situations, treatment should be continued further.
Causes and provoking factors
In 80% of cases, odontogenic osteomyelitis occurs, and its main cause is advanced pathologies:
- carious damage to crowns;
- pulp inflammation;
- periodontitis;
- alveolitis;
- cyst and granuloma of the tooth;
- pericoronitis;
- boils and carbuncles;
- purulent diseases of ENT organs;
- diphtheria, scarlet fever, umbilical sepsis in newborns.
The infection enters the tooth root and then into the bone tissue, thus forming osteomyelitis.
The cause of traumatic osteomyelitis is often gunshot and stab wounds, as well as damage to the nasal mucosa. In such cases, bacteria enter the bones from the external environment and cause inflammation.
Doctors identify a number of factors that contribute to the development of inflammation:
- weakened immunity, poor lifestyle;
- blood pathologies;
- diabetes;
- rheumatic pathologies;
- polyarthritis;
- severe pathologies of the kidneys and liver.
Those patients who refuse timely visits to the dentist are more susceptible to osteomyelitis.
Symptoms of osteomyelitis
Acute pathology manifests itself sharply and is accompanied by the following symptoms:
- pain in the affected area;
- mobility of the diseased tooth, swelling of the gums;
- purulent discharge from the gums;
- numbness of the lip;
- putrid odor from the mouth;
- temperature rise to 38-39°C;
- enlarged lymph nodes;
- headaches, weakness, nausea;
- chills, lack of sleep.
The main symptom is severe pain that radiates to the ear, eye and temple. If the process has spread to soft tissues, the face swells and becomes asymmetrical, the skin feels hot to the touch, the patient cannot open his mouth and it hurts to swallow.
In the subacute form, the symptoms are less pronounced, so the patient’s well-being improves. There is no visible swelling of the face, pain becomes tolerable, but tooth mobility increases.
The chronic stage can occur due to improper treatment of acute osteomyelitis of the jaw; sometimes a primary chronic process also occurs. With this pathology, the symptoms are mild, but a hidden course can lead to tooth loss and pathological fractures of the jaw.
Diagnosis and treatment of inflammation
Acute osteomyelitis of the jaw is diagnosed by a dentist based on the clinical picture and the collected medical history. Additionally, laboratory tests and x-rays of the jaw are prescribed. In case of chronic pathology, the image will show signs of osteoporosis and sequestration.
Treatment begins with removal of the focus of necrosis, the affected tooth or abscess is removed, the wound is washed with antiseptics and antibiotics, and drainage is installed. If the teeth are hypermobile, therapeutic splinting is performed.
Additionally, anti-inflammatory drugs and antibiotics are prescribed. After stopping the acute process, physiotherapy is indicated to speed up tissue recovery.
In case of chronic pathology, an operation may be required, during which the doctor will remove the affected areas of bone tissue and fill the voids with osteoconductive material. If there is a risk of a pathological fracture, therapeutic splinting is used, which helps to avoid injury.
Treatment of osteomyelitis of the jawbone
The standard treatment program for acute osteomyelitis of the jaw includes:
- surgical intervention (removal of infected teeth, dissection of the periosteum, primary treatment of lesions in the bone, periosteum and adjacent soft tissues, opening, drainage and sanitation of foci of infection);
- surgical removal of sequestra (rejected jaw bone tissue);
- anti-inflammatory therapy;
- detoxification measures;
- taking general restoratives;
- symptomatic treatment.
In this case, the scope of surgical intervention, the nature of drug therapy and other treatment methods are determined by the characteristics of pathogenesis, the general condition of the patient and clinical symptoms.
Complications of the inflammatory process
Osteomyelitis of the jaw requires urgent treatment, otherwise there is a risk of developing a number of complications:
- abscess and phlegmon of jaw tissue;
- meningitis;
- meningoencephalitis;
- brain abscess;
- lung abscess and sepsis;
- pathological bone fractures;
- formation of a false joint;
- impaired mobility of the masticatory muscles;
- damage to the heart and kidneys.
Many of these pathologies lead to death or disability, and pronounced cosmetic defects.
What happens if you don't get treatment?
If you have inflammation of the periosteum of the tooth, and you do not want to carry out treatment and do not rush to see a doctor, then everything can be complicated by necrosis of the affected tissue and the spread of infection to neighboring organs: palate, throat, larynx, maxillary sinuses, ears, eyes, brain. Blood poisoning and sepsis may also occur, and large fistulas will appear. Some patients with complications cannot avoid osteomyelitis or phlegmon. And in most cases, you also have to say goodbye to the affected tooth, which could become the culprit for the spread of infection.
Such consequences require urgent surgical intervention, and without timely surgery, everything can end in death. Therefore, remember that the disease is not to be trifled with.
Prevention and prognosis
The prognosis for osteomyelitis is favorable if the patient consults a doctor in a timely manner and undergoes adequate therapy. The occurrence of pathology can be prevented by observing the following preventive measures:
- treatment of caries, pulpitis or gum inflammation should occur in a timely manner;
- Instant sanitation of inflammatory and infectious foci in the body should be carried out;
- you should strengthen your immune system, eat right and lead a healthy lifestyle;
- It is recommended to avoid any injuries to the jaw.
Dentists recommend brushing your teeth daily, morning and evening, for at least 2 minutes, and visiting the dentist annually for a preventive examination and professional oral hygiene.
Possible complications after tooth extraction
23.09.2012 18:12- Simple tooth extraction “all inclusive” - 2500 rub.
- Removal of a tooth with periodontal disease - 1500 rub
- Removal of a permanent tooth (complicated) - resorcinol formalin / bur separation machine / wisdom tooth - 4000 rub
- Removal of impacted (dystopic) wisdom tooth - 5500 rub
- Removal of an impacted (dystopic) wisdom tooth using an ultrasonic device - 7500 rub
Tooth extraction is a full-fledged operation, after which certain unpleasant consequences may arise, caused both by the behavior of the patient himself and by factors beyond his control. Complications can also arise during the operation, since the removal of some teeth can be very difficult: due to the large size of the root or strong bone tissue, it is necessary to make incisions, which, after a successful operation, are stitched. In any case, there is no need to worry, since unprotected tissues in the postoperative period are under maximum influence of microbes, which can result in inflammation.
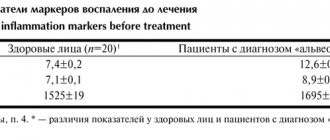
Alveolitis
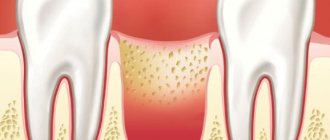
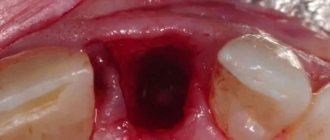
Very often, after tooth extraction, a complication such as alveolitis occurs. This problem occurs when a blood clot necessary for healing has not formed at the site of the extracted tooth. In this case, the hole becomes defenseless against external influences, as a result of which an inflammatory process often develops in it .
The key symptom of this complication is pain after tooth extraction (of varying degrees of severity). Pain may occur after 2-3 days. At the same time, the mucous membrane of the gum swells, the edges of the socket become inflamed, there is no blood clot in the tooth socket and the socket is possibly filled with food debris. The patient may have a fever, and sometimes there is pain when swallowing. The hole itself becomes covered with a dirty gray coating that emits an unpleasant odor. Along with these symptoms, the patient often feels general malaise, enlarged lymph nodes, slight swelling, fever, and pain in the area of the extracted tooth.
The main causes of alveolitis
Alveolitis is a disease that is not associated with the introduction of infection into the tooth socket as a result of working with an unsterile instrument. The disease develops with the participation of those microbes that are normally found in the oral cavity of every person.
So, teeth are usually removed due to the fact that chronic foci of inflammation are localized in the area of their roots that cannot be eliminated by conservative methods.
Therefore, the socket of the extracted tooth is primarily infected, and the concentration of microorganisms in it is quite high. If a person is healthy and all immune systems function normally, then the microflora is suppressed and the hole heals without complications. In the event that there are any local or general malfunctions in the mechanisms of the body's reactivity, the likelihood of developing inflammatory complications in the socket increases significantly.
Thus, the following local and general causes may contribute to the development of alveolitis:
- long-term existence of chronic inflammatory foci with frequent exacerbations, as well as exacerbation of the chronic inflammatory process;
- traumatic removal, when conditions arise for the destruction of the created barrier and the penetration of microflora deep into the tissues;
- absence of a blood clot in the socket of the extracted tooth (the clot did not form, or the patient did not follow the doctor’s instructions and the clot was removed; this usually happens when the patient is inattentive to the doctor’s recommendations and diligently rinses the tooth socket);
- general changes in the body due to stress, recent colds (infectious or viral) diseases, the presence of chronic diseases (mainly endocrine), especially in the stage of decompensation, general physical exhaustion, etc.
Treatment of this complication after tooth extraction
Treatment consists of relieving inflammation with local and general means. Sometimes it is sufficient to simply thoroughly rinse the hole with antiseptic solutions and then treat it with a special aseptic ointment or paste. Then, with the help of antibiotics and vitamins, general anti-inflammatory therapy is carried out. But sometimes treatment is delayed up to 1.5 - 2 weeks. In some cases, for this complication, physiotherapy or laser therapy may be prescribed.
Socket bleeding
One of the most common complications after tooth extraction is alveolar bleeding, which can occur immediately after surgery, within the next hour, day, and sometimes more than a day after tooth extraction.
Main causes of bleeding
- Early alveolar bleeding can be caused by the use of adrenaline: when it stops its action, a short dilation of the blood vessels occurs, which causes bleeding.
- Late socket bleeding may occur due to violation of the doctor’s recommendations in the postoperative period - mainly as a result of external disturbance of the socket of the extracted tooth.
- Local causes of socket bleeding include various physical injuries in the area of the socket of an extracted tooth: damage to the gums, fracture of part of the alveolus or interradicular septum, development of inflammation in the area of the extracted tooth, damage to blood vessels in the palate and under the tongue.
- The general causes of the appearance of alveolar bleeding are most often associated with various concomitant diseases of the patient (leukemia, scarlet fever, jaundice, sepsis, hypertension, etc.).
Treatment of this complication after tooth extraction
The effectiveness of stopping alveolar bleeding depends on how correctly the causes and source of bleeding were identified.
- If blood comes from the soft tissue of the gums, then sutures are placed on the edges of the wound.
- If blood comes from a vessel in the wall of the tooth socket, then first apply local cold in the form of an ice pack, then tightly squeeze the bleeding vessel and place a tampon soaked in a special hemostatic agent into the socket, which is removed no earlier than 5 days.
- If local measures do not help, dentists turn to general hemostatic agents that increase blood clotting.
Paresthesia
Much less often, after tooth extraction, a complication such as paresthesia may occur, which is caused by nerve damage during the process of tooth extraction. The main symptom of paresthesia is numbness in the tongue, chin, cheeks and lips. Paresthesia, as a rule, is a temporary phenomenon, disappearing within 1-2 days to several weeks.
Treatment of paresthesia is carried out through therapy with vitamins B and C, as well as injections of dibazole and galantamine.
Changing the position of adjacent teeth after tooth extraction
After tooth extraction, defects can often form in the jaw, and neighboring teeth begin to tilt towards the formed defect, and the antagonist tooth from the opposite jaw begins to move towards the defect, which leads to disruption of the chewing process. At the same time, the chewing load sharply increases, the usual state of the jaws is disrupted and bite deformation develops, which can greatly affect the general condition of the teeth. In this case, it is recommended to replace the extracted tooth with an artificial one using bridges, implants, or removable partial dentures.
All kinds of injuries that occurred during tooth extraction
Often, when removing the second premolar and molars of the upper jaw, perforation of the bottom of the maxillary sinus , resulting in communication between the oral cavity and the nasal cavity through the sinus.
The reasons are as follows:
(subject to the correct and careful actions of the doctor)
- anatomical features: the roots of the above teeth are close to the bottom of the sinus, and in some cases the bony septum is completely absent;
- the presence of a chronic inflammatory focus at the apex of the tooth, which destroys the already thinned bone plate.
If, after the removal of premolars or molars of the upper jaw, a message still appears, the doctor must use one of the known methods to eliminate it during the same visit.
There is only one contraindication:
The presence of a purulent inflammatory process in the sinus (acute purulent maxillary sinusitis). If the message is not diagnosed and eliminated in time, the patient feels liquid and liquid food entering the nose. In this case, you should consult a doctor as soon as possible. If you delay visiting a doctor, a chronic inflammatory process will inevitably develop in the sinus, which will require more serious and technically complex treatment.
Potential complications during the tooth extraction procedure include:
- Damage to adjacent teeth. Adjacent teeth or dentures (eg, crowns, bridges, implants) next to the extracted tooth can sometimes be damaged during the procedure. Adjacent teeth may become broken, split into pieces, or weakened during the extraction of the tooth or teeth, sometimes requiring more time from the dentist.
- Tooth fracture . The tooth may break during the extraction process, making the procedure more difficult and requiring more time and effort to complete the extraction. You may have to remove the tooth in parts. By the way, the process of removing a tooth in parts can cause complications after tooth extraction.
- Incomplete tooth extraction. A small portion of the tooth root may be left in the jawbone. Although this may increase the risk of infection, sometimes the dentist will choose not to try to extract it because removal may be too dangerous, for example if it is very close to a nerve.
- Jaw fracture. Patients with weak jaw bone structure (such as older women with osteoporosis) may be at risk for a jaw fracture. Even if the actual tooth extraction procedure is completed smoothly without any problems, there are cases of complications during the recovery period. Most often, a fracture of the jaw (in the lower jaw) occurs during the removal of “wisdom teeth” and in the upper jaw – a separation of the tubercle of the upper jaw.
- Removal of part of the alveolar ridge - occurs when a tooth is removed incorrectly, when forceps are placed directly on the bone surrounding the tooth and the tooth is removed along with it. In this case, an extensive bone and cosmetic defect occurs (especially in the anterior-frontal area). This problem can only be solved with the help of plastic surgery using artificial bone tissue and special protective membranes.
- Removal of a baby tooth and the germ of a permanent tooth - Occurs due to the carelessness or lack of professionalism of the doctor. When a baby tooth is removed (very often the roots of the tooth are missing, since they dissolve before changing teeth), the doctor begins to look for them in the tooth socket and perceives the germ of a permanent tooth as the roots of a baby tooth.
Remember the main thing: you should trust your doctor and actively participate in the treatment yourself, i.e. unquestioningly and carefully follow all recommendations. And if you suspect the development of complications, do not delay and do not hesitate to consult a doctor again.
Sources
- Lukyanenko V.I. Osteomyelitis of the jaws.
- Modern features of clinical manifestations of odontogenic and traumatic osteomyelitis of the lower jaw. Fomichev E.V.
Attention!
This article is posted for informational purposes only and under no circumstances constitutes scientific material or medical advice and should not serve as a substitute for an in-person consultation with a professional physician.
For diagnostics, diagnosis and treatment, contact qualified doctors! Number of reads: 2373 Date of publication: 04/29/2019
Dentists - search service and appointment with dentists in Moscow