Tooth extraction is carried out plannedly, as well as for emergency indications.
The main indications for planned tooth extraction: complete or severe destruction of the tooth crown and the inability to use it for prosthetics, chronic periodontitis that is not amenable to conservative treatment, grade III tooth mobility in periodontal diseases, and others.
Urgent tooth extraction is indicated for purulent periodontitis, acute osteomyelitis, periostitis, sinusitis, lymphadenitis (if the source is a diseased tooth), fracture of the tooth crown exposing the pulp and some other diseases and conditions.
Removing various teeth has some of its own characteristics, for example, removing teeth with a crown is somewhat simpler than removing tooth roots. The extraction technique for the teeth of the upper and lower jaws, incisors and molars is also slightly different.
Indications and contraindications for molar tooth extraction
Reasons for removing a molar tooth may be:
- purulent periostitis;
- abscess;
- phlegmon;
- large tumor in the tooth area;
- purulent periodontal disease;
- the presence of a cyst in the area of the diseased tooth;
- exposed pulp;
- longitudinal tooth fracture;
- critical tooth decay;
- critical tooth curvature;
- disease of the dental bone tissue;
- sinusitis.
The following reasons are contraindications to the removal of molars:
- acute heart diseases;
- acute viral diseases;
- flu;
- angina;
- renal failure;
- pancreatitis;
- hepatitis;
- acute diseases of the nervous system;
- oncological diseases
- initial and final stages of pregnancy;
- stomatitis;
- gingivitis
- general degeneration of the body;
- alcohol poisoning.
FAQ
• Is it painful to remove a tooth?
Painless tooth extraction using local anesthetics is carried out by absolutely all dental clinics. But if “freezing” is not enough, then it is better to go to a private clinic that provides all types of pain relief.
• How do you know when a tooth needs to be removed?
If it is very loose or the crown is completely destroyed, then most likely it will be removed. In other cases, accurate diagnosis is necessary.
• Is it possible to have a tooth removed if you have a cold?
Surgical intervention is unacceptable in the presence of an acute infection, including acute respiratory infections or influenza. This is due to the high probability of infection of injured tissues.
• Is it possible to remove a tooth if you have sinusitis?
The operation is not performed during exacerbation of the disease.
Molar removal technology
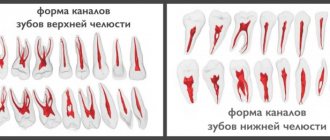
Before proceeding with the removal of a molar, the doctor must make sure that there is no curvature of the roots. For this, an x-ray is taken. If the roots are not bent, the patient is given an anesthetic injection. After 10 minutes, the tooth can be removed.
First, the dentist carefully separates the gum from the body of the tooth. Then he grabs the tooth with pliers and begins to swing it and rotate it at the same time. After several such manipulations, the doctor pulls the tooth out of the alveoli.
In this sequence, both the upper and lower root teeth are removed. However, it is somewhat more difficult to grasp the upper molars with forceps.
Sometimes, when removing a molar, the doctor must first cut it into two or three parts and then pull out each part separately. This usually happens when the roots are bent.
In case of severe curvature of the roots, when they intertwine with the roots of neighboring teeth, removal must be done in fragments and under general anesthesia. In this case, the doctor completely exposes the gum around the diseased tooth.
If there is a cyst in the area of a diseased molar, the doctor is required to be highly qualified. This removal is done under both local and general anesthesia.
Two days after the removal of a molar, the patient must visit the dentist again to take an x-ray. This is necessary to ensure that all tooth roots have been removed.
Possible complications after tooth extraction
Complications can appear during surgery, as well as after it, and can be local or general. General: fainting, rarely – shock. Their cause is the patient’s psycho-emotional stress, sometimes pain due to poor-quality anesthesia.
Local complications:
- Fracture of the tooth being removed (crown or root);
- Dislocation or fracture of a nearby tooth;
- Trauma to the soft tissues of the oral cavity;
- Dislocation or fracture of the jaw;
- Perforation of the bottom of the paranasal sinus;
- Pushing the tooth root into the maxillary sinus;
- Bleeding;
- Alveolitis.
Is it painful to remove molars?
Today, only older people remember the terrible pain during the removal of molars. Nowadays, the quality of painkillers is so high that the patient does not feel pain at all, even with difficult removal. At the same time, after the anesthesia wears off, pain, of course, occurs, but it is quite tolerable and depends on how much the gum under the tooth was disturbed.
If the pain is still severe, then the dentist recommends taking a painkiller tablet. The same analgin successfully dulls pain for a long time.
In rare cases, the patient may experience throbbing and increasing pain. This annoying phenomenon occurs due to inflammation of the socket. If measures are not taken quickly, the tissue begins to fester in the hole. This process can be suppressed with drug treatment, but sometimes you have to open the gum and clean the hole from pus.
Removal steps
Preparation
The dentist-surgeon examines the patient’s oral cavity and prescribes x-rays, if necessary. X-ray examination reveals the structural features, condition and exact location of the roots, and shows the presence of hidden inflammatory processes. The doctor selects the painkiller and dosage, finds out if the patient has any contraindications or allergies.
Important! If you have any fears, doubts or questions, it is best to discuss them with your doctor before the procedure.
Operation
During one operation, the tooth must be fragmented along the roots, and then removed as carefully and minimally invasively as possible, without destroying the bone tissue surrounding the six. In case of complex tooth extraction (if the six is hidden by the gum), the gum is cut, the tooth is destroyed using special tools and removed in parts.
Removal of molars during pregnancy
Let us say right away that any surgical intervention during pregnancy is extremely undesirable. If a molar tooth hurts at this time, then ideally it would be best to simply heal it. Unfortunately, sometimes this is no longer possible and the diseased tooth has to be removed.
It is highly undesirable to remove molars in the first and last months of pregnancy. It is at this time that the fetus is most vulnerable.
If it is possible to postpone the removal of a molar until the birth of the child, then this is exactly what should be done.
Under no circumstances should you hide your pregnancy from your dentist. On the contrary, this should be said immediately. In this case, the doctor will select a harmless anesthetic that will not cross the placental barrier.
If a pregnant woman is facing a complex molar tooth extraction, then this should only be done in a hospital setting. After removal, the patient should be under medical supervision for at least two to three days. This is due to the fact that very often, after the removal of a molar, pregnant women experience a sharp increase in body temperature, and this is extremely harmful for the fetus.
What is the difference between implantation on the upper and lower jaw?
Features of the operation from below
Implantation of the 6th tooth from below is performed using a two-stage method with delayed loading. The implant is implanted using the patchwork method. The crown is installed on the abutment after the artificial root has healed (after 2-4 months). Features of implantation are associated with the anatomical structure of the mandibular structures:
- high jaw bone density - the implant takes root faster, its good primary stability is achieved;
- bone tissue is stronger, therefore it decreases more slowly than in the upper jaw;
- the volume of the mandibular bone is anatomically higher - there are more opportunities to replace the lower tooth without tissue expansion;
- absence of sinuses - there is no risk of injuring the membrane of the maxillary sinus during implantation.
But the trigeminal nerve passes through the base of the lower jaw; if the bone atrophies, it can be damaged (if the technology of the implantation protocol is violated).
Installation of the implant from above
Implantation of the first molars of the upper jaw also has features associated with the anatomy of the jaw structures. The upper teeth are located close to the sinuses (maxillary sinuses), damage to which is accompanied by serious consequences. The maxillary bone is looser and thinner, so it decreases very quickly, and implants take 1-2 months longer to take root than in the lower jaw.
- The choice of method for implanting first molars is a two-stage protocol with a break for osseointegration of the titanium root. The average healing time for upper jaw implants is 4.5 months.
- Since the classical protocol requires sufficient volume and good quality of bone tissue, treatment is often complemented by osteoplastic surgery (sinus lift).
- When making prosthetics, the increased mesiodistal space and the distribution of occlusal forces are taken into account.
Molar tooth extraction in children
Unfortunately, young children often develop diseases in both their primary and permanent molars. Worse, it is not always possible to heal them. Dentists remove permanent teeth for children only when there is no way to save them.
Primary molars are both treated and removed. If a permanent tooth begins to grow under a baby molar, then the baby tooth is always removed, since it interferes with the normal formation of the permanent tooth.
At the same time, dentists never agree to premature removal of baby molars. Such teeth are sure to heal. If you remove a baby tooth ahead of schedule, then the baby will develop a crooked bite.
There are situations when a child’s molar tooth must be removed. Such situations include:
- molar root cyst;
- presence of granuloma;
- inflammation of the tooth root;
- inflammation of the nerve of the lower jaw;
- severe destruction of the integrity of the tooth.
Care instructions
Before the socket is tightened, you should not overheat the body, drink or eat hot or cold drinks, food, or chew on the operated side. You should not smoke, as nicotine constricts blood vessels and impairs wound healing. It is forbidden to lick a blood clot from the socket.
Antibiotics are prescribed for tooth extraction if the procedure was complicated. They are necessary to prevent tissue infection and the development of inflammatory processes. For the same reason, it is recommended to rinse your mouth with antiseptics. In this case, there is no need to rinse intensively, since it is possible to wash out the blood clot from the socket. Analgesics can be used to relieve pain.
Is it possible to remove a molar tooth yourself?
Trying to remove a molar tooth yourself is extremely dangerous. The only exception is very severe tooth looseness. It should be borne in mind that complete removal even in this situation will not work. You will simply break off the body of the tooth from the root, and nothing more. In any case, after such an independent removal, you need to visit a dentist, who will determine what should be done next. Sometimes an artificial tooth is installed at the root, and it can last for more than one year. If the root has defects, then it has to be removed.
There are situations when you have to remove a child’s very loose baby tooth at home. In this case, you should thoroughly brush the baby’s teeth and disinfect the oral cavity. Then you should wrap your fingers in sterile gauze, loosen the tooth thoroughly, and only then try to pull it out. If this was not possible on the second attempt, then the child must be taken to the dental clinic in any case.
If you have successfully removed the tooth from the socket, then you must firmly place a gauze swab in the socket and leave it there for 30 - 40 minutes. In the next two hours, the child should not be allowed to eat or drink.
Even if the removal was successful, the baby still needs to be shown to the dentist. This is the only way to protect your child from possible complications.
When is surgery indicated?
Indications can be called urgent and planned. The difference between them is that with an urgent operation, the clinical picture in the oral cavity and the general condition of the patient does not require delay. Delay may result in complications not only in the maxillofacial area, but the patient’s general condition may worsen.
Urgent indications include:
- A situation where dental tissues are severely destroyed and do not provide any functional benefit, but only aggravate purulent inflammatory processes in the oral cavity and soft tissues of the face. Usually these processes come from this jaw structure, due to the constant accumulation of pathogenic microflora there. Untimely treatment can cause the following purulent-inflammatory processes: periodontitis, periostitis, sinusitis, phlegmon or abscess.
- Diagnosed osteomyelitis in the projection of a destroyed, diseased dental unit.
- Longitudinal dental fracture.
- Transverse fracture of the dental crown with opening of the pulp chamber, but due to curvature or resorption of the roots, the tooth cannot be treated endodontically.
Why do you need to remove a cyst?
Patients sometimes do not want to resort to surgery, claiming that the tumor does not cause discomfort. Yes, the development of a cyst is asymptomatic. But it begins to destroy the root of the adjacent tooth, and then the surrounding tissue. And instead of timely basic surgery, you have to perform complex manipulations that threaten complications.
Another point:
If you do not remove the dental cyst while it is still forming (the cost will be determined by the attending physician), then there is a possibility of its degeneration into a malignant tumor.
Come for a consultation, and we will decide what steps you need to take specifically in your situation, whether you can save the tooth or need to remove it, we will take pictures to identify a cyst or granuloma. Fast, comfortable, pain-free.
With complete absence of a tooth
Prosthetics for front teeth in the absence of them involves 2 main methods:
- Installation of a bridge prosthesis
- this method is suitable for replacing 1 to 4 missing incisors. A bridge is a structure of several connected crowns, 1-2 suspended in the center and 2 hollow on the sides, which are attached to adjacent supporting teeth. The main disadvantage of the method is the need to grind and often depulpate the supporting units, even if they are completely healthy. That is, if you need to restore 1 missing incisor, two adjacent ones will have to be injured. - Implant prosthetics
– technology allows you to restore any number of missing teeth in a row. An implant is implanted into the jawbone, which fully replaces the missing tooth root. After the implant has healed, an adapter (abutment) is installed on it, onto which an artificial crown is fixed, identical in shape and color to the natural tooth. If an entire segment of the dentition is missing (3 or more teeth), 2 artificial roots are implanted, onto which a bridge is fixed. - Prosthetics of the front tooth immediately after extraction
is performed using the express implantation method. Immediately after surgical removal of a tooth, an implant is screwed into its socket, an abutment and a temporary crown made of lightweight plastic are fixed onto it. The temporary crown is removed from the bite, does not take part in chewing, it is necessary only to preserve the aesthetics of the smile. After 2-3 months, when the implant has fused with the bone, the temporary prosthesis will be replaced with a permanent one made of durable, reliable material (metal-ceramics, zirconium, etc.).
Prosthetics on implants does not involve injury to neighboring units; implanted implants perform all the functions of a natural tooth root and prevent jawbone atrophy. Implants are implanted once and for all; only prosthetic structures are subject to replacement (if they break or end their service life).
Recovery period
How long does recovery take after removal of upper wisdom teeth and what limitations does it impose? In most cases, after 1-2 days the patient returns to normal life, but sometimes recovery takes longer. To prevent the rehabilitation period from being prolonged, it is very important to follow the doctor’s recommendations:
- take prescribed antibiotics, painkillers and anti-inflammatory drugs;
- do not visit the bathhouse, sauna, swimming pool, or take a bath;
- follow a diet, if possible, eat only soft foods;
- refrain from smoking.
If the doctor did not make mistakes during removal, and the patient carefully followed all the doctor’s recommendations, then the recovery period will pass quickly, and the problem of the upper “eights” can be forgotten forever.
What to do if the bleeding does not stop
Immediately after removing a molar, the surgeon places a tampon on the socket to stop capillary bleeding. The patient needs to clench his jaw and not remove the tampon for 20 minutes. During this time, the blood coagulates and a clot forms in the hole, protecting the fresh wound from the penetration of bacteria into it.
If the patient has high blood pressure or poor blood clotting, the tampon should be kept in place for 40-60 minutes.
When a person strictly adheres to medical recommendations, but the bleeding does not stop, he should contact a dentist for help.
List of additional tools
In the process of work in surgery, not only modern equipment is used, but also hand instruments:
Inflammation after wisdom tooth removal
- Bit. The design is used in rare cases, due to its large size and awkward shape. The instrument is used as an additional lever, which is placed between the alveolar part of the tooth and its roots. In some cases, a chisel can simplify the procedure of tooth extraction.
- Hammer. It is used only for surgical indications, when, for example, it is necessary to hollow out the root part of the elements. The instrument is one of the most traumatic, so it is used only in rare cases.
- Drill. Used only in the extraction process of multi-root units.
- Luxator. The design has a thin shape, allowing the doctor to freely penetrate the periodontal area. In modern clinics, surgeons are increasingly replacing standard forceps with luxators, as they provide minimal risk of injury to the jaw bones.
- James Elevator. Used for complex operations, for example, when removing wisdom teeth from the oral cavity. There are several types of tools: right- and left-handed, straight, curved.
- Cryen's Elevator. It, like the previous surgical instrument, is designed to perform complex operations, but differs in shape. The Cryen elevator has a triangular shape with a sharp apex. Dentists call the instrument a “goat leg” differently. Using a sharp tip, the patient cleans the carious cavity from dead particles of dentin and enamel, as well as pathogenic bacteria.
The elevator is used by the dentist to remove tartar.
The specialist decides which tool to use in a particular case. He makes his choice depending on the complexity of the situation and the structure of the affected unit.