Generalized periodontitis is a type of oral disease that belongs to the group of inflammatory diseases and affects periodontal tissue. Its course is accompanied by bleeding gums, swelling, and unbearable pain. The situation is aggravated by the occurrence of bad breath, the appearance of dental plaque, and the formation of periodontal pockets.
Only a competent periodontist can diagnose the disease by examining the oral cavity and performing a biopsy of the gum tissue. Treatment involves the use of medications and surgery. General and immunomodulatory therapy plays an important role.
Periodontitis is a condition in which diffuse disruption of the periodontal complex occurs. The disease affects several teeth at once, and in particularly serious cases, all teeth. This is one of the most difficult problems in dental practice. The generalized form of the disease is 5 or 6 times more likely than caries, leading to partial or complete adentia. And the prolonged development of infection in the oral cavity is the cause of the formation of rheumatoid arthritis, infective endocarditis, atherosclerosis, stroke, and heart attack.
What is periodontium, its features
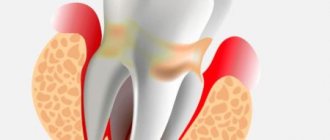
In dental practice, the term “periodontium” is used. It includes a whole complex of tissues surrounding the teeth. They all have a common nerve origin and a single blood supply, therefore they are closely related to each other. The periodontium forms several constituent elements: gums, bone tissue, periodontium, cement of the root system of the teeth. Its functions include providing support, maintenance, and protection of the entire dental system. Pathologies associated with periodontal damage include conditions such as gingivitis, periodontal disease, tumors, and periodontitis.
Reasons for the development of generalized periodontitis
The precursors to the formation of the disease are some exogenous and endogenous factors. The first group is small; most of the diseases of this system are provoked precisely by the internal state of the body. All etiological factors are classified into local (plaque, tartar, problems with bite, abnormal position of teeth, strands of the mucous membrane) and general (diseases of the body - diabetes mellitus, goiter of toxic origin, excess weight, hypovitaminosis, hepatitis, gastritis, etc. ). All this one way or another affects the condition of the periodontium and leads to a deterioration in its functioning.
Microbiological studies have been able to prove the fact that the leading role in the development of this condition is given to microorganisms called Prevotella Intermedia, Bacteroides forsythus, Peptostreptococcus, etc. In order for the dental system to be protected from their influence, protection in the form of plaque is provided in the dental plaque , accumulated in the gingival sulcus, periodontal pockets, and tooth roots.
The life products of pathogenic organisms contribute to the activation of the secretion of certain substances (prostaglandins, cytokines, enzymes), which lead to the destruction of periodontal tissue structures. Factors that entail a decrease in local and general protection from the influence of pathogenic bacteria include:
- smoking,
- radiation damage,
- ignoring the rules of personal hygiene regarding the oral cavity.
The development of this condition is usually preceded by inflammation of the gingival margin, which entails disruption of the connection, destruction of the ligamentous apparatus, and resorption of the alveolar bone. These changes lead to pathological mobility of teeth, overload of their individual groups, and occlusion. In the absence of adequate therapy, this disease provokes tooth loss or removal, as well as problems with the functioning of the jaw system as a whole.
Causes
Inflammation of periodontal tissues flows from the acute phase into the chronic phase if treatment is not started in time and the causes are not eliminated.
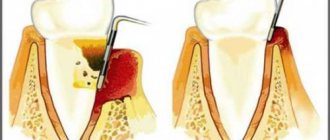
Most often, the trigger is insufficient care. Food debris and dental plaque are sources of pathogenic bacteria that cause irritation of soft tissues. A prolonged inflammatory process leads to the gum moving away from the tooth and forming a so-called periodontal pocket, where dirt and bacteria accumulate. They increase inflammation and tissue loss, causing a reduction in the volume of the gums and jawbone. As a result, the neck of the tooth is exposed, it loses stability, becomes loose and eventually falls out.
Additional risk factors contributing to the development of chronic periodontitis include:
- unbalanced diet, lack of vitamins and microelements
- lack of chewing load
- smoking
- taking medications that negatively affect the immune system: antibiotics, antidepressants, etc.
- violation of the bite and position of teeth in the mouth
- diabetes, gastritis, endocrine system disorders
Classification and symptoms of generalized periodontitis
If you take into account the depth of the pockets and the severity of bone tissue destruction, the doctor can diagnose three forms of manifestation of the disease. They differ in symptoms and signs.
Mild periodontitis
This stage is characterized by a slight sensation of itching and burning. Bleeding periodically occurs during brushing your teeth and after eating (hard foods - meat, fresh fruits and vegetables). The depth of periodontal pockets reaches 3.5 mm, and a decrease in gum tissue is observed at approximately 1/3 of the height of the root. Pathology may not manifest itself for a long time. Therefore, at the first stage of the disease, patients are in no hurry to contact doctors, which provokes the transition of the disease to more severe forms.
Average degree of periodontitis
During its course, various pathological changes occur in the patient. In particular, the functions of the dental system change. The pocket reaches a depth of 5 mm, the teeth become mobile and slightly loose. Gaps appear between them. The tissue structure of the hole is reduced by half the root. There may be an unpleasant odor coming from your mouth.
Severe periodontitis
This disease is typical for adult patients. The depth of the periodontal pockets exceeds 5 mm, the loss in tissue is more than ½ the length of the tooth root. The gums are subject to severe inflammation and bleed. They come out with purulent discharge. Not only tissue elements are destroyed, but also bone parts. Sometimes the walls between the teeth completely dissolve, leading to severe tooth mobility. In this case, it is almost impossible to preserve them in their natural form.
The more advanced the disease, the more difficult it is to cope with it and choose adequate treatment. And the chances of a full recovery decrease with each step of its progression.
Prevention
Is it possible to avoid inflammation in periodontal tissues? Of course, and in most cases, careful hygiene and regular professional cleaning at the dentist are sufficient for prevention. It is also worth eating more solid foods - fresh vegetables, fruits, nuts. Such food gives the gums the necessary chewing load, promotes self-cleaning of teeth and supplies the body with valuable microelements. However, an additional course of dietary supplements containing calcium, fluoride and vitamin B will also not be superfluous. And of course, you shouldn’t put off correcting your bite, replacing missing teeth and treating caries. Then the likelihood of developing chronic periodontitis will be minimal.
Features of the chronic form of generalized periodontitis
Any other oral disease can be a provoking factor in the development of the disease. Gingivitis, neglect of personal hygiene rules, mechanical damage - all these are obvious reasons for the development of a chronic form of pathology. It occurs in two stages:
- exacerbation, accompanied by throbbing pain in the gums, excessive bleeding, pus discharge, abscesses, fever, inflammation of the lymph nodes (such symptoms often make themselves felt against the background of pneumonia, stressful situations, ARVI);
- remission, which occurs during therapeutic measures; during this time, symptoms do not appear, and nothing bothers the patient.
The further the pathology develops, the longer the exacerbation lasts, and the time of remission gradually decreases.
How the disease develops
There are a number of predisposing factors for inflammation of periodontal tissues. These include diseases that weaken the body’s immune defenses:
- diabetes;
- gastritis;
- hepatitis.
Due to weak immunity, bacteria multiply in the mouth, causing rapid destruction of the soft tissue of the gums. The dentogingival connection is gradually disturbed. Penetrating under the crown, the infection “undermines” the roots and covers the bone. Against the background of these changes, the load on certain groups of teeth increases, which leads to their loosening and loss.
Treatment methods for periodontitis
Treatment of chronic generalized periodontitis is complex and depends on the severity of the manifestation. In general, medical and preventive measures are aimed at solving a number of problems.
- Elimination of symptoms that cause discomfort.
- Relieving inflammation in the oral cavity.
- Strengthening the protective properties of periodontium.
- Prevention of the appearance of dental deposits in the form of stone and plaque.
- Prevention of relapses and exacerbations.
This is the general treatment plan. There are private sets of measures, depending on the stage of progression of the pathology.
Symptoms of the disease
The course of the disease has its own characteristics and is accompanied by various symptoms. Acute generalized periodontitis begins suddenly and is accompanied by pronounced symptoms. Often the onset of pathology is provoked by mechanical injuries, deep immune disorders in the body, and poorly selected dentures. The gums are swollen, bleeding, and painful. There is swelling and pain in the regional lymph nodes. The appearance of purulent abscesses and fistulas is possible. The condition is characterized by: fever, malaise, weakness.
Chronic generalized periodontitis occurs in most cases. It is characterized by cyclicality: alternating exacerbations and remissions of the disease. Symptoms of the pathology at the initial stage are little noticeable: the gums become loose and swollen, discomfort appears while chewing food. There is no mobility of the incisors, the periodontal pockets are shallow, located in the intergingival space. As it progresses, there is a gradual destruction of the ligamentous apparatus, the teeth become loose and shift. Periodontal pockets deepen, exposing the necks of teeth.
Exacerbation of generalized periodontitis is manifested by severe pain in the teeth and gums, increased temperature and deterioration of the patient’s general condition. Abscesses with serous-purulent contents are often found in the oral cavity.
Treatment for periodontitis is essential if you care about your oral health.
Directions of therapy for mild periodontitis
The chronic form of mild periodontitis is treated in stages, here is an approximate diagram.
- First, plaque and deposits formed on the tooth enamel are removed.
- Subsequently, the doctor prescribes topical antibacterial agents. They need to be applied in the form of applications to the affected areas. An important role is played by rinsing the mouth with solutions containing antiseptic components.
- The key to successful therapy is compliance with hygiene procedures (purchase and use of special healing pastes, professional toothbrushes, dental floss).
By providing thorough daily oral care and learning to visit the dentist regularly, you can avoid this sore and prevent worsening if it progresses.
How to save teeth with periodontitis
The main way to save teeth from tooth loss is early treatment. Usually, after a few days of treatment, the pathological mobility of the teeth disappears. Preventative measures are of great importance in preventing edentia.
Prevention of periodontitis is divided into several types:
- Nonspecific - includes measures aimed at increasing the general resistance of the body and eliminating predisposing factors. This includes:
- to give up smoking;
- balanced diet;
- adequate treatment of all somatic diseases, especially chronic ones (diabetes mellitus, stomach and intestinal diseases);
- hardening.
- Specific - implies good oral care. These include:
- daily oral hygiene;
- professional teeth cleaning;
- use of pastes that strengthen enamel as indicated;
- the use of additional care products - dental floss.
- Secondary prevention is a set of measures whose task is to prevent relapses of periodontitis and its complications. Patients who have already encountered this pathology should consult a doctor every six months to avoid relapse. This includes treatment of all pathologies of the oral cavity, including dental prosthetics, since adentia is a significant risk factor for periodontitis.
In general, the prognosis for this pathology is relatively favorable, but only if you consult a dentist in a timely manner.
Our clinic has all the conditions for high-quality treatment of periodontitis. The latest equipment and competent specialists allow us to minimize the number of relapses and completely eliminate complications. Contacting the DENT Academy for tartar removal is guaranteed to prevent the occurrence of periodontitis.
Treatment of moderate periodontitis: possible options
If the disease is of moderate severity, therapy will take longer. In addition to these procedures, the complex should include the removal of decayed teeth and the use of steroidal and non-steroidal anti-inflammatory compounds. Also, to improve the general condition, doctors prescribe physiotherapy procedures:
- exposure to affected areas through short-wave ultraviolet radiation;
- carrying out a special massage of the gums, which can be vacuum, vibration, etc.;
- darsonvalization procedures;
- local hypothermia;
- electrophoresis.
Upon completion of treatment, it is necessary to make a follow-up visit to the doctor so that he can assess the general condition and make a prognosis.
Treatment methods for generalized severe periodontitis
Chronic periodontitis, the course of which has moved to the last, most dangerous stage, requires not only careful conservative therapy, but also surgical intervention. Indeed, at this stage, tissue destruction is pronounced, and conventional antibiotics are not enough. You will need to undergo a number of procedures aimed at restoring the affected areas and replacing teeth. Depending on the overall picture, the following types of surgical interventions are prescribed:
- removal of teeth with a high degree of mobility;
- vertical dissection of the gum wall in order to scrape tissue that has undergone pathological changes;
- horizontal excision of the pocket wall together with the affected gum (if the depth of the periodontal pockets is more than 4 mm);
- flap surgery (coronal displacement, lateral, therapy, transplantation, etc.);
- abscess incisions;
- plastic surgery in the frenulum of the tongue, lips.
An important role in the treatment of this form of the disease is played by the use of anti-inflammatory drugs, vitamin compounds, and drugs that strengthen immune function. The prognosis of the disease at this stage is unfavorable, since exacerbation does not entail remission and lasts almost constantly. In addition to tooth loss and gum decay, there is the possibility of systemic complications.
Periodontitis and periodontal disease - differences
Despite the similarity of the clinical picture of periodontitis and periodontal disease, these diseases have certain differences in etiology and pathogenesis. The main difference: periodontitis is of an inflammatory nature, and periodontal disease is of a primary dystrophic nature. Periodontitis is characterized by a bright course of the pathological process, and periodontal disease proceeds more slowly and unnoticeably.
In the pathogenesis of periodontal disease, disruption of the nutrition of periodontal tissues and disruption of the blood supply to the gum tissue are of key importance. With periodontitis, these disorders are secondary in nature and are caused by an infectious lesion.
With periodontal disease, the leading symptom is the exposure of the necks of the teeth, while the teeth themselves retain sufficient strength of fixation, in contrast to periodontitis, in which pathological mobility of the teeth is very common.
When examining the gums of patients with periodontal disease, attention is drawn to their atrophic appearance - pallor of the mucous membrane, its thinness, often accompanied by retraction.
The differences between periodontal disease and periodontitis are more clearly reflected in the table.
| Periodontitis | Periodontal disease | |
| Causes | Insufficient oral hygiene, decreased immunity | Presumably hereditary |
| Etiology | Infectious nature - penetration of bacteria into periodontal pockets | Dystrophic process accompanied by slow destruction of periodontal tissue |
| Character of the current | Aggressive, often recurs | Sluggish process |
| Tooth mobility | Appears very early, with proper therapy it is completely eliminated | Occurs very late, difficult to treat |
| Volume of lesion | Only one tooth may be affected, or it may be generalized | Both dentitions are always affected |
| Nature of gum damage | Deep periodontal pockets | Periodontal pockets may be absent, and severe gum recession is often observed |
| Gingivitis | Occurs in almost 100% of patients | Not expressed |
| Tooth hypersensitivity | Usually observed during periods of exacerbation | Always present |
What to do to avoid complications
To avoid complications, it is necessary to recognize the disease in the early stages and take measures for adequate treatment. All this will allow you to achieve stable and long-term remission and preserve the functions of your teeth and gums. In order for the dental system to be healthy, it is necessary not only to observe the rules of personal hygiene, carrying out regular care procedures, but also to periodically visit a specialist who will perform professional cleaning in order to remove minor dental deposits.
General symptoms of the disease
In the initial stages, the patient suffers from severe bleeding gums. They become loose and swollen. The patient feels itching, throbbing, severe burning, pain when he chews food. An unpleasant odor begins to emanate from the mouth. Dental pockets at this stage are shallow, they are located mainly in the interdental spaces. At the initial stages, the teeth are motionless and not displaced anywhere. The patient's general condition is normal.
The clinical picture of the developing disease is somewhat different. In addition to the above symptoms, the patient may experience:
- displacement of teeth and their loosening;
- high sensitivity of teeth to external irritants (temperature fluctuations);
- problems chewing food;
- disturbance of general well-being (typical of severe forms of pathology), accompanied by weakness, malaise, and increased body temperature;
- an increase in the size of regional lymph nodes, which in addition become painful;
- during a dental examination, the doctor observes signs of diffuse gingivitis;
- Plaque and deposits accumulate abundantly on the teeth;
- tooth loss, fistula, abscesses (signs are characteristic of advanced stages of the disease).
In the case of a chronic form of the disease, the gums have a pale pink tint. There are no dental deposits, manifestations of pus or blood. There is a possibility of exposure of the roots of the teeth. X-ray does not show signs of bone resorption.
Signs of chronic periodontitis
Like any other dental disease, it is better not to let chronic periodontitis progress. The presence of at least two signs from the list of symptoms below is a reason to consult a periodontist:
- itching and burning in the gums
- discomfort/pain when chewing and brushing teeth
- loose teeth
- bleeding and purulent discharge
- bad taste in the mouth, bad breath
- the appearance of pockets in the gums
- food getting into gum pockets
- increased sensitivity of the necks of the teeth
- inflammation of the gums
The course of chronic periodontitis in the early stages is subtle and in many cases causes almost no concern to the patient. Symptoms may smooth out and sometimes disappear completely: it seems that the ailment was temporary, the disease has receded and treatment is not required, but this is a dangerous misconception. In fact, the process of tissue damage that has begun cannot be stopped without treatment, and in the absence of appropriate therapy, the symptoms will soon return and become more pronounced.
Diagnosis of generalized periodontitis
In identifying the disease, a special role is played by the clinical picture and the “age” of the disease. If there are concomitant diseases, the doctor can refer the patient for examination to other doctors - an endocrinologist, therapist, gastroenterologist, immunologist, rheumatologist, etc. When analyzing dental status, the doctor should pay attention to the following criteria:
- the amount of deposits on the teeth;
- their character;
- general condition of the gums;
- depth of the vestibule of the oral cavity;
- features of bite;
- condition of the bridles;
- degree of tooth mobility;
- formation of periodontal pockets.
As part of the initial examination, a Schiller-Pisarev test is taken and the periodontal hygiene index is determined. The doctor also examines scrapings from the gum pocket using PCR diagnostics and saliva chemiluminescence. Among additional diagnostic methods, it is recommended to conduct a biochemical analysis of blood fluid for glucose and CRP. Of no small importance is the determination of IgA, IgM, IgG indicators.
To identify the stage of development of the disease, the following is used:
- orthopantomography,
- x-ray of the intraoral cavity,
- biopsy of gum tissue.
Doctors pay special attention to differential diagnosis with pathologies such as gingivitis, periodontal disease, periostitis, and osteomyelitis. Like therapy, diagnosis must be comprehensive and include several examinations to make the most accurate diagnosis.
Diagnostics
To determine the disease and its severity, various diagnostic methods are used. For generalized periodontitis, differential diagnosis includes an extensive consultation examination to draw up a medical history (formation plan):
- collection of complaints (mobility of units, discomfort when chewing, periodic sharp pain in the attached gum);
- visual and instrumental examination (gingival pockets, recession of gingival tissue, dental plaque, reddish gums);
- determination of the color, shape and structure of gum tissue;
- finding out what condition the dental units are in: percussion, palpation, degree of mobility;
- determination of hygiene indices;
- RG images.
Sometimes, a specialist may prescribe a blood test to clarify the etiology.
Diagnostic measures should take into account not only all the symptoms of the pathology and the patient’s complaints, but also the mandatory performance of an X-ray. Basically, in case of periodontitis, it is recommended to perform an OPTG (orthopantomogram) - a panoramic image. In such an extensive image, all dental structures and the degree of bone damage in each unit are immediately visible.
Periodontal measures for moderate disease
If the disease has become moderately severe, selective therapy is added to the above measures. It is aimed at grinding the surface of teeth that have undergone occlusion, removing deposits under the gums, applying therapeutic dressings and compresses. Along with this, questions are being resolved about whether it makes sense to remove roots or individual teeth, and whether it is worth carrying out splinting and orthopedic therapy. Local anti-inflammatory procedures are usually complemented by general therapy.
Is it possible to cure chronic generalized periodontitis?
In the process of getting rid of generalized forms of severe periodontitis, surgical manipulations are added to the listed methods. As part of these procedures, teeth with 3-4 degrees of mobility are removed, patch surgery is performed, abscesses are opened, etc. Based on the available indications, plastic surgery of the vestibule of the oral cavity and frenulum is performed. If the disease is accompanied by a particularly severe course, systemic anti-inflammatory therapy, immunomodulatory treatment, and vitamin intake are mandatory measures.
Physiotherapy takes part in complex therapy. In particular, the doctor prescribes electrophoresis, darsonvalization, laser treatment, hirudotherapy, herbal medicine, and apitherapy. Activities must be carried out under the supervision of a treating specialist in compliance with all his instructions. Violation of the treatment regimen is fraught not only with a lack of effect, but also with a complication of the general condition.
Why you can’t install removable and bridge dentures against the background of advanced periodontitis
Loss of bone tissue and widening of the sockets during periodontitis create a very ambiguous situation: on the one hand, long-term conservative treatment in the later stages is rarely effective, on the other hand, prosthetics are also difficult, and the problem of missing teeth needs to be solved. However, not every treatment method is suitable.
Why are dental bridges not suitable?
Teeth with periodontitis are weakened and are on the verge of falling out; it is strictly forbidden to use them as support for a denture. The bridge will be movable along with the teeth on which it is attached. The risks are high, even if complex and long-term treatment was carried out before.
Why are removable dentures not suitable?
In fact, after a course of treatment for periodontitis (or closer to the middle of it after acute inflammation has resolved), removable dentures can be installed to solve the problem of partial absence of teeth. But only for a short time, because... When used long-term, they lead to many problems:
- do not stop bone atrophy, but only aggravate this process,
- put increased pressure on the gums and can provoke inflammation, which is extremely undesirable during the course of therapy,
- will require regular correction, since during treatment the damaged tissues are restored, which means the level of the bone with the gum will change - the dentures will no longer fit tightly, will shift, dangle,
- if teeth are partially missing, there is nothing to attach them to - as in the case of bridges, it is better not to use living teeth for support, especially if they are mobile,
- if the teeth are removed scatteredly, then removable dentures will not work at all; the minimum segment is 2-3 missing teeth in a row.
That is, removable dentures can provoke the development of periodontitis and negate all the results of a course of complex treatment. In addition, they are difficult to get used to - more than half of patients are not satisfied with them either in aesthetics or functionality.
Forecast and preventive measures
If treatment is started in the early stages of the pathology, this leads to remission and the possibility of its extension. In restoration measures and in the process of preserving tissue functions, compliance with recommendations related to the implementation of preventive measures plays an important role. If the disease is advanced, the prognosis is unfavorable. This may be due not only to the loss of almost all teeth, but also to the fact that severe systemic complications will begin to develop, especially in the cardiovascular system.
The preventive complex involves compliance with a number of care and hygiene measures:
- timely brushing of teeth;
- a competent choice of cleaning products and tools - toothpastes, powders, brushes, threads;
- regular implementation of professional hygiene;
- timely treatment of emerging diseases;
- removal of deposits from the teeth;
- carrying out treatment of concomitant pathologies.
With these simple measures you can prevent illness and feel great.
Thus, generalized periodontitis is a serious disease that tends to constantly develop and progress. In this regard, it is necessary to diagnose it in a timely manner and take therapeutic measures. This approach will prevent complications and keep all teeth normal, eliminating unpleasant symptoms and improving the patient’s well-being.
Treatment of generalized moderate and severe periodontitis
Open and closed curettage of periodontal pockets
Laser gingivectomy in the area of one tooth
Splinting teeth for periodontitis with fiberglass and tape
The roots of the teeth are exposed - what to do and how to treat them
Laser gingivotomy - surgical treatment of complex forms of periodontitis
The danger of periodontitis: why it occurs and how to treat it
Table of contents
- Periodontitis – what is it?
- Causes of periodontitis
- Symptoms and complications
- Classification
- Severity of periodontitis
- Forms of periodontitis
- Types of periodontitis by degree of localization
- Diagnosis of periodontitis
- How to treat periodontitis?
- Preventive measures
- Advantages of treatment at MEDSI
Periodontitis is a common dental disease that affects about 90% of the adult population of the planet. Just like caries, it leads to tooth loss. But while almost everyone knows about the dangers, causes and prevention of caries, periodontitis still remains a little-known disease for many.
Periodontitis – what is it?
Our teeth are surrounded by what is called periodontium. It consists of gums, blood vessels, connective and bone tissue. The periodontium provides nutrition to the hard tissues of the tooth and the alveolar process (the part of the jaw in which the tooth sockets are located). And it holds the tooth tightly in its place.
Periodontitis is an infectious inflammation of the periodontium. Most often it is preceded by gingivitis, in which the surface of the gum becomes inflamed. Bleeding and discomfort appear. With periodontitis, inflammation penetrates deeper, and symptoms may intensify.
If the disease is not treated, it progresses to periodontal disease, in which bone tissue is destroyed and teeth begin to fall out.
Causes of periodontitis
Periodontitis is caused by bacteria. And those factors that create a favorable environment in the oral cavity for their nutrition and reproduction are the cause of this disease. These include:
- Poor oral hygiene.
After eating, food particles remain in the spaces between the teeth, in the gum pockets (the depression between the gum and the tooth tissue). This is an excellent breeding ground for bacteria to grow. And the less often or carelessly we brush our teeth, the greater the chance of developing inflammation. - Tartar.
Every day, plaque, a biofilm of bacteria, forms on our teeth. Having hardened, it forms tartar, which provokes inflammation of the tissues adjacent to the tooth. - Injury to the gums
by hard food, a poorly fitting filling or crown, a hard toothbrush, etc. Wounds are a favorable environment for pathogenic microorganisms
Factors contributing to the development of periodontitis also include:
- Untreated dental inflammation (they spread to nearby tissues)
- Weakened immunity due to vitamin deficiency, poor nutrition, constant stress
- Smoking and chewing tobacco
- Hormonal imbalances
- Reduced amount of solid food in the diet and, as a result, bone tissue atrophy
- Genetic predisposition
Symptoms and complications
The insidiousness of periodontitis is that most often it proceeds calmly, without pain.
. His symptoms are unpleasant, but not disturbing enough to rush to the hospital. And during a routine dental check-up, they often even forget to mention them. Therefore, the disease is not treated for years until it becomes advanced.
Be sure to see a doctor if you notice at least one of the following signs
:
- Gums bleed when brushing teeth
- You have bad breath that does not go away after rinsing or brushing your teeth
- The gaps between teeth have increased
- Some areas of the gums are bright red
- A gap has appeared between the tooth and gum - a “pocket”
- Enamel has become sensitive to cold and hot
- There is a permanent yellow coating on the area of the tooth adjacent to the gum
- The teeth seemed to become thinner at the base, lengthened
- Pus comes out of the gum pockets
- You feel pain when chewing and brushing your teeth
Initiating a disease is dangerous. Over time, inflammation destroys tissue, periodontal pockets enlarge, teeth no longer adhere to them and eventually fall out - even healthy ones, untouched by caries.
Classification
To choose the right treatment strategy, the doctor determines the type of periodontitis. The disease is classified according to severity, severity, and localization.
Severity of periodontitis
Depending on the severity of periodontitis, there are:
- Mild degree
, when a person is
only bothered by bleeding and discomfort
while brushing his teeth. At this stage, no more than a third of the tooth root is destroyed, and the depth of periodontal pockets is up to 3 mm - Medium degree
, in which the pockets deepen up to 6 mm, and degenerative (destructive) processes affect up to half of the tooth root.
The patient at this stage notices that the teeth begin to loosen - Severe degree
, during which the appearance of the dentition changes - the interdental spaces increase, the roots of the teeth are exposed.
Gum pockets enlarge and become centers of purulent inflammation as food gets into them. More and more periodontal tissue is destroyed, teeth begin to fall out
Forms of periodontitis
Based on severity, the disease is divided into acute and chronic forms.
Acute periodontitis
usually accompanied by severe pain at the site of inflammation, the appearance of purulent abscesses (abscesses), and the formation of fistulas through which pus comes out. Possible fever and general weakness. There is only one plus - with the acute form they often go to the doctor and begin treatment for periodontitis, which usually prevents its transition to a severe advanced stage.
Chronic form
Periodontitis in the early stages manifests itself mainly only by bleeding gums and bad breath. Almost nothing bothers the patient, but in the meantime the periodontal tissues become inflamed and destroyed. The hidden form is most common.
Types of periodontitis by degree of localization
According to the degree of distribution, they are distinguished:
- Local form
, when only a separate area is affected - Generalized form
, when the pathological process covers a large periodontal area
Diagnosis of periodontitis
First, the doctor needs your detailed description of the problem. In the early stages, even an experienced dentist may not notice the disease - there are almost no external signs. And based on your complaints, he will definitely prescribe additional studies.
To correctly diagnose the disease and determine its severity, the dentist uses:
- Oral examination
- X-ray or computed tomogram - to assess the condition of periodontal tissues and tooth roots
- Rheoparodontography, in which a weak current is passed through periodontal tissue. It is used to study the tone of blood vessels in the area under study. The more severe the stage of periodontitis, the more negative changes in the circulatory system the study determines
- Ultrasonic osteometry, which assesses the degree of destructive changes in bone tissue
- Schiller-Pisarev test, when the oral cavity is treated with a special solution. Affected and healthy tissues after treatment have different color intensities
- Determination of the bleeding index
- Determination of periodontal index
- Microbiological studies of the oral cavity - to determine the type of pathogenic microorganisms that caused inflammation
- Clinical tests of urine and blood - to identify factors contributing to the development of periodontitis, as well as the general condition of the body
A set of diagnostic measures helps determine the causes, severity of the disease, and the extent of its spread. Additional studies help determine contraindications and features of the use of therapy. As a result, the doctor makes an informed decision about treatment methods.
How to treat periodontitis?
Modern methods make it possible to cure even severe forms of periodontitis. But it will not be possible to restore already destroyed tissues in any case. That is why periodontitis should not be allowed to progress to a severe form.
The treatment regimen for periodontitis usually includes:
- Elimination of sources of infection
. Sanitation of the oral cavity is carried out: treatment of carious teeth, removal of tartar, cleaning of periodontal pockets - Regular thorough oral hygiene
. The dentist explains to the patient how to brush their teeth correctly and how often. Recommends medicated toothpastes and rinses - Destruction of bacterial infection
in periodontal tissue. Usually the fight is carried out both at the local level (antibacterial ointments, applications, rinses) and at the systemic level - antibiotic injections or tablets are prescribed - Strengthening the immune system
with multivitamin complexes, mineral supplements, immunomodulatory drugs - Correction of bite
, incorrectly installed crowns or fillings that caused inflammation - General strengthening, restorative therapy
for periodontal tissues using physiotherapeutic procedures and medications - Correction of damaged tissues and dentition
in advanced cases. Surgical methods are used here
Let's look at what procedures and medications are used to treat periodontitis.
- Ultrasonic, hardware or laser cleaning of tartar and gum pockets
- Rinsing the mouth with antiseptic preparations
- Treatment of gums with antiseptic, antibacterial ointments and gels
- Physiotherapeutic procedures - UHF, electrophoresis, ultrasound, gum massage, balneotherapy and so on
- Dental splinting is a surgical operation in which teeth are held together with a special tape to prevent them from falling out.
- Flap surgery in which a flap of gum is cut away and periodontal pockets are opened and cleaned out. The flap is then sutured into place to cover the exposed roots and strengthen the gum.
- Augmentation of destroyed bone tissue and other surgical interventions
Traditional methods of treatment can only be used in combination with therapy prescribed by a doctor, and only with his approval. By themselves, they most often are not able to cope with periodontitis.
Preventive measures
Treatment of periodontitis is a complex process. Therefore, it is best to prevent its development. Prevention measures include:
- Regular dental examinations
(at least twice a year) - Thorough and proper brushing of teeth
. The brush should be of medium hardness, the brushing movements should be directed towards the cutting edge of the teeth, the duration of the procedure should be at least 5 minutes - Regular professional dental cleaning
in the clinic - Rinsing the mouth after eating
- Regular use of dental floss or irrigator
- Including solid foods in your diet
, which improves blood supply to the gums and jaw bone tissue, and also naturally cleanses plaque from teeth - Be careful with the
oral mucosa and prevent injury to it - Maintaining good overall body tone, strengthening the immune system
- Timely replacement
of missing teeth - Regular gum massage
is a simple procedure that you can do yourself. To do this, just massage your gums with your fingers for 5-10 minutes (after washing your hands) - Timely treatment of common diseases
Advantages of treatment at MEDSI
The MEDSI clinic network offers professional diagnosis and treatment of periodontitis using modern methods, as well as preventive measures, such as professional cleaning of plaque and tartar.
The advantages of contacting us are:
- Comprehensive consultations
. Often the problem affects several areas of dentistry, for example, therapy and prosthetics. In this case, your doctor will definitely invite related specialists for a consultation. - Drawing up a transparent and detailed financial treatment plan ,
which will help you plan expenses and give you the opportunity to “freeze” prices for services - Comfort
. Comfortable waiting areas and reception rooms, the use of modern diagnostic and treatment technologies give you a feeling of comfort throughout your stay in the clinic - Excellent technical equipment
. Our clinics can carry out all the necessary diagnostic examinations, including cone beam computed tomography. All equipment is from leading European manufacturers - Possibility of treatment during sleep
, using gentle medical sedation (anesthesia). This treatment will help to completely avoid discomfort and carry out extensive work in a short time.
You can be sure that in our clinics you will receive an accurate, comprehensive diagnosis, prescribe the correct treatment and carefully monitor its effectiveness.