In the practice of dentists, there are often cases when a patient’s tooth is fully formed, but does not erupt. It is called “retained”, and the problem is treated with special methods. Teeth that are formed but “stuck” inside the jaw can cause inflammatory processes: pericoronitis, periodontitis, periostitis, abscess, phlegmon, etc. Treatment is carried out using various methods, from removal to wearing specialized braces. Reduce the risk of impacted tooth Prevention helps, for example, wearing trainers that prepare the jaw for the appearance of new teeth.
What is retention? Why does pathology develop? Symptoms and diagnosis
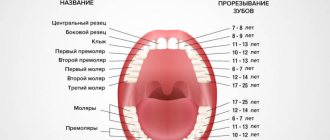
Retention is considered one of the most common teething anomalies. Most often, problems arise with the lower and upper “wisdom teeth”, which grow incorrectly. They are usually encountered by adults. In children, a common impacted tooth is the canine of the upper jaw. The second premolars of the mandible often present unpleasant surprises.
Symptoms of unerupted teeth vary by owner. The problem may not manifest itself at all, or it may cause constant visits to the dentist. The variety of symptoms and their absence is due to the fact that the incorrect position of a tooth or its incomplete eruption is an almost natural phenomenon for humans. Approximately 35-45% of “wisdom eights” in adults are impacted teeth . Difficulties begin to arise when such a molar or premolar causes irritation of the soft tissue around it. Based on indirect signs - pain or inflammation - the doctor identifies the “wrong” tooth.
Semi-retinated teeth are visible immediately at the first examination: they partially grow, but not completely. Such partially erupted molars and premolars cause many more problems: being partially located in the soft tissues, they almost always cause inflammation. There is no need to specifically diagnose them: the doctor almost always finds such teeth during a routine examination.
Finding completely impacted teeth is a real quest. They may not be visible at all, because they are located under the existing elements of the dentition. In this case, there is only one diagnostic option: you need to take a full picture of the jaw, which will clearly show the whole picture. Below in the picture is a selection of examples. Impacted teeth are marked in red or with arrows.
Examples of impacted teeth on x-ray
Is it possible to diagnose retention yourself?
Yes, it is possible, but it is always necessary to additionally consult with a doctor who will decide on the future fate of the retention. Usually around the pathology there are:
- swelling and redness of tissue in the eruption zone;
- pain;
- pulsation;
- the patient feels weak;
- there may be an increase in temperature.
Sometimes retention can occur without symptoms or with muted symptoms, but at an appointment with a dentist, the pathology will be immediately diagnosed.
Unfortunately, the consequences of retention cannot be predicted, but most often cysts and granulomas form on such teeth. There is also a high probability of malocclusion due to the strong pressure of such a tooth on healthy ones.
Types of dental retention
There are many classifications of dental retention. One of the most popular methods of division is by degree of eruption. Thus, there are semi-impacted teeth , which are partially visible in the gum, and completely hidden - located under the gum or bone tissue. The latter are not available for palpation. If the impacted tooth is located in the gum tissue, the diagnosis will say “with tissue immersion,” but if it is located in the bone, “with bone immersion.”
Another classification method takes into account the position of the molar, canine or premolar:
- vertical,
- horizontal,
- corner.
Horizontal teeth can also be transverse, sagittal or oblique, and angular teeth can be mesial, distal, lingual or buccal angular. Rarely, but still there are reverse impacted teeth - these are elements that grow “upside down”, that is, their crown is directed towards the jaw.
Types of anesthesia
Performing surgical interventions is impossible without high-quality anesthesia. During extractions, the following types of anesthesia can be used:
- infiltration anesthesia – provides a local effect. Injected with a syringe into the gum or intraosseously. This is the most common option for dental procedures;
- conductive - has a more powerful effect and is used when operating on particularly complex cases. The injection is carried out to the branches of the trigeminal nerve;
- intraligamentary - used to anesthetize one tooth. The medicine is injected with a syringe into the ligament that holds the tooth in the alveolus.
Expert opinion: Some patients want dental surgery to be performed under general anesthesia. But this type of anesthesia is not as harmless as it is described in advertising articles. It has been proven that it negatively affects the patient's health. An operation to remove teeth, even such complex ones as the “eight”, is not a direct indication for the use of general anesthesia (with rare exceptions). Surgery is painless with the correct selection of local anesthetic. Therefore, you should not strive for general anesthesia and put unnecessary drug burden on the body.
Causes of impacted teeth. Is it possible to prevent retention?
The most popular reason for impacted teeth is genetic predisposition. Moreover, what is inherited is not the desire of the canines and molars to grow “some into the forest, some for firewood,” but the structure of the jaw. It can be narrow, which is why there is simply not enough space for all the necessary elements of the dentition. But there are other reasons:
- malocclusion, which has formed due to harmful myofunctional habits or mechanical injuries;
- early loss of baby teeth, due to which permanent teeth do not have guidelines for growth;
- “extra” teeth – atavism, called polyodontia;
- initially diseased tooth germs.
In some cases, retention problems can be prevented. Some orthodontists and pediatric dentists recommend the use of trainers to develop the dental arch and give growing canines and molars a guideline for eruption. If the problems are hereditary, only timely treatment will help.
You can read more about trainers in the article: Trainers for straightening teeth: description, varieties, tips for use
Treatment of dystopic upper canines
The upper canines are critically important teeth for the dentition, given the characteristics of their morphology, position, protective function in the structure of occlusal interactions, as well as the volume of visualization in the smile profile. The proper position of the canines in the dental arch is one of the criteria for the predicted stability of the results of dental treatment.
Dystopia and tooth retention can develop due to physical blocking by other teeth, thickening of bone tissue or mucosa due to the presence of supernumerary teeth, odontoma or some other tumor. The third molars of the lower jaw are characterized by the highest prevalence of cases of dystopia and retention, while the second place is occupied by the canines of the upper jaw. During eruption, the upper canines must travel a significant distance from the lower edge of the orbit to the edge of the bony ridge when all other anterior teeth have already erupted. The prevalence of dystopia and retention of the upper canines is about 2%, and among women this pathology occurs 2-3 times more often than among men. About 66% of cases of dystopia and retention of the upper canines are situations with their displacement in the projection of the palate, while the remaining 33% fall on dystopia in the vestibular position. Bilateral dystopia is noted with an 8% prevalence rate. In Latin American countries, according to publications by authors from Colombia, Mexico and Brazil, the prevalence of canine dystopia is almost the same as in Europe or the USA. However, countries such as Greece or Turkey, for example, are characterized by a slightly higher level of registration of cases of the above-mentioned pathology (at a rate of approximately 4%).
Dystopia of the upper canines can cause displacement of other teeth, cyst formation, resorption of the roots of the lateral incisors (especially when their roots are oriented palatally), the development of localized and widespread pain, as well as inflammatory disorders. Clinicians should be aware that there may be a difference of up to 6 months between the child's chronological age and the age of canine eruption to ensure that there is no developmental or eruption disorder. Only the clinical sign of the absence of a canine tooth in the dentition at the age of 12 years is not a dominant criterion for making any diagnosis. Timely diagnosis and appropriate interventions allow a more optimal approach to the issue of proper occlusal correction. If early interventions are unsuccessful, a multidisciplinary approach to treatment may be necessary, which involves the implementation of surgical and orthopedic phases of intervention.
Causes of dystopia
Potential causes of dystopia suggested by Becker and Chaushu include: increased size of the tooth germ, odontoma, the presence of an unerupted tooth in the path of the problematic unit of the dentition, delayed eruption of adjacent teeth, and the presence or absence of lateral incisors. Three main criteria must be considered to properly evaluate dystopic maxillary canines: diagnostic principles, treatment plan, and biomechanical principles. To adequately assess the existing disorder, it is necessary to use both clinical and radiological diagnostic methods. The treatment plan for canine dystopia often involves close collaboration between the orthodontist and the oral surgeon. The implementation of biomechanical principles must take into account the possibilities of effective application and orientation of orthodontic force vectors for therapeutic purposes.
Bishara conditionally divided all the causes of dystopia into local and general. Among the common causes, the author identified disorders in the structure of the thyroid gland, hypovitaminosis of vitamins A and D, infectious diseases, radiation, and several syndromes, including Crouzon syndrome and Down syndrome. Local causes of dystopia include the presence of supernumerary teeth, odontomas, trauma at an early age, cleft lip or palate. Other potential causes are associated with abnormalities in the morphology or position of the tooth germ, disturbances in the eruption path of the canines, ankylosis of the periodontal ligament, prolonged retention or, conversely, too rapid loss of primary canines, iatrogenic causes, bifurcated roots, or the influence of idiopathic factors.
It is generally accepted that the specific cause of buccal retention of the maxillary canines is a lack of space in the dentition or insufficient length of the dental arch. Tomographic studies have demonstrated a relationship between narrow maxillary shape and buccal canine retention. But similar associations were not found for palatal dystopia and maxillary canine retention. Jacobs reported the influence of tooth size discrepancy on the possibility of developing impaction of canines, with canines being more prone to such problems due to their significantly longer eruption path compared to other teeth. Becker suggested that palatal retention of the canines may be caused by a lack of direction from the roots of the lateral incisors (in the absence or morphological deformation of the latter). Other authors have cited genetic causes behind canine impaction, including microdontia of the lateral incisors, enamel hypoplasia, defective eruption of primary molars, or distally disrupted eruption patterns of second premolars. Peck et al associate palatal dystopia and canine impaction with a broader set of chromosomal abnormalities.
Planning of surgical/orthodontic interventions and algorithm for selecting them
To help clinicians determine the optimal treatment method for maxillary canine impaction, an algorithm for selecting surgical and orthodontic types of interventions will be presented below.
Diagnosis of canine retention
The diagnostic process should follow a logical sequence and include a detailed analysis of personal and family history of existing dental disorders, the results of a comprehensive clinical examination, which in turn includes: palpation, X-ray screening through orthopantomography, lateral cephalography and radiography in the superior occlusal projection. It is also recommended to obtain additional targeted images using the Clark method, although from the point of view of cost-effectiveness, orthopantomography is a more reasoned diagnostic approach. For a more detailed analysis, you can use the method of cone beam computed tomography. The latter makes it possible to diagnose root resorption of adjacent teeth, possible transposition between the lateral incisors and canines, as well as the trajectory of the eruption of the canines in cases of its projection over the apical areas of the lateral incisors. In addition, CBCT can identify root splitting and signs of ankylotic changes. According to Ericson and Kurol, CBCT data confirmed evidence of root resorption in 38% of maxillary lateral incisors and 9% of maxillary central incisors due to canine impaction (Figures 1 and 2).
Photo 1. Scan of palatally impacted canines (front view).
Photo 2. Scan of palatally impacted canines (occlusal view).
CBCT method and canine retention
As a valuable X-ray diagnostic tool, the use of CBCT is indicated depending on the amount and nature of the information that the doctor received during the clinical examination. The use of CBCT must be justified taking into account the individual needs of each individual patient. This means that CBCT should not be considered as the first imaging modality in the absence of clinical suspicion of maxillary canine impaction. Localized CBCT imaging is only warranted after careful clinical evaluation and in cases where other radiographic diagnostic modalities do not provide the necessary data to identify or differentiate the pathology. Although it is intuitive to assume that 3-dimensional imaging is certainly superior to 2-dimensional imaging, this assumption has not been completely unambiguous in cases of impacted canines. Systematic reviews comparing diagnostic approaches to the verification and assessment of canine impaction using CBCT and traditional imaging methods have shown that, although CBCT leads to greater consistency in diagnosis, the choice of different treatments for the same pathology by different clinicians - dentists continues to vary. In other words, CBCT does not eliminate differences in existing personal treatment preferences among dentists. Therefore, orthopantomography in many cases remains the most appropriate method of radiological diagnosis. A similar conclusion was reached in studies of angulation and position of impacted canines: although CBCT allows a more accurate assessment of the above-mentioned parameters, the treatment plan for this disorder varies significantly among different dentists, that is, the level of patient-centered effectiveness of impaction treatment canines remains quite low, despite the fact that the tomographic method is used. In summary, there is no convincing evidence that CBCT should be considered a first-line diagnostic modality for assessing maxillary canine impaction, although its use is indicated in cases where 2D diagnostic results do not provide adequate diagnostic information.
Open or closed surgical technique?
In a systematic review of the literature examining treatment options for high palate impacted canines, Parkin et al concluded that the available evidence does not support the conclusion that closed versus open surgical techniques are superior when compared. None of the above-mentioned techniques was characterized by a better treatment outcome in terms of gingival aesthetics, dental health and patient comfort. The authors recommended more detailed randomized trials. In another systematic review, Sampaziotis et al compared the effectiveness of open and closed operative approaches for the management of impacted maxillary canine teeth. The researchers also concluded that the difference in periodontal and esthetic outcomes between the two treatment methods was not significant. The level of postoperative discomfort in patients of both comparison groups was similar. The only difference was that the open surgical technique required less time, although this conclusion was based on the results of only two studies analyzed. In a systematic review with meta-analysis, Cassina et al concluded that the open surgical approach has a lower risk of ankylosis and a shorter required traction period for impacted canines. It should be noted that this systematic review analyzed only a small number of clinical studies. To formulate targeted clinical recommendations regarding the choice of a particular treatment method, the researchers recommended conducting controlled randomized trials. The disadvantage of the method of closed induced eruption of canines is that if the orthodontic appliances used lose stability, additional surgical interventions are required. In addition, since the tooth is located inside the bone tissue, it is much more difficult to control the force vector, therefore, traction is essentially a blind movement. In addition, in cases of closed type interventions, the risk of developing ankylosis increases. This is why many doctors prefer the technique of open canine movement, although no consensus decision on this matter has yet been formed.
Consideration of location early in the treatment of impacted canines
Removing a temporary canine is the simplest method of preventing the development of retention of permanent canines. This manipulation can be performed in isolation, or in combination with the use of a place holder, such as a Nance button or a maxillo-palatal arch. In some cases, a device can be used to expand the dental arch. Jacobs emphasized the importance of correcting the lack of arch space in the upper jaw, and Baccetti, in turn, noted the importance of early expansion of the palate during the mixed dentition period to prevent the development of early signs of retention. Palate expansion is an effective and cost-effective method of restoring arch width to avoid future bite problems. Pediatric dentists should recommend orthopantomographic examination for patients aged 7 to 11 years. According to orthopantomography data, it is possible to objectively assess the proximity of the canine crown in relation to the roots of the lateral and central incisors. After removal of temporary canines, the clinical situation can significantly improve even with signs of resorption of the roots of the lateral incisors. However, you need to understand that early extraction of primary canines does not always work.
In a randomized clinical controlled trial, Naoumova and Kjellberg provided a clear algorithm for the temporary removal of primary canines. When potentially impacted permanent canines are located in sector 2 (between the distal surface of the lateral incisor and the midline of the lateral incisor) or in sector 3 (between the midline of the lateral incisor and the distal side of the central incisor), and their conventional inclination to the vertical plane is 20-30 degrees , removal of temporary fangs is indicated for prophylactic purposes. In cases where the inclination is less than 20 degrees or more than 30 degrees, the extraction of temporary canines will not significantly affect the result of retention of permanent teeth. The same applies to permanent canines impacted in sectors 1 (deciduous canine), 4 (distal central incisor to midline of the central incisor), or 5 (midline of the central incisor to midline of the maxillary arch). The exposure and direction of impacted canines from the surfaces of nearby tooth roots is carried out surgically. The authors proposed to advance the canine first palatally or buccally, depending on the situation, and then distally. In patients with severe crowding, it is recommended to evaluate the response of the impacted canine to traction before deciding whether to remove a premolar.
Recommendations for anchoring impacted teeth
For orthodontic pulling of impacted teeth, a stainless steel arch with a rectangular cross-section or a thick transpalatal beam of a sufficient level of rigidity is used. The use of these traction materials is extremely important in cases of palatal impaction of canines. In the process of orthodontic treatment of these teeth, it is necessary to abandon the use of flexible arches, since their action can provoke the development of undesirable side effects in the area of adjacent teeth during the process of canine traction. Sufficient intra-arch anchorage can be achieved by using 0.019 x 0.025 orthodontic wire in a 0.022 slot. This approach prevents arch deformation, open bite changes, intrusion of adjacent teeth and ensures the prevention of associated complications. Swing gate expanders, transpalatal arches, Hass expanders, quad coils, Hyrax expanders and orthodontic implants can be used as external elements as alternative fixation options. In cases where a transpalatal beam is used, its mechanism of action is to use cantilever extensors to pull the affected canine into the projection of the palate. After this, the canine is directly pulled out and its position is normalized using positional arches (photo 3-4).
Photo 3. A swinging gate-type device for direct traction of palatally impacted canines during the implementation of the open surgical method.
Photo 4. Exposure of a palatally impacted canine. A transpalatal bar was used as an anchor with an additional handle to provide traction on the canine.
Recommendations for activating impacted canines
The vectors of force acting on the canines should ensure their displacement away from the roots of adjacent teeth, especially in cases where impacted teeth are adjacent to the roots of the lateral incisors. With deep palatal retention, activation of the canines must occur first occlusally and then distally to achieve the required position in the dental arch. Elastic chains or threads, nickel titanium springs, extrusion assist springs, ballista springs, cantilever arms, and orthodontic implants may be used to enhance traction. If the development of ankylosis is suspected, the traction force should be reduced and the patient should be referred to a periodontist. In such cases, it is recommended to obtain a plain periapical x-ray to evaluate the presence of osteoid tissue to ensure that the periodontal tissue follows the tooth as it advances.
Treatment time for impacted canines
In assessing the duration of orthodontic treatment, Fink and Smith reviewed six private orthodontic practices and 118 case reports of patients without evidence of canine impaction and concluded that the average orthodontic treatment time was approximately 23.1 months, with a range of 19.4 to 27.9 months. . Another study evaluated the duration of treatment in adolescents with palatal impacted canines using closed orthodontic eruption. In cases of unilateral retention, the average treatment time was 25.8 months, while in cases of bilateral retention it increased to 32.3 months. A similar study was conducted among adults with palatally impacted canines who were treated with the same protocol. The treatment success rate in adult patients was found to be 69.5%, compared to the 100% success rate reported among adolescents. Another interesting discovery was that in all cases of unsuccessful treatment for non-eruptive canine pathology, the age of the patients exceeded 30 years.
The orthodontist is often faced with the problem of creating sufficient space in the dentition before pulling out the canines. This preparatory stage of treatment can take from 2 to 4 months. The position of problematic canines can be assessed by palpation, radiography, or transmucosal probing. Palpation of the unerupted canine allows the doctor to feel a hard, well-defined area that can be used to determine the location of the impacted tooth. If this bulge cannot be detected, an x-ray may be necessary. For this purpose, lateral, occlusal, panoramic and periapical imaging techniques are used. During radiographic assessment, the SLOB rule (“same-lingual, opposite-buccal” - same-lingual, opposite-buccal) is often used: on two images of the same area, taken at different angles of the tube, it is determined in which direction visually “ the problematic tooth moves. For the purpose described above, the method of cone-beam computed tomography can also be used for greater diagnostic accuracy.
Intervention techniques for vestibular retention of canines
Approximately a third of all clinical cases of canine retention occur due to their vestibular transposition. In such cases, use one of the two intervention techniques described above:
1. Gingivectomy, which is essentially the cutting out of gum tissue. In this case, the tip of the canine should be at or below the mucogingival junction. This procedure is indicated when there is a wide area of keratinized gum tissue. It is performed with a special Kirkland knife or a 15th blade with an external bevel. If the canine tip is located coronal to the cemento-enamel junction of the lateral incisor, this is another indication for gingivectomy. At the end of the procedure, at least 3 mm of keratinized gingiva should be accessible apical to the level of the cemento-enamel junction. To place a bracket, at least two-thirds of the surface of the canine crown must be exposed. The disadvantage of this intervention is that the procedure may need to be repeated when the gum tissue is restored, or if there is not enough keratinized gum.
2. The method of creating an apically repositioned flap is an intervention option for a deficiency of keratinized gingival tissue, and is preferable in cases where the canine is localized mesial to the lateral incisor. The flap must be secured and adapted to the tooth. Contraindications to an apically repositioned flap include the risk of gingival recession and irregular gingival margins, as well as the potential need for extensive bone grafting. The primary incision is made using a 15 c ridge projection blade in order to obtain the maximum volume of keratinized gums. After this, vertical incisions are made and the flap is moved in a lateral or apical direction. The design of the flap provides for the same width of the base and the coronal part of the flap, or the base can be slightly narrower; The flap thickness should be 4-5 mm to ensure proper width in the mesiodistal direction, extending to 1.5 mm beyond the corner of the tooth (Figure 5-6). The bone covering the impacted tooth must be removed with a curette or bur to expose the crown surface. The flap is then positioned at the cemento-enamel junction and secured with sutures to ensure proper stability. Depending on the level of retention, a periodontal bandage can be used to prevent overgrowth of soft tissues. The bracket is installed during the flap formation procedure, or after 10 days. If the impacted canine is too apical, a closed orthodontic eruption technique is used. The orthodontic phase in this case begins 4-6 weeks after surgical exposure. In cases where the canine is surrounded by a wide follicle, the flap incision must be made wider than the size of the follicle in order to achieve proper subsequent adaptation of the flap to the tooth and bone tissue. If the flap is adequately adapted, it will not move when the lip moves.
Photo 5. Application of an apically displaced flap during the treatment of bilateral canine impaction. During the manipulation, the median frenulum was cut out and braces were installed.
Photo 6. After the orthodontic phase of treatment, the canines were positioned in the dentition.
Surgical methods for treating palatal impaction of canines
Two surgical approaches can be used to expose palatally impacted canines: an open approach with a trapezius or lunate flap, or a closed approach.
Open surgical method. A semilunar oblique incision is made with the 15th blade or 15c blade from the mesio-palatal side of the tooth, continuing it to the distal palatal side. The incision is made to the entire depth of the tissue to the bone, after which the full-tissue flap is separated using a periosteal elevator. The bone covering the canine is removed using a curette or rotary instrument. The follicle is cut out and scraped to completely expose the fang, creating conditions for fixing the bracket. A ligature is attached to the bracket for traction. Hemostasis is ensured by local anesthesia, bone wax, or a sponge soaked in an anesthetic solution with an adrenaline concentration of 1:50,000. To fenestrate the gum tissue in the projection of the bracket, a new 15c blade is used, thus, as if forming a window for access to the bracket through a flap that is fixed with sutures. A periodontal dressing is used if necessary. In cases where it is necessary to apply direct traction, orthodontic force is applied 2 weeks after the operation; before that, the tooth is given a chance to erupt independently in the direction of the occlusal plane, after which its position in the dentition can be corrected (photo 7-8).
Photo 7. Spontaneous eruption of impacted canines 7 months after surgical exposure.
Figure 8. After the canines had erupted to the level of the occlusal plane, they were placed into the dentition using orthodontic traction. The total duration of treatment was 12 months.
Closed surgical method. When performing this manipulation, an intrasulcular or crestal incision is made with the 15th blade or 15c blade from the premolar to the midline. The full-tissue flap is separated using a periosteal elevator to expose the impacted tooth. Any residual tissue that interferes with the eruption of the canine is removed by curettage. After fixing the bracket and installing the ligature, the flap is fixed into place. The advantage of this approach is the preservation of gingival aesthetics, but the disadvantage is the possible peeling of the bracket due to the lack of dryness of the working field during its installation. Consequently, in some cases there is a need for additional surgical intervention.
Complications during surgical/orthodontic treatment of impacted teeth
Complications that orthodontists may encounter when treating impacted teeth include devitalization, the need for re-exposure, ankylosis, damage to adjacent teeth, and external root resorption. An adequate treatment protocol preserves the integrity of the periodontal attachment. To date, there are no studies explaining the difference in treatment outcomes for impacted canine teeth between adults and adolescents. It has been suggested that the periodontal ligament around unerupted canines atrophies in older patients, thereby slowing their ambulation and making it less predictable. The use of CBCT allows a comprehensive assessment of the morphology of the tooth and root, as well as the surrounding periodontal complex. In cases where there is no ligamentous space or with a hook-shaped apex, more careful planning of the intervention is necessary to avoid the development of ankylosis. The prevalence of ankylosis increases with age, therefore the possibility of successful treatment of impacted canines decreases. Patients should be informed about the risks and benefits of treatment for ankylosed canines so that they can choose between orthodontic treatment and possible extraction or further implantation.
Adverse reactions from the periodontium
An appropriate surgical approach is critical to predict the soft tissue and periodontal condition during the treatment of impacted canine teeth. Rapid movement, heavy loads and poor oral hygiene are most responsible for a possible negative reaction to periodontal treatment. Marginal bone loss, gum recession, and sensitivity are complications of long-term orthodontic treatment. To optimize treatment time, some doctors suggest using approaches with the formation of perforations and tunnels, although other specialists consider these approaches to be periodontally compromising. After all, if during treatment it is nevertheless possible to position the canine into the required position, then the patient will be left with a periodontal defect that requires augmentation intervention to restore the integrity of the tissues.
Root resorption of impacted canine and/or adjacent teeth
In conventional orthodontic treatment of non-impacted teeth, the risk of root resorption is directly related to the duration of treatment. At the same time, the anterior teeth of the upper and lower jaws are more sensitive to the risk of developing root resorption. Other factors associated with a greater likelihood of resorptive damage are anterior retraction, extraction of teeth, significant orthodontic forces and irregularities in the shape of the apical region of the teeth. Remington et al followed a large sample of patients for 10 years after completing their treatment. They concluded that if the development of resorption is associated with treatment, then stopping the movement of teeth under the influence of orthodontic traction will most likely stop the resorptive process.
Ericson et al reported that the likelihood of lateral incisor root resorption was 3 to 4 times higher in women than in men treated with impacted canines. In addition, the diagnosis of resorptive pathology in women using CBCT is more accurate than in men. In general, CBCT can identify 50% more cases of root resorption than 2D x-rays. It is still not completely clear what the mechanism of resorption of the roots of the lateral and central incisors is in cases of treatment of canine retention. Perhaps it is caused directly by the movement of the fang and its pressure on adjacent structures; on the other hand, the cause of the pathology may be an enlarged tooth follicle. Yan et al reported a correlation between the development of root resorption of adjacent teeth and a distance of less than 1 mm between the root resorption and the impacted canine. Dağsuyu's studies could not find any associations between the size of the canine follicle and the resorption of the roots of the lateral incisors. However, the authors reported that lateral incisors with signs of resorption were in close contact with more asymmetrical and enlarged canine follicles. Chaushu stated that when the canine follicle size is greater than 2 mm, the risk of developing root resorption of adjacent teeth significantly increases. If there are signs of resorptive damage to the root of the lateral incisors (even in conditions of only half the formation of the canine root) in patients aged 9-10 years, it is recommended to expose the canines and shift them away from the adjacent teeth. After such distalization of the canines, no orthodontic forces act on them for some time in order to create conditions for the full development of the root. Movement of problematic canines away from incisors with signs of root resorption may promote restoration of cementum over exposed dentin. If there is resorption of the buccal or palatal surface of the root of the lateral incisors, it should be diagnosed before treatment. Pre-existing resorptive lesions rarely cause loss of central or lateral incisors, but require special attention. Vermette found that the roots of impacted canines, after they had fully moved into the dentition, were shorter than normal ones. The most pronounced resorptive signs were found on canines impacted in the middle of the bone crest. In many cases, root resorption can be avoided by physiological movement of the lateral incisors during canine traction.
Summary
Although impaction of the maxillary canines is relatively uncommon among the general population, the frequency of registration of this pathology among dental patients is quite high. Canine impaction requires an integrated approach to diagnosis and treatment. Some clinical cases of canine retention can be solved by removing their deciduous counterparts and using “place holders” - special orthodontic appliances. If it is not possible to achieve an effective result through minimally invasive interventions, then complex surgical and orthodontic treatment is resorted to. This article describes protocols for surgical and orthodontic treatment techniques for cases of palatal and vestibular canine impaction. The doctor must independently choose the most optimal approach, based on the characteristics of the clinical situation and the evidence base. In case of buccal retention, special attention when choosing a treatment method should be paid to the position of the canine relative to the mucogingival border. To correct such clinical cases, gingivectomy, apically positioned flap, or closed surgical technique can be used. For palatal retention of canines, the open surgical method has many advantages over the closed surgical method. However, the latter also has its own specific indications. The use of proper orthodontic traction techniques and consideration of basic biomechanical principles significantly reduces the risk of developing iatrogenic complications. The following three factors are critical to orthodontic success: adequate anchorage in the maxilla, use of an effective bonding protocol, and application of adequately targeted forces of optimal magnitude to provide traction. Possible complications that may be noted during the treatment of impacted canines include the development of ankylosis, resorption of the roots of adjacent teeth, disruption of the gingival aesthetics in the projection of the canines, and the potential need for excessively prolonged treatment.
Authors: Miguel Hirschhaut, DDS Nelson Leon, DDS Howard Gross, DDS, MS Carlos Flores-Mir, DDS, DSc
Why are impacted teeth dangerous?
Despite the fact that sometimes unerupted teeth do not interfere with a person in any way, you need to understand that every impacted tooth is a potential cause of serious and unpleasant diseases. They lead to the following problems:
- inflammatory processes;
- non-healing ulcers on the gums and cheeks;
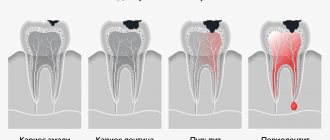
- constant appearance of caries, pulpitis;
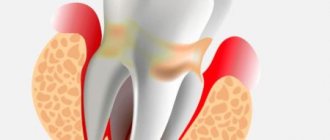
- the appearance of gum pockets, which can cause periodontitis;
- infectious processes, often leading to osteomyelitis (purulent infection of the jaws).
The absence of symptoms is almost always the result of a happy accident, and not a normal development of events. Therefore, with such a diagnosis, it is very important to constantly see a doctor.
Possible complications
When there is an impacted tooth in the oral cavity, dental problems arise over time, which can be used to determine the presence of an impacted tooth:
- the appearance of swelling and soreness of the gums and soft tissues around, aggravated by palpation, an inflammatory process in them;
- redness of the gums, pain reaction in it;
- numbness of the face that occurs due to the pressure of a tightly fitting (not erupted) tooth on the nerve endings;
- pulpitis and caries of neighboring teeth;
- the appearance of an odontogenic cyst;
- resorption (absorption) of the roots of teeth located next to the impacted tooth and constantly compressed by it;
- the onset of inflammation of the periosteum (flux);
- emerging gingivitis, pericoronitis, abscess;
- periostitis, osteomyelitis of the jaw bone and surrounding soft tissue;
- problems with the functional muscles of the face, violation of its aesthetics, difficulty opening the mouth, speech impairment;
- bad breath;
- painful, uncomfortable condition when chewing, inflammation of the mandibular nerve;
- disturbance of taste sensations;
- headaches, trigeminal neuralgia;
- Body temperature may rise and weakness may occur.
Principles of treatment: is it possible to avoid surgery?
Many patients are sure that an impacted dystopic tooth is necessarily a reason for surgical intervention. But dentists try not to cut without a good reason. Therefore, if your extra teeth are not inflamed and do not interfere with your life, it is quite possible to avoid surgery. The doctor may also prescribe the installation of hard metal braces, which will “pull” the partially erupted tooth from the gum tissue and fit it into the dentition.
Typically treatment proceeds as follows:
- A diagnosis is carried out, which includes a visual examination and the creation of a panoramic image of the jaw.
- The doctor examines the results and decides whether the tooth needs to be removed. If yes, then surgery is prescribed.
- If the dentist sees other ways to solve the problem, he prefers them. First of all, the installation of a bracket system is considered. To do this, it is necessary that there is a place in the dentition where a new element could be placed.
- If braces are not required or cannot yet be placed, the doctor will try to help the tooth erupt. For this purpose, medications and surgery are used. Teething assistance is often used when the wisdom tooth is partially left under the gum, but is positioned correctly.
Modern doctors have many treatment methods in their arsenal, but everything completely depends on the specific case.
Stages of treatment for an impacted tooth
What is a dystopic tooth?
Dystopic tooth
- abnormally erupted tooth. In the jaw it is not located in its proper place, the angle of landing is not physiological. It creates difficulties for the correct positioning of the rest of its brethren.
A dystopic tooth in the jaw develops pathologically, grows in several directions, dystopia occurs: with a deviation to the side - vestibular, tortoposition - the tooth rotates around an axis, with a position pressed into the jaw or extended out of it - distal and medial. In this case, the inclination of the dentition changes pathologically, as does the bite.
Wisdom teeth are characterized by the simultaneous development of two pathologies. The teeth are not only positioned incorrectly: at an angle, but it is also difficult for them to erupt; it happens that they erupt only a little, causing pain to the gums and neighboring teeth. Impacted and dystopic wisdom teeth must be removed. If there is no danger to neighboring teeth, there is no displacement of teeth, there is no discomfort during chewing or sleep, then doctors may decide not to do anything with the tooth.
Canine teeth can also suffer from two abnormalities at the same time, especially if this is caused by supernumerary teeth. If eruption occurs outside the dental arch with displacement, removal is indicated here if orthodontic structures do not help.
The causes of dystopia are:
- Large crown sizes of teeth, especially those that do not erupt completely.
- Supernumerary teeth for which there is no room in the jaw.
- Traumatization of the jaw area.
- Hand chewing, thumb sucking or pacifier sucking.
When is it necessary to remove an impacted tooth? Why remove impacted teeth?
Even an experienced surgeon will say that removing an impacted dystopic tooth is a serious and complex operation that should not be performed unnecessarily. Therefore, it is indicated in the following cases:
- inflammation of the soft tissues (pericoronitis) or jaw (osteomyelitis);
- the tooth is located in a follicular cyst or grows horizontally;
- a cyst or benign formation is diagnosed;
- pus or bacterial infection is detected.
Removal technique
Removal should be carried out by an experienced doctor who knows the specifics of working with impacted teeth. The main problem here is their inconvenient location, so it’s difficult for a beginner to cope with the problem. Removal takes place in several stages:
- Performing local anesthesia (in case of complex tooth position, general anesthesia can be used).
- An incision in the mucous membrane.
- Drilling into bone tissue to create a hole.
- Tooth extraction.
- Removal of tooth or bone fragments.
- Treatment of the wound.
- Stitching.
- Sutures are removed one week after surgery.
Often, the doctor has to first crush and then remove the tooth so as not to damage the adjacent molars and mucous membrane.
Contraindications
The operation will have to be postponed for the following reasons:
- the patient's serious condition due to any kind of illness;
- hypertensive crisis;
- nervous problems or mental disorders;
- viral infections;
- blood diseases;
- serious heart problems.
For women, this operation is not performed 2-3 days before the start of menstruation and after an abortion (at least 2 weeks must pass).
What complications occur after removal of impacted teeth? How to avoid them
Any operation can cause complications, and surgical treatment of an impacted tooth is no exception. Most often, the consequences manifest themselves as severe bleeding, pain, swelling of the gums or cheeks. If nerves are affected, increased sensitivity or insensitivity of the mouth and face may occur. Due to the incorrect actions of doctors, the patient faces a dislocation of the jaw or even a fracture.
The patient can avoid problems after surgery if he goes to a trusted clinic (excluding the human factor) and carefully takes care of the wound that appears in the mouth. Immediately after surgery, the patient should:
- refuse food for 3-4 hours;
- do not smoke for at least 3 hours;
- Avoid alcohol until the stitches are removed.
It is important to come back for a follow-up appointment with a surgeon or therapist. It is necessary to monitor the bleeding: if it does not stop for too long or painkillers do not work, you should contact the dentist immediately. Timely help will help avoid unpleasant consequences.
Postoperative care after removal of an impacted tooth
The doctor is obliged to advise the patient on how to properly care for the wound on the gum. Since removing an impacted tooth is a full-fledged operation, it is imperative to follow the rules of care. The patient needs:
- reduce physical activity to a minimum for 2-3 days after surgery;
- refuse hot and cold foods and liquids;
- change your toothbrush to a soft one;
- take only a warm shower or bath, do not visit baths and saunas;
- take all medications prescribed by your doctor (antibacterial therapy is usually prescribed).
It is important not to rinse your mouth so as not to disrupt the healing. You can make neat baths (liquid or herbal decoction is taken into the mouth, held without rinsing and spitting), but coordinate all procedures with your doctor.
Indications and contraindications for surgery
Indications
Surgery is necessary if the wisdom tooth:
- Dystopic (the direction of growth is changed towards adjacent teeth, tongue or cheek)
- Impacted (not fully or not fully erupted)
- Has roots that are too long (this may initiate their penetration into the maxillary sinus or fusion with the jaw)
- Caused inflammation of the “hood” of the gums or periodontal tissue (pericoronitis)
- Caused the formation of a follicular cyst, phlegmon, gumboil or fistula
- Destroyed due to the development of caries or other dental disease
- Caused inflammation of the trigeminal nerve
- Became a source of permanent injury to the oral mucosa
- Interferes with the eruption of other molars with a narrow jaw
Absolute contraindications:
- Malignant tumor in the root zone
- Hemangioma (benign formation)
- Serious chronic cardiovascular problems
Relative (temporary) prohibitions:
- Infectious diseases, including those of the oral mucosa
- Having had a heart attack or stroke
- Taking anticoagulants
- Exacerbation of psychoneurological diseases
- Pregnancy and breastfeeding (except for emergency indications)
Conservative methods of treating retention
If the tooth is located correctly in the gum and there is minimal interference with eruption, doctors try not to remove it, but to return it to its intended place by nature. Different methods are used for this:
- laser correction;
- current pulses;
- gum massage;
- electrophoresis;
- some medicines.
All these treatment methods are aimed at making the tooth crown get rid of the gum hood on its own. They partially imitate the natural process of eruption of canines and molars. But the availability of such treatment depends on the situation.
Preparing for dental surgery
If a patient is faced with the removal of a complex tooth, then an experienced doctor will not perform such manipulations without prior preparation. An x-ray is required before the operation. This is necessary to clarify the location of the tooth in the bone, as well as to evaluate the tissues surrounding it.
When a patient has an inflammatory process, it is first cured by taking antibiotics.
Complications after pulling out problem teeth rarely occur, but to avoid them, the procedure should be trusted to a highly qualified doctor.
How to stimulate tooth eruption
Stimulating the eruption of an impacted tooth is also one of the ways to treat the problem. The doctor prescribes specialized procedures if he sees that a molar or canine is positioned correctly, but its roots have not yet formed. Then the orthodontist recommends:
- Carrying out vacuum massage with special equipment;
- light finger massage at the site of eruption;
- electrical stimulation;
- exposure to ultrasound, laser, vibrating vacuum devices, etc.
Such methods are aimed at restoring blood circulation and accelerating metabolic processes in the gums.
Extraction for acute and chronic inflammation
Quite often, the removal of a problematic tooth is accompanied by the presence of purulent foci, gum inflammation or periodontitis. In such cases, the doctor prescribes intensive therapy with the use of antibacterial drugs, and only after the inflammatory process has been suppressed is surgery to remove the tooth performed.
There are also situations when a tooth needs to be removed urgently. Only an experienced, highly qualified doctor can perform surgery in such cases.
Conclusions. Expert advice
An impacted tooth is a molar, premolar or incisor that is hidden in bone or gum tissue. If part of the tooth is visible, it is called semi-impacted. Many children and about 40% of adults face this problem when they lose their eights. The appearance of incorrectly positioned teeth itself may go unnoticed – the symptoms are associated with related diseases. Thus, caries in a tooth hidden in the gum almost always causes inflammation of nearby tissues.
It is believed that impacted dystopic teeth are a hereditary problem. But they can appear due to an incorrect bite. Retention can be improved using surgical intervention or conservative methods: massage, electrophoresis, etc. Some dentists recommend wearing trainers, which help develop the dental arch and reduce the risk of improper eruption.
Almost always, the orthodontist tries to return the tooth to the dentition using braces and other methods of influence. If this does not work, the doctor removes the foreign element. The operation is complex, so it is important to contact a specialist. Success largely depends not only on the doctor, but also on the patient: failure to comply with the rules of postoperative care leads to complications.
What to do if you suspect you have a similar problem? See a doctor and be constantly monitored by him. The dentist will prescribe treatment and help prevent complications.
Therapeutic tactics for a dystopic tooth
Removal of a dystopic tooth
occurs if the patient is over 16 years old and the tooth is significantly curved, and there is not enough space in the jaw for its location. If the defect cannot be corrected with orthodontic treatment, then the only option is to remove the tooth. Or it will gradually destroy the roots that are growing directly and cause inflammation of the gums. If other methods have failed, only then is a decision made to remove the tooth.
Dystopic teeth respond well to treatment if the patient is 16 years of age. Prevention of the occurrence of dystopia begins at the time of pregnancy, when the mother eats calcium, and after birth feeds milk, and does not give the pacifier too long. Children and adults should be checked by a dentist regularly to prevent dystopia.
The dentist's goal is to try to preserve the organ, if possible, and create a straight smile line. If saving treatment does not seem feasible, only then will removal be resorted to. For long-term results, it is important to understand how advisable it is to leave dystopic and impacted teeth in the jaw.
If the removal brings correction of the bite and straight teeth, then it will be motivated from the point of view of aesthetics and functionality. If the patient is not bothered by the eights, if they erupted a little crookedly, but do not affect the overall appearance and ability to chew food, then they can not be removed, but a full set of teeth can be left.
Indications for removal:
- Caries, pulpitis, periodontitis. A tooth with difficult access for complete treatment.
- Constant trauma to soft tissues in the area of bite closure.
- The jaw is smaller than the teeth, so there is not enough space for them.
- If the roots of healthy teeth are reabsorbed.
- The aesthetic appearance of the patient is disrupted.
- They interfere with the installation of implants or prosthetics.
- Painful sensations when chewing.
Contraindications for removal are:
- Pregnancy.
- Diabetes.
- Hypertension
- Blood diseases