Ameloblastoma is a type of tumor that appears in the human oral cavity. This disease affects the lower jaw in 80% of cases. It can occur in adults under the age of 60. Ameloblastoma can also be found in adolescents and children.
There are two types of ameloblastoma:
- cystic
- solid (massive)
Massive ameloblastoma is characterized by the presence of spongy tissue at the site of disease. A distinctive feature of cystic ameloblastoma are partially connected or separate cysts that have a thin epithelial membrane on the inside.
Methods of treating the disease
Ameloblastoma is a benign odontogenic neoplasm, diagnosed in a significant number of patients. As a rule, the pathology develops between the ages of 20 and 50, occurring equally often in men and women. In some cases, the disease is detected in childhood and adolescence, accounting for about 6% of all benign jaw tumors. In approximately 80-83% of patients, the neoplasm affects the lower jaw, most often localizing in the area of its angle, much less often developing in the bone of the upper jaw. According to statistical studies, in most cases, ameloblastoma is detected in the initial stages of development, within about six months from the moment of occurrence. Often this pathology is detected by chance, during x-rays performed due to another dental disease. Some patients turn to the dentist with this problem when the disease has lasted for more than a year and the tumor has managed to affect a large area of the jaw. Recurrence of ameloblastoma is diagnosed quite often, in some cases developing years after surgical treatment. and when the pathological process is neglected, its course is unfavorable and there is no adequate therapy, there is a possibility of malignant degeneration (malignancy) of the tumor. Conducting in-depth studies of the disease allowed specialists to put forward several hypotheses related to the causes of its occurrence. It is assumed that the stimulating factors are disturbances in tooth formation and injuries of various types, but to date the reasons for the development of the disease have not been fully elucidated. Ameloblastoma develops very slowly, without causing discomfort to the patient for a long time. As the disease progresses, jaw deformation appears: facial asymmetry and swelling in the affected area become noticeable. It is typical that the degree of asymmetry varies from barely noticeable to pronounced. The symptoms of ameloblastoma of the upper jaw, which is much less common, visually appear even weaker, which is explained by the spread of the tumor process into the maxillary sinus. The occurrence of pain indicates the involvement of bone tissue in the pathological process, and patients often mistake this pain for dental pain. From this moment, displacement and loosening of the teeth begin to develop, and the thinning of the jaw bone with further progression of the disease manifests itself in a characteristic crunching sound. The development of maxillary ameloblastoma poses an even greater threat, since the tumor is likely to spread into the nasal cavity and orbit. At advanced stages of the pathology, the patient complains of intense pain, fistulas develop in the oral cavity, from which purulent exudate is released. Treatment of ameloblastoma involves surgical removal of the affected area of the jaw within the boundaries of unchanged tissue. The extent of the operation is influenced by the size, location and stage of development of the tumor. Since ameloblastoma in most cases is diagnosed at an early stage, the neoplasm does not have time to reach significant sizes. Such patients do not require resection or partial removal of the jaw; surgical intervention is not accompanied by disruption of the continuity of the jaw bone and the formation of cosmetic defects, and is often performed with preservation of functions. After removal of the tumor, in order to prevent recurrence, the resulting cavity is treated with a high concentration phenol solution, as a result of which the pathologically altered epithelial cells become necrotic. If a large ameloblastoma is detected, resection of the jawbone or partial removal of the jaw is indicated. If a focus of purulent inflammation develops, in parallel with the removal of the tumor, its surgical removal is carried out. Before the procedure, which is performed under general anesthesia or local anesthesia, the oral cavity must be sanitized. During the postoperative recovery period, the patient is prescribed courses of antibiotics and symptomatic drug therapy. Coarse and hard foods and dishes that require thorough chewing are excluded from the patient’s diet. After each meal, the patient must rinse the cavity formed after the operation. In the case of removal of a significant portion of the jaw bone to restore lost functions and eliminate cosmetic defects, bone grafting surgery using individually made orthopedic structures is indicated.
Recurrent ameloblastoma: a clinical case
Ameloblastoma is a common, localized, aggressive, benign odontogenic tumor of the oral cavity of epithelial origin. This pathology was first described by Cusack in 1827, and its name was given to Ivy and Churchill in 1930.
According to the 2005 WHO classification, there are 4 subtypes of benign ameloblastoma: (1) solid/multycyst, (2) desmoplastic, (3) unicyst, and (4) extraosseous/peripheral. Histologically, 6 tumor subtypes can be differentiated, including follicular, plexiform, acanthomatous, basal, unicyst and desmoplastic. Treatment is carried out either conservatively or radically, depending on the type, location and size of the lesion, as well as taking into account the age of the patient. A systematic review by Almaida and colleagues found that 50% of tumor recurrences are observed in the follicular subtype, and the incidence of such development is reduced when a radical treatment algorithm is implemented. This article describes two cases of recurrent ameloblastoma in patients who underwent segmental resection of the jaw.
Clinical case 1
A 46-year-old patient sought help at a private dental clinic with complaints of swelling in the area of preliminary surgery, covering the area of the lower jaw on the right. According to the medical documentation, it was established that about 15 years ago the patient underwent a segmental resection of the jaw with further augmentation of the formed defect with an augmentation from the region of the ribs. No data on the histopathological characteristics of the lesion were noted in the patient's medical record. After a CT scan and orthopantomography, a multilocular radiolucent lesion was discovered in the area of the previous surgical intervention (photo 1).
Figure 1: 3-dimensional reconstruction of a CT scan demonstrating recurrent tumor in the area of the augmentation involving the articular process.
Clinically, a diagnosis of recurrent multicystic ameloblastoma with involvement of the bone augmentation was made. An incision in the tumor area was made at a distance of 1 mm from the edge of soft tissues unaffected by pathology through the scar contour already existing from the preliminary operation (photo 2-3). The specimen collected for histology allowed a diagnosis of follicular ameloblastoma with acanthomatous changes and free margins. 1 year after surgery there were no signs of relapse. Therefore, alloplastic reconstruction of the mandible on the right side was planned, given the benign nature of the tumor.
Photo 2: View of the exposed tumor during surgery.
Photo 3: Surgical specimen.
Clinical case 2
A 45-year-old patient sought help from the Department of Oral and Maxillofacial Surgery with complaints of swelling in the right temporal region. The swelling did not provoke pain and developed over the course of a month, increasing in size. There were no signs of infection in the affected area. In 2012, the patient already approached a private dental clinic with a similar problem. An orthopantomogram and CT scans revealed a multicystic lesion. After a biopsy, it became clear that the problematic tumor was an ameloblastoma. The patient underwent a hemimandibulectomy procedure. Directly during surgery, radiography of the surgical tumor specimen was taken to analyze the condition of the tissues at a distance of 1.5 cm from the clinically visualized tumor edge. Histological analysis confirmed the diagnosis of ameloblastoma with atypical features and multicellular structure. In 2016, the patient again had swelling in the right temporal region. MRI identified heterogeneous signal enhancement in this area measuring 4.4 cm × 3.7 cm × 4.6 cm with the presence of tiny cystic inclusions (Figure 4). Through access along the zygomatic bone, the tumor was removed with a certain amount of surrounding tissue (photo 5-6). The formed defect was restored using the temporal muscle. After histoanalysis of the surgical tissue sample, the diagnosis of ameloblastoma with non-invasive margins was confirmed. At this time, the patient is at the monitoring stage.
Photo 4: Preoperative CT scan showing recurrent ameloblastoma in the infratemporal fossa.
Photo 5: Visualization of the bone defect after tumor removal, which was then reconstructed using the temporalis muscle.
Photo 6: Excised tissue sample.
Discussion
Ameloblastoma is a locally aggressive tumor of the oral cavity that rarely undergoes malignant transformation. After odontoma, it is the second most common odontogenic tumor. According to epidemiological data, 70% of cases of ameloblastoma were reported in developed countries. The problem of low identification of ameloblastoma in developing countries is obviously associated with the insufficient level of their official registration. The WHO classified ameloblastoma into four subtypes in 2005: multicystic/solid, unicyst, desmoplastic, and extraosseous. Solid/multycystic ameloblastoma is the most common type, which is also the most aggressive and often recurs after conservative treatment such as curettage or enucleation. Ameloblastomas of the lower jaw recur much more often than their counterparts in the upper jaw. Also, the follicular type of tumor is characterized by a higher rate of relapse compared to its plexiform subtype. The pathogenesis of ameloblastoma development remains incompletely understood. The genetic theory of development involves the participation in the process of pathogenesis of the BRAF protein in the structure of the mitogen-activated protein kinase pathway (MAPK), which, as a rule, is already identified as mutated.
Ahlem et al found that the activity of the biomarkers Ki67 and CD10 was significantly higher in recurrent tumor types compared to primary tumor types. As a rule, ameloblastoma affects the posterior areas of the lower jaw. Infiltration of the lesion occurs into the cancellous part of the bone with less involvement of the cortical component. The CT scanning method for diagnosing a tumor is the most informative when the cortical structure of the bone is damaged and the damage has spread to the surrounding soft tissue. Treatment of the tumor can be conservative or radical. A conservative approach involves enucleation of the tumor with further chemical cauterization or peripheral osteoectomy with expansion of the excision boundaries by 1-1.5 cm from the visualized edge of the tumor. A conservative treatment approach is more effective in cases of monocystic type of formation. According to Pogrel and Montes, unicystic ameloblastomas respond best to conservative treatment using Carnoy or cryotherapy principles. A radical approach is indicated in cases of large ameloblastomas when the lesion has spread to the area of the inferior alveolar nerve, or in cases of the aggressive nature of the tumor. The radical treatment method involves performing marginal or segmental resection with removal of adjacent bone tissue 1.5-2 cm from the visualized edge of the tumor. To confirm that the tumor has spread to adjacent tissues, it is recommended to carry out control radiography directly during surgery. In cases of ameloblastic carcinoma, excision of bone tissue is recommended at a distance of 2-3 cm from the visualized edge of the tumor. Recurrence of ameloblastoma is most often associated with the histological type of lesion and its location. The solid variant of the neoplasm is the most aggressive. Most often, ameloblastoma occurs in the distal areas of the lower jaw and affects the cancellous component of the bone through the mechanism of invasion, reaching the cortical plate and provoking its perforation. Once the tumor penetrates the periosteum, the risk of its further spread to the surrounding soft tissue increases. Inadequate lesion resection increases the risk of possible recurrence during follow-up. Cases of recurrent ameloblastoma have already been described by Grafft, Carvalho, Dolan, Marinelli, Stea, Zacharides, Vasan, Bianchi, Martins and Favaro, Su, Choi, Basat.
In most of the described relapses, restoration of the defect site after surgery was carried out using an iliac graft. Cases of recurrent ameloblastoma after radical treatment were described in studies by Sehdev, Shatkin and Hoffmeister, Mehlisch, Muller and Slootweg, Olaitan, Ueno, Eckhardt, Nakamura. It is known that the relapse rate with conservative treatment is significantly higher (60%) than with radical treatment (13%). The risk of relapse during surgical excision of ameloblastoma may be associated with retention of epithelial conglomerates of the neoplasm in the structure of the surrounding soft tissue. In the first clinical case described, the augmentation tissue succumbed to tumorigenesis, apparently due to the remaining tumor cells in the area of the osteoectomy. Therefore, before starting reconstruction of solid ameloblastomas, it is recommended to monitor the cleanliness of the edges of the excised tissues using control radiography. It is even better to wait for the results of a histological analysis of a tissue sample taken during the operation. Tumors in the infratemporal fossa are usually asymptomatic, and the main complaint of patients remains only signs of swelling and facial deformation. The infratemporal fossa is a pyramid-shaped structure that is located on the lateral surface of the base of the skull, deeper than the temporal arch, masseter muscle and ramus of the mandible. The medial part of the ramus of the mandible and the floor of the skull form the upper surface of the pyramid-shaped structure. The anteromedial part of the infratemporal fossa corresponds to the posterior surface of the upper jaw, and the posteroinferior part is formed by the pterygoid fascia. In fact, the infratemporal fossa is anatomically inaccessible, so it is almost impossible to monitor neoplastic growth in its structure.
Diagnosis and treatment planning for ameloblastomas localized in the infratemporal fossa should include the use of CT and MRI methods, which make it possible to establish an objective level of tumor spread. Conventional radiography in such cases is not sufficiently informative. Access to the infratemporal fossa can be formed transorally, transnasally, transpalatally, through the zygomatic bone, transcervically, and even through an extended maxillary approach. The approach through the zygomatic bone area is one of the most suitable for both resection of neoplasia and the formation of a temporal flap. The choice of surgical approach depends on the tumor type, clinical features, histological subtype, extent of spread and location.
In the second clinical case, relapse may be associated with preservation of the periosteum during a previously performed operation. It is in the periosteum that conglomerates of neoplastic cells could and will remain. A more extensive resection allows you to remove all tissue that has succumbed to neoplastic invasion, and thus minimize the risk of relapse. Carlson and Marx described the need to remove all anatomical structures adjacent to the tumor area for prophylactic purposes. This approach is reasonable when tumor invasion into surrounding soft and hard tissues is confirmed, since cases of recurrent ameloblastomas have been reported even 30 years after initial removal of the lesion. Laborde and Becelli described that in the cases of 7 patients, there was no evidence of tumor recurrence after treatment, and doctors used an approach with extensive excision of surrounding tissue.
Similar reports were also provided by Vayvada, Chaine and Basat. Vaishampayan suggested that recurrence of ameloblastoma after excision from the infratemporal fossa is associated with retention of the weakened process of the mandible after segmental resection procedures. Peacock et al concluded that the completeness of tumor excision can be verified not only by histological examination, but also by plain radiography. Although several publications indicate the resistance of ameloblastomas to brachytherapy, irradiation of recurrent types of lesions with high doses of 110 Gy was characterized by a fairly successful result.
During treatment for ameloblastoma, we recommend adhering to the following recommendations:
- In order to control the degree of invasion of large ameloblastomas into the surrounding soft tissue, it is necessary to use the MRI method.
- To control the completeness of excision of neoplastic tissue during surgery, it is necessary to use control radiography.
- Tumor resection margins should be widened to minimize the risk of future tumor recurrence.
- After confirming the cleanliness of the working field, it is necessary to carry out surgical reconstruction of the bone defect formed after tumor removal.
- Monitoring the area of preliminary localization of ameloblastomas after their resection is mandatory and should include the use of CT and MRI control.
conclusions
Based on the analysis of two clinical cases, we can summarize that the solid type of ameloblastoma is extremely aggressive and is characterized by a high rate of relapse. During treatment, it is necessary to take into account the risk of tumor invasion into the surrounding soft tissue, as well as the fact that the tumor, as it progresses, can provoke erosion of the cortical ball of the mandible. To gain a deeper understanding of the nature of the development of ameloblastomas, it is necessary to conduct a number of additional clinical and histological studies.
Authors: Chithra Aramanadka, Abhay Taranath Kamath, Adarsh Kudva (India)
How is the disease diagnosed?
Examination of a patient, diagnosis and development of a treatment regimen takes about three days in Israeli clinics.
- Day 1
- Day 2
- Day 3
On the first day of stay at the medical center, the patient undergoes a consultation with a leading dentist.
At the appointment, the doctor gets acquainted with the medical history, clarifies the symptoms that are bothering the patient, and conducts an examination of the oral cavity. At the final stage of the consultation, the specialist prescribes the required examinations. The next day, the types of diagnostic procedures indicated in the list of appointments are performed:
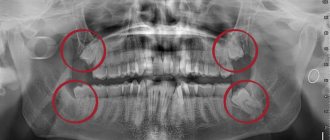
- X-ray examination (general X-ray of the upper and lower jaw,
- lateral projection, axial radiography);
— computed tomography (CT);
— puncture of the tumor followed by laboratory cytological analysis of the obtained material (the most informative method of diagnosis).
The research results are reviewed by a medical commission, which includes a dentist and highly specialized specialists. Doctors collectively make a diagnosis and build a treatment plan.
Symptoms
Ameloblastoma is one of the most common forms of odontogenic tumors in dental practice. In 80% of cases, the lower jaw is affected. Ameloblastoma rarely occurs in childhood or adolescence; there are no statistical differences by gender (occurs equally often).
Relapses of ameloblastoma are quite frequent, and in cases of advanced pathology and predisposition to cancer, the formation can become malignant.
The development of a tumor to visible size takes from a year to several years, and at first it is asymptomatic. Then they appear sequentially:
- Asymmetrical face. In most cases, the tumor is accompanied by changes in proportions and facial features, however, with a tumor of the upper jaw, the violation of symmetry is not so pronounced, so it can go unnoticed.
- Periodic pain in the jaw area (often mistaken for toothache), in some cases persistent and constant.
- Loose teeth, displacement of part of the dentition, malocclusion. Massive tooth loss may begin.
- Changes in the skin. This symptom is not observed in all patients; most often it accompanies an inflammatory process complicating ameloblastoma.
- Visible deformations of the maxillofacial structures. With severe changes, speech and chewing function are impaired.
Advantages of treatment in Israel
- High level of qualifications and extensive experience of doctors.
- Availability of modern diagnostic and treatment equipment.
- Quickly and accurately diagnose.
- Application of modern methods of therapy.
- Reasonable prices.
The success of therapy and the least number of complications directly depend on the implementation of a treatment course at an early stage of the disease. Don’t waste time, contact your chosen Israeli clinic and start treatment as soon as possible.
- 5
- 4
- 3
- 2
- 1
(0 votes, average: 5 out of 5)