December 3, 2020
Contact dermatitis is an inflammation of the skin in an area that has come into contact with an irritating substance or environmental factor. Children under 12 years of age are most susceptible to the disease. The point is the structural features of children's skin and the weakness of its protective mechanisms. The disease manifests itself in any area that has been in contact with the irritant, but more often on the face, arms, neck, and groin area.
If the provoking agent is recognized in time and the child is protected from it, the inflammation is well treated and the symptoms quickly pass. When the cause is difficult to identify or parents do not consult a doctor on time, the course of the disease becomes more severe.
Contact dermatitis occurs:
- simple - local irritation by some factor;
- allergic.
The second option will appear when the child has an increased sensitivity to this substance. The first interaction with it is outwardly unnoticeable, but chemicals are formed in the skin that bind to immune cells - T-lymphocytes. Immune cells remember the stimulus. Upon repeated contact, which can occur after a long time, T-lymphocytes trigger an allergic reaction and cause skin symptoms.
How to recognize allergic contact dermatitis in a child
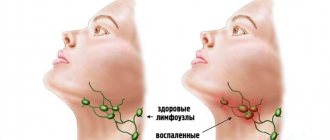
The contours of the inflammation often coincide with the outlines of the object that caused the irritation. The rash spreads little beyond the area of skin that came into contact with the causative factor. The skin here becomes red and swollen, very itchy, blisters, wounds and crusts appear.
Fungal and bacterial infections easily attach to wounds and suppuration occurs. Babies may experience an increase in general temperature.
Frequent exacerbation in the same places leads to unpleasant outcomes: areas of increased or decreased pigmentation, scars, thickening and roughening of the skin.
If you notice a rash or red spots on your child’s skin, be sure to see a doctor to get tests done to determine the exact cause and begin treatment.
The disease may worsen. To prevent this from happening, you need to find and eliminate the provoking causes.
Soon after the birth of a child, parents may notice a formation on the skin of blue, red, pink color, which can quickly grow, capturing new territories on the baby’s tiny body. Most likely, this is a benign vascular tumor, a hemangioma, with all the inherent signs of a benign tumor.
A feature of the course of vascular neoplasms - hemangiomas in young children is the unpredictability of their “behavior”. A punctate hemangioma of the cheek in a one-month-old baby can turn into an extensive and deep tumor with a complex anatomical localization and without a tendency to stop growth within 2-3 weeks. This leads to disruption of the functions of various important organs responsible for vision, hearing, breathing, etc. Due to the unpredictability of the development of hemangiomas in children under one year of age, hoping for independent resorption of large and deep hemangiomas using expectant management means voluntarily taking a conscious risk of the health and life of the baby. It is necessary to distinguish between a vascular tumor and other formations: medial spot, nevi Unna, rosacea, etc.
Therefore, if you find any spots, spots, or blood vessels on the baby’s body, immediately contact pediatric surgeons and oncologists.
Why does hemangioma appear?
It is believed that a tumor as a disease occurs as a result of the body’s reaction to harmful external and internal influences. Therefore, to prevent vascular tumors during pregnancy, simple rules must be followed: contact with harmful carcinogenic substances should be completely avoided; You should not smoke, you should not be in a room where people smoke or have smoked; Uncontrolled use of any medications is strictly prohibited. There is an opinion that the appearance of hemangiomas is associated with complex disorders of intrauterine development of the fetus, especially in the first trimester of pregnancy, when the vascular system of the unborn baby is formed. During this period, emotional and chemical stress, low-frequency electromagnetic influences, injuries, infections, hormonal disorders and any unfavorable factors of a physical or chemical nature that have embryotoxic properties are especially dangerous. Particularly dangerous factors of a physical nature include ultraviolet radiation (solariums!), ionizing radiation, mechanical injuries and elevated temperature in a pregnant woman with long-term exposure. Among the biological factors include viral and bacterial diseases, decreased immunity, and parasitic infections of the mother during pregnancy. Sometimes it is enough to dye your hair in the early stages of pregnancy and the child develops a “stork’s kiss,” as hemangiomas are often called.
Experts are still debating whether hemangiomas are true tumors or a congenital malformation of the vascular system. These tumors have the ability to self-resorb and malignant degeneration. Nowadays, hemangiomas occur in every tenth newborn. In girls it is 2-3 times more common than in boys. If a child already has one hemangioma, then during the first six months of life, 75% of such children may develop hemangiomas in other parts of the body. Recently, the number of children with multiple hemangiomas has increased to 43%. Hemangiomas can grow unevenly. Along with rapid growth, often leading to severe irreversible damage, sometimes there is a complete lack of growth, and in some rare cases even reverse development.
What complications can occur with hemangiomas?
The vast majority of hemangiomas do not have complications. However, in some cases, ulcers and ulcerations occur on them; some hemangiomas are complicated by bleeding. A feature of the course of hemangiomas in the perineum and external genitalia is their tendency to frequent ulceration. Contamination of these areas with urine and feces, friction with diapers or clothing can lead to the formation of ulcers, drip bleeding, and infection. In cases of internal hemangiomas, for example, the larynx or the inside of the nasal passage, the breathing process is complicated. Vascular tumors of the eye can cause occlusion and amblyopia. Hemangiomas of the oral mucosa and lip area disrupt the processes of sucking and digestion. With very large tumors, cardiac dysfunction may occur due to the large amount of blood that must be pumped into the excess blood vessels of the hemangioma. Angiomas adjacent to the bone can also lead to bone erosion. Children with hemangiomas may develop thrombocytopenia due to the death of platelets in the vascular tumor. There are gigantic hemangiomas of skeletal muscles, consisting of thin-walled capillaries infiltrating the entire limb.
How to assess the condition of hemangioma in a child yourself?
Signs of growth, stabilization and regression:
1.Color - a fast-growing tumor is bright red, tense, bulging, the surface is shiny or peeling
2.rapid increase in tumor size: dynamic measurement of the tumor is necessary. You can transfer the contours to cellophane and get a stencil that reflects its size and area. Mark on the stencil the date and overall height of the child at the time of measuring the tumor or the length and circumference of the body part at the measurement site. After 3-4 weeks, take a repeat measurement to create a repeat stencil, observing the same position of the child’s body (standing, lying, sitting). Re-enter the date and information about the child’s height. The assessment is carried out by simple mathematical comparison. If the increase in the size of the hemangioma area in millimeters is equal to or exceeds in digital value the number of centimeters by which the child has grown, then this is an indicator of the progressive development of the neoplasm itself. Such a growing hemangioma requires immediate treatment.
A sign of stabilization of growth or the beginning of regression is its pallor, a decrease in volume, the appearance of areas of whitish coloring in the mass of the tumor - a symptom of “fly agaric”.
If there is a hemangioma, in the interests of the child, taking into account the unpredictability of its development, it is necessary to carry out therapeutic or preventive measures, and the sooner the better.
What treatment methods for hemangiomas exist?
Currently, more than 60 methods of treating hemangiomas are known: surgical, sclerosing, electrocoagulation, radiation, hormonal, laser, cryogenic, medicinal, etc. Each of the methods has certain advantages and disadvantages, and the question is which one is the most rational with in terms of simplicity, accessibility, convenience for the patient, effectiveness in terms of cosmetic and functional results. The choice of treatment method should be based on a comprehensive assessment of each case, taking into account the type, location, clinical form, size, nature of the hemangioma, and the age of the patient. Conservative and invasive methods are used to treat hemangiomas. Of the conservative methods, the most commonly used are hormone therapy, treatment with propranolol, radiation methods, and photochromotherapy. Among the invasive methods, the most popular are surgical excision, cryotherapy (cold treatment), electrocoagulation, laser therapy, sclerotherapy, and embolization of regional vessels. Unfortunately, each of these methods does not provide a guaranteed cure, but has a number of side effects. At the Oncology Research Institute in Rostov-on-Don, a non-invasive, painless method of treating hemangiomas in children was developed and patented: photochromotherapy (a treatment method in which a certain modified red light). This medical technology is protected by Russian Patent No. 2240159 for the invention “Method for treating skin tumors in children under one year of age” and has been widely and successfully used for more than 10 years.
Photochromotherapy - the use of the method is based on the ability of monochrome red light to induce photobioadaptive processes in the child’s body, leading to the activation of humoral factors regulating local blood flow and induction of reparative tissue reactions, which contributes to the stabilization of growth and regression of vascular neoplasms of the skin. This technique is non-invasive and allows it to be used for both therapeutic and preventive purposes. The developed method for treating skin tumors is suitable for children of any age - both up to one year of age and older.
Contraindications:
individual intolerance to light therapy, severe neurological symptoms, acute infectious diseases of unknown origin. Considering the simplicity, harmlessness, painlessness and high efficiency of this method, it can be actively recommended for the treatment of hemangiomas in children.
Errors in the treatment of hemangiomas
The traditional mistake is to wait and see
in the hope of spontaneous resorption. It is not possible to hope for spontaneous regression of large and deep hemangiomas due to their rapid growth or other complications.
Another common mistake is prescribing troxevasin
to the area of hemangiomas. Monitoring of children after the administration of troxevasin in the early stages showed stimulation of tumor growth in 98% of children. This also applies to Lyoton and other heparin-containing drugs. One of the erroneous prescriptions is to apply ice; after such an effect, a phase of sharp vasodilation begins, and the hemangioma grows. There is no point in using Vishnevsky's liniment, and the use of decoctions of St. John's wort, primrose, oats, bee products, acetic and sulfuric acids can significantly worsen the process, lead to dangerous bleeding and tumor growth. The obvious harm is lost time, a neglected process.
What should children with hemangiomas be wary of?
1. Injuries . Danger of bleeding in case of injury - call an ambulance if there is bleeding. It is necessary to apply a hemostatic sponge and press firmly. Cold compress - ice cubes, preferably made from a decoction of oak bark, but you can keep it for no more than 10-15 minutes, then remove it for 15 minutes and repeat the procedure. Hydrogen peroxide 1-2% and antiseptic disinfectants (miramistin or chlorhexidine) are used.
2. Sun. _ You should be wary of direct sunlight. You should take a walk in the summer until 10 a.m. and from 6 p.m. From 11 a.m. to 5 p.m., direct sunlight causes irreparable damage to the skin. Before a walk in the sun, give your baby salted water or tea with lemon. Use sunscreen.
Sunscreens for babies: AVEN: sunscreen for babies spf 50+, Garnier AMBRE SOLER: sunscreen milk-screen baby spf 50, spray, sunscreen color, control for babies, spf30, Vichy Capital Soleil, baby sunscreen spray, spf 50, sunscreen hypoallergenic baby cream, spf 30. La Roche Pose antiheliosdermoKIDs: milk (for babies), spf 50. Mustella sunscreen milk for babies spf 50+, sunscreen spray for children, spf 30. Uriage baby sunscreen milk for hypersensitive skin spf50 spf 30. Floresan, sunscreen milk for babies spf25. Bübchen sunscreen spray for children spf 30, sunscreen milk for children spf 20, sunscreen foam for children spf 15 and 25. Nivea sun sunscreen spray color for children spf 30, children's sunscreen lotion spf 50+. Oriflame children's sunscreen spf 40, spray spf30."Our Mother" Russia children's sunscreen cream spf 15, children's sunscreen mousse with a water-repellent effect, spf 20, children's sunscreen milk spf15."Our Sun", Russia children's sunscreen cream spf 20.1. You need to choose the right protection product: creams are useful for children For those with dry skin, sprays are most convenient.2. Check safety: apply the cream behind the ear, on the elbow and knee bends, observe the skin and the child’s reaction to the smell for 24 hours. 3. Apply the product half an hour before going outside. 4. Distribute correctly over the entire surface of the skin - colored sprays are convenient. 5.Storage sunscreen in the refrigerator for a maximum of six months.
3. Bathing . It is not recommended to bathe in hot water up to 37 degrees, do not bathe in a manganese solution, use neutral soap on the hemangioma area once every 10 days.
4. Before recovery, it is not recommended to do routine preventive vaccinations, since the possibility of provoking the rapid growth of hemangiomas in children after vaccination cannot be ruled out.
Photochromotherapy.
This is a type of treatment with visible electromagnetic radiation (light quanta) with a certain wavelength. The clinical use of red light with a wavelength of 0.67 microns allows for a therapeutic effect due to the photolytic breakdown of biomolecules, which leads to the growth of free forms with high biological activity. This medical technology is protected by RF patent No. 2240159 for the invention “Method for treating skin tumors in children under one year of age.” The technique is non-invasive, which allows it to be used in the treatment of early infants with hemangiomas of critical locations (head and neck, genitals, mammary glands, places of natural skin folds, articular surfaces. The high efficiency of the FCT method lies not only in achieving a local therapeutic result (photo-induced regression of the vascular tumor itself), but also in increasing the overall protective and compensatory potential of the child, achieving an immunostimulating and anti-stress effect on his body.
External causes of the development of allergic dermatitis in children
The disease can be caused by one of the factors or a combination of several.
- Physical - friction or pressure on the skin of fabrics, leather products, high or low temperatures, humidity, electric current, ultraviolet or x-rays.
- Chemical - various acids and alkalis, substances included in creams and hygiene products, medicines, tobacco smoke.
- Biological - sap and pollen of plants, bites and secretions of insects and animals.
Of the plant agents, the most dangerous are the juice of celandine, hogweed, nettle, pollen of meadow and weeds.
In industrial cities in winter, there are widespread cases of contact dermatitis under the eyes and on the hands of children. Three factors are combined here: cold, chemical impurities in the air and touching the skin with wet mittens.
In infants, allergic inflammation can be caused by a combination of high humidity in diapers, fabric friction and the action of inappropriate cream.
A special type of contact dermatitis is phototoxic, when sunscreens degrade in sunlight and cause allergic damage to the epidermis.
Dermatitis in a child and psychosomatics
Skin health directly depends on a person’s mental well-being. Stress changes hormonal levels and metabolism, causing disruptions in the functioning of the immune system. Therefore, a calm emotional state will prevent exacerbation of the disease and delay the first appearance of symptoms.
When faced with contact dermatitis, analyze the causes and identify the allergen that caused it.
It's not always easy. To be sure of the correct diagnosis, conduct the necessary tests and receive treatment, come for a consultation at our center. In addition to treatment, you will learn how to properly prevent this disease. December 3, 2020
Author of the article: dermatologist Mak Vladimir Fedorovich
What are the causes of the disease?
It is necessary to distinguish between the cause and triggers of atopic dermatitis.
The reason is not fully known to modern science; the main version is a set of genetic, immune and skin changes, in particular, a deficiency of the skin protein filaggrin, which is responsible for retaining moisture in the skin.
The triggers of atopic dermatitis are very diverse, atopic skin is overly sensitive to irritation, so exacerbation can be caused by increased sweating, heat, rough clothing, detergents, dry air, etc. Children with atopic dermatitis may simultaneously have allergies to food, household or other animals, dust mites, tree and grass pollen - these allergens can also be triggers for exacerbations.
In general, atopic dermatitis has a wave-like course, periods of exacerbations (most often occurring for unobvious reasons or for no reason) are replaced by periods of remission - hence there is a great temptation to associate exacerbations with factors that are not directly related to the disease, and vice versa - to attribute healing properties to completely extraneous factors (for example, a diet that parents started by mistake or out of desperation).
It is impossible not to mention the established harmful domestic tradition of calling atopic dermatitis allergic (usually associating it with an allergy to cow’s milk protein) and treating it with diets (a strict “hypoallergenic” diet for a nursing mother, and/or a hydrolysis/amino acid mixture for a child). Indeed, if a child has an intolerance to cow's milk proteins, it may aggravate or cause atopic dermatitis, but not vice versa. Not every child with atopic dermatitis has an intolerance to cow's milk proteins or any other allergens. This means that by prescribing a diet, or an expensive and unpleasant-tasting mixture, the doctor adds problems to the family without helping them. In most cases of atopic dermatitis, identifying allergies and excluding allergens does not provide any benefit.