One of the most common reasons for patients visiting dental clinics is traumatic damage to teeth and surrounding tissues. At any age, a tooth bruise can occur - a painful injury, which, despite the discomfort, at first looks quite harmless. Subsequently, it often turns out that the pain does not subside, and the bruised tooth begins to react to hot or cold. This usually means that the neurovascular bundle—the dental pulp—is damaged, and a visit to the dental office is necessary.
Even a very careful adult can get a severe bruise to a gum or tooth (for example, by not calculating the movement and hitting himself with a spoon or glass). What can we say about kids who are constantly on the move and often fall, hitting their teeth on various objects. As a result, enamel cracks, root fractures, dislocations and other injuries occur. In the ICD (International Classification of Diseases), chapter 29 is devoted to dental injuries, which describes the consequences of single or multiple mechanical impacts leading to disruption of the integrity of teeth and surrounding tissues.
What it is
One of the most common dental injuries, mostly occurring in childhood, is bruising. Of course, this kind of damage cannot be ruled out in adults, especially those leading an active lifestyle and involved in traumatic sports.
A tooth bruise is a closed injury caused by strong mechanical impact with a hard object. In this case, the integrity of the bone tissue and the anatomical position are not damaged, but the periodontal tissues suffer, sometimes severe rupture occurs, followed by bleeding.
If the blow was so powerful that the neurovascular bundle was damaged, the tooth may become stained or darkened due to hemorrhage into the dentinal tubules and pulp tissue. Occasionally, with a bruise, numbness is one of the accompanying signs, as well as external damage to the facial area in the injured area, as well as the appearance of swelling and bruising. In any case, most often all these damages are reversible and can be treated if you consult a dentist in a timely manner.
The likelihood of tooth loss after injury: what doctors say
Can a tooth fall out after a blow? This situation is rare, but it cannot be excluded if the supporting ligaments and periodontal tissues are severely damaged, and the person does not seek dental care for a long time.
More often, after a blow, the tooth hurts and only wobbles a little, and the gums around it are red and swollen. But even in this case, you cannot relax. According to doctors, against this background traumatic gingivitis and periodontitis can develop. These diseases, with inadequate treatment and careless attitude to oral hygiene, progress and become generalized (spread to the entire range). Advanced periodontitis is also fraught with loosening and loss of moving elements.
Causes
Like any other injury, a tooth bruise can have a wide variety of causes. This could be an accidental hit in the jaw with a ball or other sports equipment, an unfortunate fall, a strong blow in a fight, or the consequence of a road accident or riding a bicycle. All these reasons have one thing in common - a strong blow of a mechanical nature.
Children and athletes are the most vulnerable to such injuries. It is these two categories of patients with a similar diagnosis that are the most frequent visitors to dental clinics. However, household injuries, as a result of which a person accidentally or recklessly hits a tooth, can cause a bruise. In this case, the most unprotected and weakest anterior and lateral incisors on the upper jaw most often suffer due to the anatomical structure and overhang of the upper jaw over the lower jaw.
Complications after injury
Usually bruises do not affect the health of the teeth in any way, but sometimes they lead to complications. Among the most common are a strong change in the color of the enamel against the background of hemorrhage that appears in the pulp chamber. Over time, a damaged tooth may become gray or brown, this is due to a slowdown in metabolic processes occurring in the tissues.
If the pulp dies, a disease such as pulpitis may develop. If you ignore the first symptoms, the risk of developing periodontitis becomes very high. As a result, a post-traumatic odontogenic cyst may appear, which is localized on the upper part of the tooth root.
If a child whose molars have already emerged is injured, the development of the roots of permanent units may be disrupted. If the injury is in a very young patient, it can cause a disruption in the formation of the rudiments of future permanent teeth. In the absence of timely intervention, they may die.
Symptoms
The symptoms accompanying a tooth bruise are easy to recognize. If a person bruises a tooth, it hurts quite noticeably, and over time the pain only intensifies, especially with pressure on the damaged area and chewing food. The following symptoms are also present:
- When the neurovascular connection is ruptured, hemorrhage occurs into the pulp tissue, due to which the enamel quickly turns pink;
- The crown may darken;
- When bruised, the tooth becomes loose, although its mobility is relatively small;
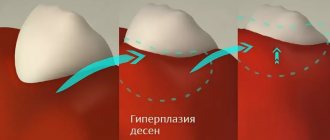
- At the site of impact on the soft tissues of the gums, swelling, hyperemia, deformation of individual areas of the mucous membrane, and the formation of hematomas may occur;
- If there is a very strong impact, ligament rupture, joint damage, or even a fracture of the alveolar process of the jaw may occur where the striking object hits the jaw. In this case, it will be difficult and painful for the patient to open and close the jaw. Such damage can only be diagnosed with an x-ray.
Acute Dental Trauma Classification Terminology Diagnostics
The format of the article does not allow us to present the mentioned classifications in full; we will limit ourselves to only a few comments. The disadvantage of the classification proposed by the Bulgarian authors Sl. Davydov and Z. Peneva (1964), in our opinion, is the inclusion of a section “Traumatic periodontitis” in it, which does not correspond to the generally accepted classification of periodontitis, which distinguishes acute, chronic periodontitis and chronic periodontitis in the acute stage.
The term “traumatic” indicates only the cause of periodontitis, and not its course. The nosological forms introduced by the authors: “Loosening of teeth without dislocation”, “Rupture of the neurovascular bundle without loosening of teeth” are not types of injury, but its consequences.
In the classification developed by V.F. Vasilevskaya (1970), types of crown fractures in the area of enamel and dentin are distinguished based on the transillumination of the pulp, which seems to us rather arbitrary due to the same treatment for this pathology. In our opinion, it is inappropriate to introduce into the “Combined trauma” section simultaneous, but different in form, injuries to two or three teeth of one patient. In addition, the classification does not take into account all types of combined tooth damage.
It is extremely difficult to use in practice the classifications proposed by G. M. Ivashchenko (1963) and A. M. Konstantinov (1985), due to the unsystematic and incomplete listing of nosological forms of injuries. Thus, G. M. Ivashchenko did not include in the working classification the definition of the type and level of the tooth fracture line, which is necessary to know when planning treatment. A. M. Konstantinov uses not a clinical, but a metric assessment of damage - “Fracture of 1/3 or 2/3 crown.”
This is quite difficult to determine due to the different size, shape and location of the broken part; in addition, this information is not decisive when planning treatment. It is unacceptable, in our opinion, to distinguish between “complicated” and “uncomplicated” root fractures, since this involves combining the injury as such with its consequences.
One of the latest is the classification developed by V.V. Roginsky (1987). In our opinion, there is no reason to complicate the classification by indicating the degree of formation of the root of the injured tooth. You should also not include tooth contusion in the classification as a nosological form, since it is impossible to diagnose it on the basis of the signs proposed by the author.
Pulp necrosis, identified by the author (class I-II, type 3), is a consequence of trauma, and not a nosological form.
In our country, the best known classification is N.M. Chuprynina, published in the latest edition in 1993 (Chuprynina N.M., Volozhin A.I., Ginali N.V. Dental trauma, 1993). In this classification, in particular, dislocations with displacement of a tooth towards the adjacent one and rotation of the tooth along the axis are considered separately.
In our opinion, a tooth physically cannot rotate along its axis, much less move towards the adjacent one, without preliminary extrusion, which in this classification is also considered as an independent form of dislocation. In addition, there is the author’s interpretation of the concepts of “combined” and “combined” trauma, which contradicts general medical concepts in this area. And finally, the category “trauma of the germ” is highlighted.
Since the germ is not a full-fledged tooth and cannot be directly injured, consideration of this nosology in the classification of acute dental trauma is unjustified.
The WHO classification is known, which identifies 8 classes of HTA:
- Class 1: Tooth contusion with minor structural damage.
- Class 2. Uncomplicated fracture of the tooth crown.
- Class 3. Complicated fracture of the tooth crown.
- Class 4. Complete fracture of the tooth crown.
- Class 5. Coronal-root longitudinal fracture.
- Class 6. Tooth root fracture.
- Class 7. Tooth dislocation (incomplete).
- Class 8. Complete tooth dislocation.
The classification created by Jacobsen (1981) is simple and accessible to practitioners. However, the classification of Andreason et all (Andreason JO, Andreason F., Andreason L., Textbook and Color Atlas of the Traumatic Injuries to the Teeth, 2007) is most widespread abroad:
- Crown fracture.
- Fracture within the enamel.
- Fracture within enamel and dentin.
- A simple crown-root fracture within the dentine enamel and cementum.
- Fracture within the enamel, dentin and pulp (Fig. 1).
- Complete coronocoronal fracture within the enamel, dentin, pulp and cementum (Fig. 2).
Rice. 1. CT, visualization of tooth 11, MPR; fracture within the enamel, dentin and pulp.
Rice. 2. CT, visualization of tooth 22, sagittal reformat and volumetric rendering; Complete coronal-coronal fracture within the enamel, dentin, pulp and cementum.
- Root fracture.
- Root fracture within cementum, dentin and pulp (Fig. 3).
Rice. 3. CT, visualization of tooth 21, MPR; root fracture within the cementum, dentin and pulp.
- Damage to periodontal tissue.
- Injury.
- Subluxation (subluxation).
- Dislocation with displacement (lateral luxation, Fig. 4, 5).
- Intrusion (impacted dislocation).
- Extrusion (dislocation with extension from the socket, Fig. 6).
- Complete dislocation (avulsion, Fig. 4).
Rice. 4. CT, visualization of tooth 21, MPR; dislocation with displacement (lateral luxation) of tooth 21, complete dislocation (avulsion) of tooth 22.
Rice. 5. CT, visualization of tooth 21, MPR; dislocation with displacement (lateral luxation) of a fragment of tooth 21 (sagittal reformat) and tooth 11 (coronal reformat), fracture of the alveolar process in the area of the alveolar part of the palatal cortical plate (axial reformat).
Rice. 6. CT, visualization of tooth 42, MPR; dislocation with displacement, extrusion (dislocation with extension from the socket).
- Damage to pulp and periodontal tissue.
- Long-term result: a tooth with non-vital pulp, but without destruction of bone tissue in the periapical area (Fig. 7).
Rice. 7. CT, visualization of tooth 23, MPR; trauma three years ago, obliteration of the middle and apical third of the root.
In recent years, dentistry as a science and applied branch of medicine has been actively developing, new technologies are being introduced into everyday practice, and world experience is being adopted. In this regard, it seems possible for us to recommend the Andreason classification and international terminology for use in our country. Below is a list and transcription of terms used in foreign literature when describing conditions associated with dental trauma.
- Fracture (fractura) - fracture.
- Subluxation - mobility without displacement, subluxation.
- Luxation is a dislocation of a tooth or displacement of a tooth fragment.
- Lateral luxation is a lateral displacement with fracture of the socket wall.
- Extrusion - extension from the hole.
- Intrusion - impacting, impacted dislocation (Fig. 8).
- Avulsion - “full luxation”, complete dislocation with tooth extraction.
- Contusion is a bruise of soft tissues.
- Abrasion - abrasion.
- Laceration (laceration) - rupture, dissection.
- Incision - incision, cut.
- Penetration - injury by a small object with its fixation in the tissues.
- Malformation is a developmental defect characterized by a change in shape and structure; violation of morphogenesis.
- Dilaceration - curvature of the root at a large angle or curvature of the crown relative to the root (Fig. 9).
- Inflamation - literally “fire”, inflammation, acute inflammation.
- Exacerbation - literally “outrage”, exacerbation of a chronic process.
Rice. 8. CT visualization of the coronal part of tooth 11 in a state of intrusion, an adult patient with a history of trauma to the primary incisor in childhood.
Rice. 9. CT visualization of rudiment 11, condition after trauma of primary incisors; after avulsion of the incisors, the tooth germ 11 develops in a state of dilaceration; the injury provoked the development of a follicular cyst from germ 11.
A dental therapist examines a patient with dental trauma. He also treats the patient, if necessary, involving a surgeon, orthodontist, or orthopedist. The examination consists of clarifying the victim’s complaints, medical history (questioning), determining the general condition of the patient and the condition of the periodontium in the area of the injured tooth, analyzing the data obtained, establishing a diagnosis and developing a treatment plan.
Until recently, radiodiagnosis (x-ray diagnostics) in dentistry was considered an additional research method, however, when examining injured teeth, this type of research has always been necessary and relevant. Therefore, with regard to dental trauma, we can say that radiodiagnostic testing is mandatory in all cases of trauma.
The maximum information about the condition and position of the injured tooth, as well as the degree of damage to the surrounding bone tissue, is provided by computed tomography (CT), performed on a specialized maxillofacial tomograph with cone beam collimation.
Research using spiral and sequential computed tomographs is extremely rarely used in dentistry, especially in pediatric practice, due to the high radiation exposure and low resolution of image receivers. However, cone beam CT scans with a single planar sensor are designed specifically for examining the maxillofacial region.
Devices of this class provide high image quality, and the radiation dose is only 30-60 microsieverts (0.03-0.06 mSv, which is 2-3 times less than, for example, with conventional radiography of the paranasal sinuses), therefore this method has no direct contraindications for use in pediatric dentistry.
If it is not possible to make a computed tomogram, it is necessary to perform polypositional intraoral radiography. Depending on the sector the tooth belongs to, intraoral photographs are taken in direct (orthoradial) and oblique (eccentric) projections.
It should not be forgotten that, firstly, the study is carried out in cases of severe pain, changes in the configuration of the tissues surrounding the tooth and, in many cases, contamination of the surrounding mucous membrane with blood.
Secondly, to avoid projection distortion when photographing single-rooted teeth, it is necessary to position the image receiver parallel to the vertical axis of the tooth being examined. In this regard, we recommend carrying out the most non-contact and apodactyl positioning with a parallel position of the tooth axis relative to the plane of the sensor or film (orthogonal projection).
When working with a radiovisiograph, this is easily done using a standard positioner. If film is used during the study, it must be fixed in a film-fixer or held by the edge of the cover with a mosquito-type clamp.
In case of combined trauma, panoramic tomography of the dentition (orthopantomography) is performed, however, in case of isolated damage to one or more teeth in the frontal region, this research method should be considered uninformative.
Initially, it is necessary to determine the quality of the radiograph: contrast, sharpness, projection distortions (lengthening, shortening of teeth). The image should be decrypted taking into account these data or a new image should be taken, avoiding previous mistakes.
An analysis of the shadow of the tooth should be carried out, paying attention to the outlines of the crown and root of the tooth, the presence of a cavity in the crown, a filling, and its defects (overhanging edges, loose fit to the walls of the cavity). When studying the image, the size, shape, location of the tooth cavity, the presence of a denticle or intracanal granuloma in it, the location and size of the canal mouths are revealed.
The condition of the root is determined from the radiograph: length, shape, contours, canal width, size of the apical foramen, which characterize the degree of root formation and reveal physiological or pathological root resorption. It is necessary to pay attention to the state of the space of the periodontal ligament and the closing hard plate of the alveolus (lamina dura), monitor its integrity, configuration and compliance with the anatomical shape.
It is necessary to evaluate the condition of the bone tissue surrounding the tooth, the outlines of the apexes of the interdental septa, their relationship with the enamel-cement border, integrity, extent, evaluate the configuration of the bone pattern, identify the presence of pathological changes and determine their nature. Radiation diagnostics are carried out immediately at the time of treatment, several months later, and also, in some cases, a day after the injury.
Repeated identical radiographs of the injured tooth, taken at various intervals, are necessary not only for dynamic monitoring of reparative processes, but also to clarify the diagnosis. This is due to the fact that immediately after the injury (several hours), if there is no significant mobility or change in the position of the coronal part of the tooth, the fracture line may not be visualized. Over time, the fragment shifts, associated with increased swelling of the surrounding tissues and mechanical impact on the crown during chewing, the gap between the fragments widens and becomes clearly visible on the image (Fig. 10).
Rice. 10. Intraoral photographs of tooth 21: a - an hour after the injury, b - a day later.
Despite the rapid development of technology and improvement of treatment methods, acute dental trauma still remains a pressing problem in dentistry. It is almost impossible to foresee or take any measures to prevent situations that provoke dental injury. In this regard, the prognosis in the treatment of OTD largely depends on a timely and correct diagnosis, on the basis of which the optimal treatment method will be selected.
Consequences
Not a single injury for a person passes without a trace. Even if you managed to avoid obvious complications at the time of treatment, there is always a possibility of their occurrence in the future. For a tooth bruise, the consequences are also no exception. One of the most common complications is the gradual death of pulp tissue if the pulp was damaged by an impact, but during treatment, identifying its viability gave positive results. With necrosis, the nerve endings in the tooth cavity are damaged, which inevitably leads to inflammation.
Another most common consequence of a bruise is staining of the enamel. Most often, it occurs in a short time after injury, since fluid from damaged vessels enters the dentinal tubules and stains the walls. In addition, the enamel may simply darken due to a lack of nutrients supplied through damaged fibers and tissues.
More serious complications that arise over time are also possible. This may be the development of a cyst, periodontitis, or a stop in root development in children in both milk and permanent teeth.
Diagnosis of pathology in the dental office
If your tooth hurts or becomes numb after an impact, or if it has moved, you should immediately consult a dentist. The specialist will conduct an external examination and palpation. The doctor will also definitely send you for an X-ray examination to determine the condition of the tissues and their integrity, detect internal damage, and differentiate the bruise from other possible injuries (fracture, dislocation, crack). In order to check the condition of the pulp, to identify traumatic pulpitis and periodontitis, electroodontic diagnostics (EDD) can be performed.
Diagnostics
What action should you take if you or your child gets a tooth bruise? First of all, you need to contact a dental clinic as soon as possible. Using an X-ray, as well as after palpation and a thorough visual examination, the doctor will determine the extent of the damage resulting from the bruise, and will also draw up a detailed plan for further treatment.
When a tooth is bruised, diagnosis must certainly include, in addition to identifying obvious symptoms, an x-ray examination to exclude possible internal injuries, such as a fracture of the root or alveolar process. In addition, damage to the periodontal area, if present, will be visible in the image.
Also, over the course of several days, the doctor must monitor the condition of the pulp using electroodontodiagnosis. It helps to identify even the initial stages of necrosis and remove damaged tissues in time before they begin to become inflamed.
What indicates pathology: characteristic signs
A bruise is an insidious pathology, since immediately after it you may not notice any external manifestations of the injury at all. However, doctors warn that when a blow or bruise occurs, a negative effect on periodontal tissue occurs, their rupture and internal bleeding may occur, and in some cases, the neurovascular bundle, that is, the pulp, is also partially or completely damaged.
How can you independently determine whether you have a problem? We list the main symptoms that should alert you and become a reason for mandatory consultation with a doctor.
- Teeth hurt after being hit. The unpleasant sensations are long-term, aching in nature, intensified by biting and pressing on the crown while chewing food, or by tapping on injured tissues. Acute pain may occur from eating hard, cold and hot, as well as sour and sweet foods.
- After the impact, my teeth became loose. Usually there is slight mobility of the damaged element of the row. It seems to a person that the incisor or fang is swaying and has begun to move to the side.
- The coronal part of the bruised unit has changed its color. Pink color indicates rupture of pulp vessels and internal hemorrhage. If a tooth turns black after an impact, this may indicate a violation of its nutrition and an inflammatory process occurring in the depths of the tissues. If it turns gray, then the symptom signals necrotization and death of the nerve.
Important! As a result of the bruise, partial or complete rupture of the pulp may occur. In the first case, the process is considered reversible, while in the second it is irreversible and requires invasive treatment methods. Only a doctor can find out what problem a particular patient is facing.
- Not only the tooth aches, but also the gums surrounding it. In this case, the bruised soft tissues and mucous membranes swell and turn red. A hematoma may appear.
- Some patients notice numbness in their teeth after an impact, which indicates severe damage to the nerve endings.
“Even if there are no external manifestations of injury, you should still consult a doctor who will conduct a thorough examination. Only on the basis of x-rays can we say for sure whether the patient will require treatment. If you hesitate, you can completely lose a tooth, even one that looks completely healthy,” says dentist-therapist Marina Igorevna Tarabanovskaya.
Treatment
In some cases, if the impact is not very strong, no treatment other than monitoring the condition of the damaged area is required. It is necessary to provide the affected tooth with long-term rest, apply cold compresses to reduce the bruise and relieve swelling. Solid food is completely excluded from the patient's diet for several days. Among other things, the doctor must observe the injured tooth for two to three months to avoid complications.
In children with baby teeth, it is possible to grind off the enamel on the cutting edge to remove the load from the damaged area; this action is not carried out on permanent teeth.
To eliminate the consequences resulting from a severe bruise, treatment should consist of a number of procedures:
- first of all, the damaged area is numbed with an anesthetic;
- if there is damage to the pulp sac, the doctor performs trephination, depulpation and thorough treatment of the dental cavity with disinfectants, after which the canals are sealed;
- if the neurovascular bundle has been damaged and the enamel has darkened or become stained, it is recommended to bleach permanent teeth using hydroperite, which will return the enamel to a more or less natural color;
- if necessary, the doctor can prescribe, in addition to complete rest, anti-inflammatory drugs and physiotherapy to help quickly eliminate the consequences of the injury.
Even if there is no severe pain after a blow to the jaw, it is recommended to visit a dentist to identify possible hidden injuries. This will help you maintain the health of your teeth for many years to come.
What treatment measures do doctors usually prescribe?
In the absence of serious damage
Teeth hurt after a blow: what to do? If, as a result of the examination, it becomes clear that the injury did not bring any serious consequences, then the patient is prescribed the following therapeutic treatment:
- painkillers and syrups for pain relief: read about the best of them in the feature article on the website,
- cold compresses to relieve swelling and resolve bruises,
- treatment of inflamed gums with antiseptic solutions and anti-inflammatory ointments: you can rinse your mouth with Chlorhexidine and Miramistin, use topical gels, for example, Cholisal,
- gentle diet: the bruised element of the row should be at rest, which is why during the rehabilitation period (on average it takes up to 3-4 weeks) it is not recommended to eat hard and hard food, or chew on the side of the jaw that has been subjected to mechanical stress. You should not eat cold or hot, as this can cause pain and have an irritating effect. It is better to eat soft and pureed foods, ground in a blender, as well as liquid foods at a neutral temperature,
- physiotherapy: for rapid healing of damaged tissues, laser and magnetic therapy, UHF (ultra high frequency) therapy are usually prescribed. The course consists of 10 procedures of 5 minutes each.
On a note! For 2-3 months after a bruise or blow, it is recommended to carry out dynamic observation even in cases where no serious damage has been identified. During the process[1] of observation, the doctor can adjust treatment tactics and decide on the use of non-invasive and invasive methods. Subsequently, adults should visit the dentist 2 times a year and children 3-4 times a year for preventive examinations.
For pulpitis and periodontitis
How to save a tooth after an impact? If the injury leads to damage to the pulp, the development of pulpitis and periodontitis, then specialists perform trepanation of the crown, that is, they open it. Doctors gain access to the root canals, remove the nerve if necessary, carry out treatment, anti-inflammatory and antiseptic treatment, and filling. All procedures are performed under local anesthesia.
When changing shade
If a tooth has darkened after an impact, the patient is offered intracanal bleaching, which allows the element of the row to be restored to its former whiteness. However, the procedure is performed only on pulpless units, that is, when the nerve has been removed from them. What to do if the pulp was saved? You can hide the defect and restore the aesthetics of the anterior incisors and canines with composite restorations, veneers and lumineers, crowns made of ceramics and zirconium dioxide.
A change in the shade of the crown often occurs due to incomplete rupture of the pulp, which causes a hematoma to form in the tissue. According to some studies, the crown acquires its natural color after the hematoma resolves, so in the first days after the injury, patients are often simply prescribed dynamic observation.
With mobility of the bruised unit
How to ensure complete rest and strengthen a tooth after an impact if it begins to wobble? For this purpose, doctors may install temporary immobilization and splinting devices for you. The splints will fix the movable unit in a stable position, unite it with healthy ones, help the correct distribution of the chewing load and allow therapeutic treatment until damaged or torn ligaments are restored. They need to be worn from several weeks to several months. During the period of immobilization, it is very important to follow a gentle diet and give up solid food.
On a note! If a row of milk units is bruised, splints are not placed, and rest is provided to the moving element using mouth guards, which temporarily separate the bite and prevent direct contact with the antagonist teeth. To reduce the load on the bruised element, children also undergo grinding of the cutting edge of the antagonist crown.
For increased tissue sensitivity
Often after a bruise, increased sensitivity of hard tissues occurs. They begin to react to food temperature and mechanical stress, and then experts recommend a course of fluoridation or remineralization of the enamel. In the process, products with minerals are applied to hard tissues, promoting strengthening and increasing resistance to caries and any external factors.
When chips and cracks form
Often, a blow or bruise to the incisors and fangs leads to the formation of cracks and chips on them, and to the destruction of hard tissues. In these cases, to restore the aesthetics, original form and functionality of the damaged elements, patients undergo artistic restorations with composite materials, and microprostheses (veneers and lumineers) are installed. If the destruction is extensive, then prosthetic crowns are prescribed.