The main criteria for the treatment of gingivitis are:
- Complexity
Each specific case requires a number of therapeutic procedures. Both local and general treatment are necessary. Therapy should be aimed not only at relieving symptoms, but also at the causative factors.
- Individuality
The features of the clinical course, associated problems (their presence and nature), as well as factors of local and general defense of the patient’s body (the state of the immune system) must be taken into account.
- Systematicity
Chronic forms of the disease require regular courses of maintenance therapy to bring the disease into stable remission.
Treatment tactics depend, first of all, on the form of the disease. Let us consider in detail the specifics of treatment of three forms of gingivitis. This will help you understand the basic principles of therapy and roughly explain how your dentist will treat gingivitis.
Gingivitis: causes and symptoms
In order to know how to treat gingivitis, it is necessary to study at least brief information about this disease and the mechanisms of its occurrence. Gingivitis is a fairly common dental disease, which is an inflammation of the gums, which can be treated with dental ointments and rinses. These rules are similar for the prevention of stomatitis.
The occurrence of gingivitis is often associated with improper oral care, which results in the formation of plaque consisting of bacteria. This sticky substance accumulates along the edges of the gums and in places that are difficult to reach with a regular toothbrush.
In most cases, the causative agents of gingivitis are pathogenic microorganisms that live in the oral cavity of healthy people. The immune system does not allow bacteria to manifest itself, but when it weakens, the virus begins to progress in the body. Among the reasons that can trigger the development of the disease are the following:
- Neglect of dental treatment;
- Poor quality prosthetics and installation of braces;
- Diabetes;
- Viral diseases of the upper respiratory tract;
- Hormonal imbalance, for example, during pregnancy;
- Unbalanced diet, especially lack of vitamins C;
- Nicotine abuse.
Many experts do not consider gingivitis to be an independent disease. In their opinion, the disease develops against the background of other pathologies that contribute to a decrease in the body’s immune defense.
Symptoms of simple gingivitis include swelling and redness of the gums, which may bleed when eating or brushing teeth, and gums often pull away from the teeth. The general clinical picture of the disease looks like this:
- Increased sensitivity of teeth and gums;
- The appearance of dental plaque and tartar;
- Bad breath;
- Swelling;
- Pain and burning when biting;
- Soft tissue necrosis.
There may be no pain, but with acute gingivitis there is already severe pain. In addition, if gingivitis is not treated promptly, complications may develop and numerous ulcers may appear.
Treatment of chronic catarrhal gingivitis
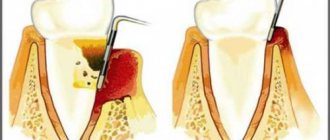
- The first and mandatory step in therapy is professional teeth cleaning - removing tartar and smoothing the surface of the teeth using ultrasonic and sandblasting devices. The steps of the procedure are shown in the figure below.
- Training in proper individual oral hygiene.
- Elimination of local factors that contribute to the formation of plaque - treatment of caries, correction of orthodontic and orthopedic structures.
- Relief of a problem that aggravates the effect of a microbial factor - elimination of injuries, treatment of pathology of the attachment of the frenulum (plastic surgery to enlarge the frenulum).
- Antibiotics and anti-inflammatory drugs in the form of oral baths, applications, irrigations are used for gingivitis at the stage of a pronounced inflammatory process.
- To improve the process of tissue regeneration, keratolytic agents are used (sea buckthorn and rose hip oil, solcoseryl, vitamins A and E).
- General strengthening therapy is necessary - the use of vitamins, adaptogens, antioxidant therapy, and means to normalize metabolism.
Catarrhal gingivitis: symptoms
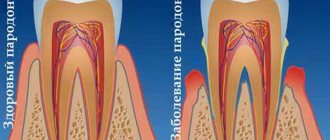
Among all patients with gingivitis, this form accounts for more than 97% of cases. Those. This is the most common form of this disease. The term “catarrhal” means that the inflammation affects only the mucous membrane of the gums, i.e. flows superficially. Thus, with gingivitis, there is no destruction of the bone tissue around the teeth, as well as destruction of the periodontal attachment. In Fig. 3-5 you can see what catarrhal gingivitis looks like in the oral cavity.
The cause is exceptionally insufficient oral hygiene, as a result of which soft microbial plaque accumulates in the area of the necks of teeth, and the formation of tartar occurs. Plaque bacteria produce toxins and pathogens, which trigger inflammation in the gum mucosa. At the same time, various chronic diseases or vitamin C deficiency are not the direct causes of the development of gingivitis, but may be a predisposing factor that increases the impact of microbial plaque.
Catarrhal gingivitis: photo
Symptoms –
- swelling of the gingival margin and interdental papillae,
- redness or bluishness of the gums,
- bleeding gums when brushing teeth,
- pain when brushing teeth,
- itching in the gums,
- Usually, accumulations of microbial plaque are visible at the necks of teeth.
The appearance of bleeding is associated with an increase in the permeability of capillary walls, capillary fragility, as well as a decrease in the thickness of the epithelium of the gum mucosa. All this arises as a result of the influence of toxins and microbial plaque pathogens on the mucous membrane of the gums. Most often, bleeding occurs when the gums are exposed to mechanical factors (for example, when brushing teeth or chewing rough, hard food).
Pain when brushing teeth is also associated with thinning of the epithelium of the gum mucosa. Thinning of the epithelium against the background of gum inflammation is a natural process, and develops due to an increase in the rate of desquamation of epithelial cells (24stoma.ru).
Forms of catarrhal gingivitis –
There are 2 variants of the course of the catarrhal form of gingivitis. Firstly, there is acute catarrhal gingivitis (Fig. 3-4), which is characterized by bright red gum color, acute development, and sometimes significant bleeding and pain when brushing teeth. With this form of the disease (due to pain when brushing teeth), patients sometimes abandon oral hygiene altogether, which leads to an even greater increase in the amount of microbial plaque, and as a result, to an increase in gum inflammation.
Secondly, the chronic form of the disease (Fig. 5-6), which is characterized by sluggish symptoms over a long period of time. Chronic catarrhal gingivitis symptoms of bleeding will be quite minor, and pain during brushing may be completely absent. The marginal gum and periodontal papillae will have a bluish color. However, exacerbation of symptoms may periodically occur, which usually occurs against the background of a decrease in immunity during the period of colds.
Chronic catarrhal gingivitis –
Treatment of ulcerative gingivitis
Therapeutic measures should be aimed at eliminating the inflammatory process, increasing the patient’s body’s resistance to microbes, and preventing the influence of local factors that provoke necrotizing ulcerative gingivitis. Let's consider the main stages and principles of the treatment.
- Professional oral hygiene.
- Antibacterial and anti-inflammatory therapy.
- One of the features of the treatment of necrotizing ulcerative gingivitis is the removal of necrotic areas of tissue; Hydrogen peroxide and chlorhexidine are usually used.
- The use of keratolytic agents, vitamins, adaptogens.
- Training in the rules of proper oral hygiene, as well as monitoring hygienic skills.
- One of the features of the ulcerative form of the disease is severe pain, therefore the treatment of gingivitis, due to the difficulty of carrying out normal hygienic care, is accompanied by the use of antiseptics and anti-plaque agents.
- Elimination of factors contributing to the formation of plaque on the surface of teeth.
- Elimination of the problem that aggravates the proliferation of microorganisms and their pathogenic effects.
Types of diseases
There are several types of gingivitis, so for effective treatment it is necessary to determine the form of the disease. The following options are possible here:
- Catarrhal. One of the most common forms, which is diagnosed in most patients. The disease manifests itself as bleeding gums and discomfort when pressing on soft tissues.
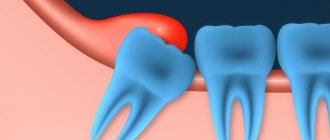
- Hypertrophic. Usually diagnosed during adolescence. The source of inflammation is located in the area of the front teeth. A characteristic feature of this form of the disease is the proliferation of interdental papillae, and soft tissue hyperplasia is possible.
- Ulcerative-necrotic. This is an advanced stage, which is manifested by acute pain, ulcers in the mouth, and excessive salivation. Patients experience lack of appetite, high fever, and enlarged lymph nodes.
- Atrophic. The most severe form, in which atrophy of soft tissues is observed, the roots of the teeth are exposed. Characteristic signs of this disease are a gray tint of the mucous membrane and bad breath. The patient experiences general weakness and severe pain.
According to the form of its occurrence, gingivitis is divided into chronic and acute. In the first case, the disease does not have pronounced symptoms, there is practically no pain, the gums bleed only when brushing the teeth. In the second, the disease manifests itself more acutely and gives the patient a lot of discomfort.
Treatment of hypertrophic gingivitis
The principle and procedure for carrying out treatment procedures is similar to those for catarrhal gingivitis. However, the hypertrophic form sometimes requires surgical intervention.
Gingivectomy is a procedure performed to remove diseased tissue. Its stages can be seen in the figure below. Gingivectomy allows you to get rid of a large amount of excess tissue and prevent the accumulation of plaque, as well as stop the intensification of the inflammatory process.
Stages of gingivectomy
Classification of gingivitis according to ICD:
- K05.0. Acute gingivitis
- K05.00 Acute streptococcal gingivostomatitis
- K05.08 Other specified acute gingivitis
- K05.09 Acute unspecified gingivitis
- K05.1. Chronic gingivitis
- K05.10 Simple marginal gingivitis
- K05.19 Chronic unspecified gingivitis
- K06.0. Gum recession.
- K06.1. Gingival hypertrophy.
- K06.2. Lesions of the gums and edentulous alveolar margin caused by trauma.
- K06.9. Changes in the gingiva and edentulous alveolar margin, unspecified.
Treatment of gingivitis at home
Gingivitis is an inflammatory process that can be eliminated without serious medical intervention. At this stage, treatment with folk remedies is effective. But if the disease is left to chance, gingivitis can cause periodontitis, a disease that is much more difficult to cure. Therefore, treatment of gingivitis in children and adults is also reliable prevention.
A decoction of oak bark, medicinal chamomile, sage, as well as commercial anti-inflammatory drugs are used to treat gingivitis at home. They have a soothing, antimicrobial and astringent effect.
Gingivitis: treatment at home
Once again, let us draw your attention to a very important point - treatment of gingivitis in adults at home is only possible in terms of a course of anti-inflammatory therapy. At home, you can successfully use antiseptic rinses and applications to treat catarrhal gingivitis, but to remove plaque, you still need to visit the dentist!
A small example: a person’s gums are bleeding and he decides to use the remedies he heard about in an advertisement. These can be various gels, rinses or anti-inflammatory toothpastes. And indeed, as long as a person uses such means, bleeding decreases or disappears completely for a while. But as soon as the use of the products is stopped, the gums begin to bleed again, plus their swelling and redness return.
The reason for this is quite commonplace - the person tried to treat the symptoms (such as bleeding, pain, swelling) without removing the cause of these symptoms (microbial plaque, as well as hard supra- and subgingival dental plaque). Advertisements for various dental products do not talk about the causes of bleeding or the need to remove dental plaque. Moreover, for obvious reasons... We hope that our article on the topic: Gingivitis symptoms and treatment in adults was useful to you!
Sources:
1. Dental education of the author of the article, 2. Based on personal experience as a periodontist, 3. National Library of Medicine (USA), 4. American Academy of Periodontology (USA), 5. “Non-surgical periodontal treatment” (Roncati M.).
Simple ways to get rid of a difficult disease: prevention of gingivitis
The best and main method of prevention is compliance with oral hygiene measures.
Personal hygiene
Regular and high-quality teeth brushing (at least twice a day). It is important to know how to choose the right toothbrush; its bristles should not injure the gums, but at the same time remove plaque well. And also use the toothpaste that is suitable for you.
Brushing your tongue is an important part of oral hygiene and should be cleaned as often as your teeth.
It is necessary to use a mouthwash whose antiseptic properties kill most known microorganisms. It is advisable to use it after every meal.
Cleaning the interdental spaces with dental floss at least once a day. It helps remove all food particles that the toothbrush cannot reach, thereby preventing plaque from accumulating in between the teeth.
If you are the owner of dentures, veneers, crowns or implants, then you cannot do without an irrigator. It perfectly cleans the surface of artificial structures, as well as the joints between them and natural teeth.
Visit the dentist every six months
In addition to the consultation appointment, the periodontist will, if necessary, perform professional teeth cleaning. It includes:
- removal of hard dental deposits and soft plaque from tooth surfaces. This cleaning can be carried out using ultrasound or an Air Flow device;
- polishing teeth with a special paste that prevents tartar deposits. In addition to the polishing effect, it has the property of remineralizing tooth enamel, as it contains calcium and fluoride;
- carrying out medical applications on the gums with an antiseptic solution.
Following these really simple methods will help you avoid a whole host of gum and dental problems.
Cure gingivitis is the last opportunity to stop the serious process of inflammation of periodontal tissues - periodontitis, which leads to the loosening of healthy teeth and their loss. In addition, treatment of periodontitis is much more difficult and less effective. Therefore, if you have the slightest problem with your gums, do not forget to see a doctor.
Diagnostics
Diagnosis of gingivitis is carried out in several ways, which are used in combination. At the initial stage, the doctor collects anamnesis:
- The diet and bad habits are revealed;
- The reasons for tooth extraction/loss are clarified;
- Genetic predisposition is determined.
After this, an examination of the oral cavity is carried out, the depth of the dental canals is studied with a special probe. Additional methods of diagnostic testing include x-rays and testing the sensitivity of the pulp.
The following methods can be used to diagnose gingivitis:
- Fedorov-Volodkina index;
- RMA index;
- Schiller-Pisarev test.
Answers to popular questions
How to stop bleeding gums at home?
Herbal rinses (for example, oak bark) will help stop the bleeding, but they only give a temporary effect and mask the problem.
Can a hard brush cause gingivitis?
No, the brush itself does not cause gingivitis, but too hard bristles can damage the enamel. For most people, medium-hard brushes are suitable.
I don’t have problems with my gums, but my gums often hurt and bleed in only one place, what should I do?
It's worth seeing a doctor. Most likely, there is an old filling in this place, in which food gets stuck and inflammation begins.
Is gingivitis curable or is it permanent?
Fortunately, yes, if you follow all the recommendations, you will not only cure gingivitis, but also not see it again.
Local drug therapy for periodontal diseases
Local drug treatment of periodontal diseases includes the use of agents that affect etiological factors, pathogenetic mechanisms and symptoms of diseases. The dosage forms are dosed, the methods of using the drugs are adapted to local use. Medications can be used in the form of rinses, irrigations, gum dressings, and treatment plates.
As etiotropic treatment, antibacterial drugs are used that act on the cause of the disease and prevent secondary infection. Antiseptics are most often used (2-3% hydrogen peroxide solution; chlorhexidine digluconate - 0.05%; lizoplak; chlorophyllipt; iodinol; lozenges - ambazon, sebidine). Antibiotics can be used in the form of rinses, applications or parenterally (tetracycline ointment; synthomycin emulsion; gramicidin - 2% solution; microcide; levovinisol - aerosol; 0.1% gentamicin sulfate ointment; lincomycin - parenterally). Less commonly used are sulfonamides (streptocide - in the form of a powder; ingalipt - an aerosol), drugs of the nirofuran series (0.02% aqueous solution or 0.2% furacillin ointment).
Pathogenetic treatment consists of the use of anti-inflammatory drugs - non-steroidal (sodium mefenamate in the form of a paste, ointment; romazulan; 10% methyluracil ointment; etonium), steroidal (0.5-2.5% hydrocortisone, 0.5% prednisolone ointment, lorinden, dermosolone). These same drugs have an anti-edematous effect.
Oil solutions of vitamins A, E, rosehip oil, carotoline, AEvit, methyluracil, solcoseryl, vinylin have epithelializing and reparative effects. Galascorbine and calcium salts help reduce the permeability of the vascular wall.
The most effective is the use of broad-spectrum agents. Thus, etonium, dimexide, parodium, eludril have anti-inflammatory, local anesthetic, antimicrobial, and epithelializing properties.
Symptomatic treatment includes painkillers: parenterally (in the form of infiltration or conduction anesthesia), application in the form of solutions, ointments, aerosols (5% anesthetic ointment, 1% pyramecaine ointment, etonium, pharmacoethyl).
Local hemostatic drugs are used for appropriate indications (galascorbin, hemostatic sponge, bioplastic, capramine, racestiptin, hemocollagen, hemofibrin).
Proteolytic enzymes are used when it is necessary to soften and remove plaque (trypsin, chymotrypsin, chymopsin, papain).
Parodium paste (Pierre Fabre), containing chlorhexidine and rhubarb extract, is applied in a layer of 0.2-0.5 mm along the marginal gum and compacted with a tampon.
Therapeutic paste-bandage for the treatment of periodontal vitadont (“VladMiVa”) based on lecithin contains a complex of natural antioxidants, vitamins C, E and beta-carotene. The paste is applied to the dried mucosa, into the periodontal canals and to the edge of the gums and left for several hours.
Wokopak paste (VOKO) is used in the treatment of periodontitis, after gingivectomy and other surgical interventions.
Diplen-denta (“Nord-Ost”) - plates for the treatment and prevention of inflammatory diseases of the oral cavity. Several types are available: diplendenta X - with chlorhexidine; diplendenta HD - with chlorhexidine and dexamethasone; diplendenta LH - with chlorhexidine and lidocaine; diplen-denta G - with gentamicin; diplen-denta L - with lincomycin; diplen-denta M - with metronidazole; diplendenta F - with sodium fluorine and chlorhexidine; diplen-denta C - with solcoseryl.
KP-plast (“VladMiVa”) - self-absorbable plates measuring 50×80 mm for the treatment and prevention of inflammatory diseases of the oral cavity. They produce several types: KP-plast-phyto contains natural polysaccharides, extracts of chamomile, yarrow, calendula, vitamin C, plasticizers and antioxidants; KP-plast-vita - a plate based on natural polysaccharides, also contains vitamins C, E and beta-carotene; KP-plast antimicrobial - a plate based on natural polysaccharides and polypeptides, contains chlorhexidine and metronidazole; KP-plast-anesto - a plate with anesthetic and vitamins; KP-plast-hemostatic. To use, cut off the required fragment of the plate and place it on the affected area of the gum. Hold it for 1 hour. The course consists of 10 daily applications; if necessary, the course is repeated after 10 days.
Septo-Pak (“Septodont”) is a protective bandage for gums that contains amyl acetate, butyl phthalate, zinc oxide and zinc sulfate. Can be used with medications for local periodontitis and after periodontal surgery.
Solcoseryl dental adhesive paste (“Solko”) contains an extract from cattle blood (2.125 mg per 1 g of paste) in combination with polidocanol (a local anesthetic). A strip of paste 0.5 cm long is applied, without rubbing, to a previously dried area of the mucous membrane and lightly moistened with water. The procedure is repeated 3-5 times a day after meals and before bedtime. When treating bedsores from removable dentures, the paste is applied to a dry denture and moistened with water. Per course - 5 g (1 tube).
Differentiated choice of means and methods of treatment
Treatment of herpetic gingivitis is aimed at etiopathogenetic factors and takes into account the severity of the disease. Complex therapy includes general and local effects. From the first days of the development of the disease, it is necessary to use antiviral ointments (0.25% oxolinic; 0.25-0.5% florenal; 0.25-0.5% tebrofen; 50% interferon; 0. 25% bonaftone; 0.75% glycerin; 0.25% riodoxol; 1% alpizarin; 1% helipelin). Modern antiherpetic drugs are especially effective: acyclovir ointment, herpevir, 2% solution of Zovirax. They are recommended to be used repeatedly (3-4 times a day) after antiseptic treatment of the oral mucosa.
It is advisable to use painkillers when treating oral mucosa: 5% anesthetic emulsion, 1% pyromicaine ointment. Herbal medicinal preparations are used as antiseptics: warty birch (buds, leaves, sap), Scots pine (pine buds, resin, needles), eucalyptus leaves, colanchoe juice, calendula; collection "Elekasol" (chain grass, chamomile flowers, licorice roots, sage and eucalyptus leaves, calendula flowers). These agents have epithelializing, anti-inflammatory, antimycotic and antiviral effects against the herpes virus.
It is advisable to use painkillers when treating oral mucosa: 5% anesthetic emulsion, 1% pyromicain ointment.
During the period of extinction of the disease, keratoplasty preparations acquire leading importance: rosehip and sea buckthorn oil, carotolin, solcoseryl ointment and jelly, vinylin, oil solution of vitamin A, E, “Gipozol”, “Vinizol”.
General treatment of herpetic stomatitis should be carried out for moderate and severe forms of acute stomatitis. In the first stages of the disease, antiviral drugs are prescribed according to the age-specific dosage: bonafton 0.1, alpizarin 0.1, helipin 0.1, 2 or 4 tablets per day for 5-10 days. Acyclovir (Gerpevir, Verolex, Ciclovir) has high selectivity for the herpes virus and low toxicity. Adults need to take 200 mg of acyclovir 5 times a day every 4 hours. For children under 2 years of age, the drug is prescribed 100 mg 5 times a day, and after 2 years of age, adult doses are prescribed. Timely administration of medications leads to a reduction in future relapses of herpetic diseases.
During the height of the disease, physiotherapy is usually prescribed: ultraviolet irradiation, GNL, the use of percutaneous laser biostimulation of blood. In the complex of general treatment, hyposensitizing therapy (suprastin, diazolin, tavegil, pipolfen and others) is carried out in age-appropriate doses. Complex therapy includes agents that stimulate the immune system: lysozyme - 75-100 mg daily for 5-10 days; human leukocyte immunoglobulin and antiherpetic immunoglobulin 1.5-3.0 ml 1 time every 3-4 days (2 or 3 injections); leukocyte interferon, cycloferon 2.0 - 1 time per day (1, 2, 4, 6, 8 days); Thymalin; methyluracil, sodium nucleinate, decaris (levamisole), echinacea preparations (immunal, estifan).
During the height of the disease, physiotherapy is prescribed: ultraviolet irradiation, GNL, the use of percutaneous laser biostimulation of blood.
Rational nutrition involves the introduction of a sufficient amount of fluid: liquid, non-irritating, high-calorie foods.
Acute gingivitis with severe bleeding
Treatment begins after identifying the common cause with training in individual oral hygiene and recommendations on the choice of hygiene products: a soft toothbrush, non-abrasive toothpaste. Mouth rinsing involves the use of solutions that have an antibacterial effect. Hemostatic agents are used for appropriate indications in the form of applications (hydrogen peroxide, capramine, alascorbine, aminocaproic acid), treatment plates (KP-plast-hemostatic), hemostatic sponge, capramine, hemocollagen, hemofibrin.
Professional hygiene is carried out sparingly, in individual segments of the jaw, followed by the application of drugs that reduce bleeding. In the process of removing dental plaque, abundant irrigation of antiseptic solutions is performed (chlorhexidine 0.05%; furatsilin 1:5,000). In case of severe pain, pain relief is performed: application or injection. For use at home, lozenges (Sebidine, Faringosept, Drill) can be prescribed.
In the presence of local traumatic factors, overhanging edges are ground down, prostheses are corrected, etc.
General treatment is prescribed by an internist in accordance with the general condition of the patient.
Local treatment of ulcerative gingivitis
Includes the prescription of pain-relieving applications (2% oil solution of anasthesin, 1% pyromicaine ointment), lysozyme baths (1 glass of boiled water, the white of 1 egg and 1/4 part of a teaspoon of salt), rinsing with herbal decoctions (chamomile, St. John's wort, calendula), 0.5-1% aqueous solution of galascorbine, romazulan, chlorophyllipt. To cleanse the surface of ulcers and erosions from necrotic plaque, it is possible to use enzymes (trypsin, chemotrypsin, pancreatin).
When epithelialization begins, it is necessary to use agents that promote reparative processes in tissues (carotolin, sea buckthorn and rosehip oil, vinylin, vinylsol, solcoseryl ointment and jelly, etc.), immunostimulants (1% sodium nucleinate solution, 5% methyluracil ointment) .
Prevention of exacerbations consists of eliminating microtraumas of the oral mucosa, allergens that cause hypersensitivity of the body, prescribing desensitizing agents, restorative therapy, hardening the body. Physiotherapeutic methods of treatment include ultraviolet irradiation on the lesions (5-6 biodoses), low-intensity radiation from a helium-neon laser (HNL) at a power of 100 mW/cm2 for 2 minutes, number of fields no more than 5, course up to 10-15 sessions. In severe cases, supravenous irradiation of GNL blood is indicated for 20 minutes, for a course of 10 sessions (repeat twice a year in the inter-relapse period) of magnetic autohemotherapy (blood taken from a vein into a syringe, placed for 10-15 minutes in a magnetic field, after training injected intramuscularly 8-10 injections).
Prevention of exacerbations consists of eliminating microtraumas of the oral mucosa, allergens that cause hypersensitivity of the body, prescribing desensitizing agents, restorative therapy, and hardening the body.
Treatment of desquamative gingivitis
Includes the elimination of locally irritating factors, professional hygiene, and training in individual oral care. The patient is recommended to choose a soft toothbrush, interdental teeth cleaning products, and a non-abrasive paste, preferably in the form of a gel, based on herbal preparations. Local drug treatment involves the use of drugs that have an epithelializing effect: oil solutions of vitamins A, E, rosehip oil, carotoline, AEvit, methyluracil, solcoseryl, vinylin. These same drugs stimulate the regeneration of connective tissue. Oil solutions of vitamins A, E, carotoline are used in the form of applications 3-5 times a day. In the form of rinses, you can prescribe medicinal elixirs and herbal infusions (sage, chamomile).
The sensitivity of the gums to irritants is an indication for the prescription of painkillers. In the form of applications, you can use a 5% anesthetic emulsion, 1% pyromecaine ointment. It is recommended to eat bland food. Vitamin therapy is indicated.
General medications are prescribed by an internist in accordance with the identified diseases. Along with drug treatment, laser therapy is recommended. Irradiation technique: remote, stable, light guide with a conical attachment is located 3 mm from the gum surface, the diameter of the light spot is 3 mm. Physical parameters: LILI in the red range of the spectrum, power 5 mW, PPM ~ 70 mW/cm2, exposure 40 seconds, radiation dose per field 2.8 J/cm2, 10 irradiation fields per session. The course of treatment is 10 sessions.
Treatment of periodontitis
In mild cases, it is limited to local influences (in the absence of a common etiological factor). General strengthening drugs (vitamins) and an adaptogen (Eleutherococcus in microdoses) may be prescribed.
Motivation and training in individual hygiene is carried out on the first visit. Depending on the clinical situation, a toothbrush, interdental agents and toothpaste are selected. If dense plaque is detected and there is no bleeding gums, a high-hardness brush is recommended, and an abrasive paste is recommended.
In other cases, choose a brush with medium-hard bristles and a therapeutic and prophylactic toothpaste, including ingredients with an anti-inflammatory effect (Elgidium).
Professional hygiene is carried out by a dentist in several stages. The number of visits depends on the method of removing dental plaque. The use of the Vector system ensures the treatment of dentition in one session. Sound scalers allow you to limit yourself to two stages. Manual removal will require an additional visit to polish the root surfaces.
During the first or second visit, other locally irritating factors are eliminated: overhanging edges of fillings, spaces between teeth, etc. Selective grinding of the teeth is performed. According to indications, surgical interventions are performed: excision of the frenulum, removal of a tooth located outside the arch, etc.
Drug treatment depends on the pattern of symptomatic gingivitis and can be used minimally. Rinsing, irrigation of solutions in the process of professional hygiene. Applications at home of oil solutions of vitamins A, E in the presence of epithelial desquamation. Physiotherapy methods include hydromassage and electrophoresis with galascorbine. The laser beam has a good effect.
Treatment of a patient with moderate severity of periodontitis
Includes general and local effects. Therapy for a concomitant disease is prescribed by a specialist in a specific branch of medicine. In parallel, agents that increase the overall resistance of the body may be recommended: vitamins, Eleutherococcus extract in adaptive doses, potassium orotate.
Local exposure involves motivation, training in individual oral hygiene with a careful selection of products and methods used 2-3 times a day at home. In cases of violation of the integrity of the epithelial cover of the gums (desquamative or ulcerative gingivitis), severe bleeding and hyperesthesia of the teeth, preference is given to a brush with soft bristles and gel toothpaste based on herbal preparations. Dental floss, brushes, and toothpicks are used extremely carefully.
The sensitivity of the gums to irritants is an indication for the prescription of painkillers. In the form of applications, you can use a 5% anesthetic emulsion, 1% pyromecaine ointment. It is recommended to eat bland food. Vitamin therapy is indicated. Professional hygiene can combine the removal of heavy dental plaque with hand instruments followed by treatment of the root surface with ultrasonic tips. The number of visits depends on the clinical picture and methods used. Studies have shown that the use of an ultrasonic scaler allows you to limit yourself to two sessions; manual instruments require additional stages of work. The most gentle way is to use the Vector system. A prerequisite is to reduce or eliminate irritating influences. The dentist-therapist performs correction of low-quality restorations. According to indications, tooth depulpation can be performed.
The orthopedist corrects low-quality dentures, carries out selective grinding, and, if necessary, splinting of mobile teeth.
The choice of medications depends on the clinical manifestations, namely the symptoms of gingivitis. An obligatory element of the medicinal effect is the use of antiseptics (2% hydrogen peroxide solution, potassium permanganate, chlorhexidine bigluconate).
According to indications, hemostatic agents (capramine, hemofibrin), analgesics (ethonium, anesthesin), and epithelializing agents (vitamins, sodium mefenamate, methyluracil) are used. The patient can independently use rinse solutions, aerosols (proposol), lozenges (strepsil), and spray.
Gum dressings (parodium, vokopak) and treatment plates (diplen-denta) are professionally applied. Treatment of a patient with severe (chronic complex) periodontitis includes general and local treatments.
General therapy is carried out by a specialist in accordance with the underlying disease. In parallel, drugs are prescribed that increase the general resistance of the body: vitamins, Eleutherococcus extract in adaptive doses, potassium orotate.
Treatment by a dentist involves motivation, training in individual oral hygiene with the selection of optimal products and methods used at home.
For desquamative or ulcerative gingivitis with bleeding gums and dental hyperesthesia, select a brush with soft bristles and gel toothpaste based on herbal preparations. Dental floss, brushes, and toothpicks are used only after eliminating defects in the gum mucosa.
Professional hygiene is carried out gently, step by step, using painkillers. Removal of heavy dental plaque is carried out with hand instruments, followed by treatment of the root surface with ultrasonic tips and polishing pastes.
Movable teeth must be splinted before professional hygiene. The number of visits depends on the clinical picture, in particular the condition of the gums. The use of an ultrasonic scaler allows you to limit the number of sessions compared to manual instruments.
A prerequisite for specific treatment of periodontitis is the reduction or elimination of irritating influences.
The dentist-therapist makes corrections to existing restorations. According to indications, tooth depulpation is carried out. The peculiarity of endodontic treatment is the need to treat retrograde pulpitis or tooth depulpation with reduced electrical excitability of the pulp.
An orthopedist corrects low-quality dentures, carries out selective grinding when splinting mobile teeth, and immobilization of teeth precedes professional hygiene.
The choice of medications depends on the clinical manifestations, including symptoms of gingivitis. Local therapy affects etiological factors, pathogenetic mechanisms and symptoms of the disease.
Treatment by a dentist involves motivation, training in individual oral hygiene with the selection of optimal means and methods used at home. In addition to solutions, ointments, and powders, medications can be used in the form of gum dressings and treatment plates. A layer of 0.2-0.5 mm of parodium is applied along the marginal gum and compacted with a tampon. Vokopak is used in the treatment of periodontitis, after gingivectomy and other surgical interventions. Diplen-denta (Nord-Ost) - plates for the treatment and prevention of inflammatory diseases of the oral cavity. Septo-Pak (“Septodont”) is a protective bandage for gums that contains amyl acetate, butyl phthalate, zinc oxide and zinc sulfate. Can be used with medications and after surgical interventions on periodontal tissues.
Suppuration from pockets requires the most intensive drug therapy, so local use of antibiotics is justified. The choice of antibiotic is best done by determining the sensitivity of microorganisms to it.
Surgical interventions can consist of eliminating the root cause (excision of frenulum, strands of the mucous membrane) or eliminating the inflammatory process (gingivotomy, gingivectomy, open curettage, flap surgery). Anesthesia and surgical intervention are performed in accordance with local and general indications.
Physiotherapeutic treatment can be carried out before and after surgery. Good results are shown by the use of a helium-neon laser, which has an analgesic, bactericidal, and epithelializing effect.