|
|
Why do trophic ulcers appear?
There are a number of provoking factors that contribute to the occurrence of such defects. Namely, if the patient has:
- Varicose veins of the saphenous veins. This disease is at the forefront among other diseases that can lead to the appearance of TU. When the subcutaneous veins of the legs dilate, the outflow of venous blood is significantly impaired, as a result, it stagnates in the dilated area. Persistent venous hypertension develops. Scientists measured blood pressure in varicose veins in patients who stood on their feet for a long time; the figure reached 250 mmHg! Venous blood does not have the ability to provide nutrition and oxygenation to tissues, and as a result of its stagnation, the skin is not supplied with the necessary elements. Trophic tissue disorders appear, their gradual destruction occurs, and a superficial, long-term non-healing wound is formed. It will certainly become an ulcer in the future.
- Thrombosis of the main veins. In the long-term period after phlebothrombosis, a significant and irreversible narrowing of the lumen of blood vessels occurs. The normal outflow of venous blood is disrupted, and stagnation occurs in the most distant segments of the leg (foot, lower third of the leg). Then everything happens similarly to the above, only the scale and extent of the process are more significant.
- Stenosing atherosclerosis. Atherosclerotic plaques form on the arterial walls. Over time, such plaques grow, resulting in the lumen of the blood vessel being completely obliterated. Because of this, arterial blood does not pass through the vessels and does not supply tissues with oxygen and nutrients (ischemia, hypoxia). In the latter, irreversible processes develop. Subsequently, the skin in this area becomes thinner, and TJ develops.
- Infectious skin lesions. Some skin infections and fungal infections, combined with reduced immunity and impaired skin nutrition, can provoke the formation of a trophic ulcer. This is explained by the fact that some bacteria have the ability to destroy skin cells. In addition, they can cause disruption of its structure.
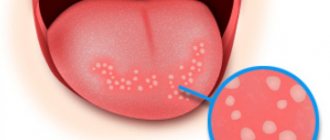
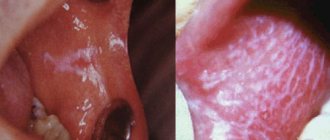
Types of traumatic stomatitis
Traumatic stomatitis can be conditionally classified according to the nature of damage to the mucous membrane and soft tissues of the mouth. All injuries are divided into three categories:
- Mechanical. They can be obtained as a result of falls, blows, or due to bad habits, such as biting the inner surfaces of the cheeks or lips, chewing hard objects, etc. In addition, the cause of traumatic stomatitis can be teeth with chipped parts, tartar, poorly fitting dentures or braces.
- Chemical. In children, chemical burns often occur when trying to taste any inedible substances. Among adult patients, traumatic stomatitis, provoked by chemical damage to the mucous membrane, can be caused by smoking and drinking alcohol.
- Physical. Such injuries most often occur as a result of a thermal burn. The risk of such damage is quite high at any age - all you have to do is sip too hot a drink or eat something scalding.
Statistics
Let's talk about venous tumors of venous etiology, which are the most common in the practice of a vascular surgeon. Let us immediately note that TU is not a diagnosis or an independent disease! This is a complication of the underlying vascular disease (most often, varicose veins), developing in the absence of adequate treatment. The difference between these particular ulcers is the minimal tendency to heal on their own. In most clinical observations, in the absence of radical correction of impaired blood flow, venous ulcers recur. In addition to physical suffering and a sharp decrease in quality of life, long-term non-healing venous leg ulcers also cause enormous financial damage. This is a colossal item of domestic healthcare expenditure. According to a number of researchers (S.N. Yakushkin, 2019), the costs of the vast majority of such patients for the purchase of medications (phlebotonics) and expensive dressings in Moscow exceed 50,000 rubles per year.
Trophic ulcer - treatment. Reviews from our patients.
Patient's review of laser treatment for trophic ulcers in our center.
Victor Petrovich, 65 years old.
I am a pensioner with a whole cartload of all sorts of ailments. My legs had been hurting and swollen for a long time, but I, like many, put off going to the doctor until later. I took some pills on the advice of a neighbor nurse, although I didn’t notice any particular improvement. In general, I lived to the point where I had a huge ulcer on my leg. God bless your doctors, I already thought that I would be left without a leg. They gave me laser treatment. I didn’t particularly delve into the nuances of this case; the doctors guaranteed a good result. Everything went without pain, literally after a few days my trophic ulcer began to disappear before my eyes, and after two weeks only a small scar remained. Of course, various medications were prescribed, then I went to a sanatorium and forgot about this terrible disease. Thanks to all the doctors of the Medical Center for Phlebology, especially Dr. Malakhov Alexey Mikhailovich.
A patient's review of the treatment of trophic ulcers using the EVLO method in our center.
Komissarova L.I.
Our patient with surgeon-phlebologist A.M. Malakhov. after treatment
My leg ached constantly, there was a buzzing sensation in it at the end of the day, and then a trophic ulcer formed, which became larger and larger. I didn’t dare to have surgery using the classical method, because I was afraid after reading reviews online and all sorts of complications. Well, my daughter is in the know, she found me an experienced doctor in Moscow, Alexey Mikhailovich Malakhov. Before the operation, and this is endovasal laser coagulation, at the medical center in Moscow, where I decided to have it, they did an ultrasound, donated blood and that’s it. After the operation, I was forced to get up from the table and walk for about an hour. After 3 weeks I saw my doctor. I didn’t worry about scars, the main thing was that the ulcer healed faster. It's been 3 months since the laser procedure on my leg. Everything is fine, the ulcer has become very small, but I hope it will heal completely soon.
I'm very glad that everything went well. Thanks for all. Komissarova Lyudmila Ivanovna, December 7, 2016
Symptoms
The development of TN is not a matter of one day, it occurs over a long period of time. Literally a few months before the formation of varicose veins, characteristic signs of progressive damage to the veins of the lower extremities appear. Against the background of pronounced varicose transformation, swelling and a feeling of heaviness in the calves intensify. Often the patient suffers from nighttime muscle cramps. Burning and itching may also occur; there is an increase in pigmentation, thickening of the skin of the lower leg, the so-called. cellulite. Due to hemosiderin accumulating in the skin, eczema and chronic dermatitis develop. The skin in this area atrophies and becomes as if varnished. On palpation, their thickening, immobility, tension, and pain are observed. Lymphostasis often develops, as a result of which small transparent droplets appear on the skin, even with apparently intact skin - this is lymphorrhea.
After a certain period of time, a whitish focus of skin atrophy appears. This is essentially a pre-ulcerative condition. The early stage of TU is characterized by the appearance of a bluish spot on the lower leg or foot. A minimal, unnoticeable injury received by a patient at home immediately triggers this process. Then a blister appears. Then it will become a superficial chronic wound, the width and depth of which will only increase over time instead of healing. The ulcer spreads not only in width, but also in depth. It may happen that several ulcers merge with each other. This creates a large defect.
When the ulcer penetrates into the deep layer of tissue, the patient experiences strong and sharp constant pain. TJ can involve its own fascia, nerve trunks, gastrocnemius muscle, Achilles tendon, and the surface of the tibia. If the soft tissues in the ankle joint are damaged, arthritis develops and contracture develops.
After a few years, the patient may even have a limb amputated due to the formation of extensive circular purulent-necrotic ulcers. The latter, being sharply painful, constantly bleed lymph and pus; become a source of electrolyte and protein losses. Against this background, erysipelas easily develops; there is a probability (3-5%) of malignant degeneration of periulcerous tissues. All this exhausts patients, depriving them of the opportunity to live a full life, go to work, and do what they love. Cases of family breakdown, depression and loneliness are common. To avoid all these consequences, it is necessary to promptly contact a qualified specialist who will examine and prescribe effective treatment.
Perforated ulcer of the stomach and duodenum
Perforation, or perforation, of stomach and duodenal ulcers is a breakthrough of the ulcer into the free abdominal cavity with the entry of gastroduodenal contents into it. In 75% of cases, a perforated ulcer is located in the duodenum, most often observed in men aged 20–40 years with a short history of ulcers (up to 3 years). Sometimes perforation of an ulcer can occur in people who have never previously complained of epigastric pain and were not aware of the presence of an ulcer. In young people, perforation of duodenal ulcers predominates, and in middle-aged and elderly people, perforation of gastric ulcers predominates. Perforation of ulcers is more often observed in autumn and spring.
Classification. By localization: a) stomach ulcers: lesser curvature (cardiac, antral, prepyloric, pyloric), anterior wall (antral, prepyloric, pyloric), posterior wall (antral, prepyloric, pyloric); b) duodenal ulcers: anterior wall, posterior wall. Along the flow: a) perforation into the free abdominal cavity, b) covered perforation, c) atypical perforation. There are 3 phases of the clinical course of a perforated ulcer: 1) the shock phase, 2) the phase of “imaginary well-being,” and 3) the phase of widespread peritonitis.
Etiology and pathogenesis. The main factor leading to the development of perforation is the exacerbation of peptic ulcer disease, when the processes of inflammation and destruction in the ulcer intensify, it deepens until the formation of a hole in the wall of the organ. Through this opening, the contents of the stomach and duodenum - gastric juice, air (gas bubble of the stomach), eaten food - enter the abdominal cavity. Hydrochloric acid from gastric juice suddenly entering the abdominal cavity causes a chemical burn of the peritoneum of the upper abdominal cavity (chemical peritonitis). In response, the peritoneum begins to produce fluid - exudate, which, diluting the acid, reduces its concentration and the strength of its irritating effect. At the same time, a large amount of biologically active substances are released into the blood, which determine the first clinical phase of the disease - the shock phase. The second phase - “imaginary well-being” - is due to the fact that gastric contents cease to flow into the abdominal cavity (most often due to clogging of the perforation with a lump of food). Acid diluted with exudate irritates the peritoneum less, and the pain receptors of the burned peritoneum become less sensitive. Subsequently, pathogenic microorganisms that enter the abdominal cavity from the stomach and infect the peritoneum begin to multiply, release toxins and cause the development of the third phase of the disease - widespread peritonitis.
Complaints. The main complaint when an ulcer perforates is pain in the upper abdomen. In most patients, perforation of stomach and duodenal ulcers begins suddenly, accompanied by sharp pain in the abdomen. The pain can be so severe that patients compare it to a “dagger blow.” They are permanent in nature, localized first in the epigastric region or in the right hypochondrium, and then spread relatively quickly throughout the abdomen, often along the right lateral canal. In 30-40% of patients, pain radiates to the shoulder, scapula or supraclavicular region: on the right - with perforation of pyloroduodenal ulcers, on the left - with gastric ulcers. When an ulcer perforates, general symptoms are also observed: dry mouth, thirst, nausea. In 30-40% of patients, reflex vomiting occurs, which becomes more frequent as peritonitis progresses.
Anamnesis. Before ulcer perforation, 80-90% of patients have a typical ulcer history or vague gastric complaints, against which perforation occurs. In 10-15% of patients, “without anamnesis” or “silent” perforated ulcers occur, when perforation is, as it were, the first symptom of a peptic ulcer. In 50-60% of patients, prodromal symptoms of perforation or exacerbation of peptic ulcer disease are observed (increased pain, general weakness, low-grade fever, nausea, vomiting).
Examination of the patient. The condition of the patients is serious. Pallor, cold extremities, and cold sweat on the face are noted. Breathing is frequent, shallow, the patient cannot take a deep breath. The pulse in the first hours after perforation is slow or normal, and with the development of peritonitis it becomes more frequent. Body temperature is initially normal or subfebrile, and later rises to 38 degrees. and more. There is also retention of stool and gas. The appearance of the patients is characteristic: they take a forced position on their back or side with their knees brought to their stomach, and avoid changing it. The facial expression is frightened, suffering.
Characteristic symptoms of perforation are revealed by objective examination. The abdomen is often scaphoidally retracted or flat and does not participate in the act of breathing. Tension of the muscles of the anterior abdominal wall is a very characteristic and constant symptom of a perforated ulcer. In this case, most patients experience a board-like tension in the abdominal muscles. It can cover the entire abdomen or its upper section. However, in elderly patients, sometimes muscle tension may not be pronounced. On palpation, in addition to muscle tension, sharp pain is noted, more in the upper abdomen, the Shchetkin-Blumberg symptom. Percussion often reveals a very important sign - “disappearance of hepatic dullness” or a decrease in its size as a result of the entry of free gas from the lumen of the stomach through the perforation into the abdominal cavity. In addition, a high-pitched tympanic sound (Spizharny's symptom) and dullness in the lateral parts of the abdomen may be detected in the epigastric region - due to the accumulation of liquid stomach contents there, poured out through the perforation, and exudate produced by the peritoneum in response to its sharp irritation with acidic gastric juice. Auscultation may reveal the absence of intestinal motility, listening to heart sounds up to the level of the navel (Gusten's symptom). Digital rectal examination may reveal sharp pain in the pouch of Douglas (Kulenkampf's sign).
The shock phase (up to 6 hours) is characterized by daggering, excruciating pain in the abdomen. The condition of the patients is serious, they are excited, pale, covered in cold sweat, and show fear and suffering. Breathing is frequent and shallow. The pain is localized in the epigastric region or right hypochondrium, and can radiate to the right shoulder and collarbone. Characteristic is “board-shaped” tension of the muscles of the anterior abdominal wall in the epigastrium. Percussion often detects the symptom of “disappearance of hepatic dullness.” Phase of “imaginary well-being” (6 – 12 hours). In this phase, the patient's condition improves. Abdominal pain and muscle tension in the anterior abdominal wall are reduced. Breathing becomes equal. The Shchetkin-Blumberg sign is positive in the epigastrium, the right half of the abdomen. Diagnostic errors most often occur in this phase. The phase of widespread peritonitis (more than 12 hours). The condition of the patients again deteriorates significantly. Bacterial purulent peritonitis develops. As a result of intoxication, the general condition worsens, body temperature rises to 38° or more, pulse quickens, blood pressure decreases, and bloating appears. Facial features become sharper, tongue is dry. The clinical picture of a perforated ulcer during this period does not differ from that of widespread peritonitis of another etiology.
Diagnostics. General blood analysis. Leukocytosis and a neutrophil shift in the leukocyte count to the left are observed.
Plain radiography of the abdomen. Free gas is detected in the abdominal cavity (pneumoperitoneum). On photographs with the patient in an upright position, it is revealed as a crescent-shaped clearing under the right, less often under the left, or both domes of the diaphragm. The most characteristic is a crescent-shaped clearing between the liver and the right dome of the diaphragm, that is, on the right. Pneumoperitoneum with perforation of an ulcer is found in 60-80% of patients and is a direct symptom of perforation, but its absence does not exclude a perforated ulcer.
Pneumogastrography. In the absence of pneumoperitoneum on a plain radiograph of the abdomen, 500–700 ml of air is introduced through a probe into the stomach after it has emptied, which partially passes through the perforation into the free abdominal cavity and is found under the diaphragm. Fibroesophagogastroduodenoscopy (FEGDS). During the procedure, you can detect a perforated ulcer, and after the procedure, you can detect free gas in the abdominal cavity.
Diagnostic laparoscopy. It is possible to detect the presence of exudate in the abdominal cavity, signs of inflammation of the peritoneum, and the perforation of the stomach or duodenum itself. Laparocentesis. During an abdominal puncture performed below the navel, the trocar stylet is directed to the right hypochondrium. After this, a 30-centimeter vinyl chloride tube is inserted, from which the exudate is aspirated. If there is any doubt about the nature of the exudate, the Neimark diagnostic test can be used. To perform this test, add 4-5 drops of 10% iodine tincture to 2-3 ml of exudate found in the abdominal cavity. If the liquid contains an admixture of gastric contents, then under the influence of iodine tincture it acquires a dark, dirty-blue color (due to starch residues). Diagnosis of “covered” perforation often presents significant difficulties. Free gas in the abdominal cavity in such patients is detected less frequently than with open perforation. In the diagnosis of this form of perforation, an ulcer history in the past, an acute onset of the disease, and two phases in the clinical course - pronounced perforation syndrome and extinction of clinical symptoms - are important.
Treatment. Patients with a perforated gastric or duodenal ulcer are subject to immediate hospitalization in the surgical department and emergency surgery. Possible options for operations: Suturing the ulcer with a single-row suture in the transverse direction with application of a greater omentum. Suturing the ulcer according to Opel-Polikarpov (with tamponade of the perforated hole with a strand of the greater omentum). In this case, a strand of the greater omentum is inserted into the perforated hole, and then, using interrupted sutures in the transverse direction, the edges of the perforation hole and the strand of the greater omentum inserted and stitched into it are tightly brought together. Gastric resection is performed rarely, according to strict indications and taking into account contraindications. Operations for perforated ulcers are necessarily accompanied by thorough sanitation of the abdominal cavity, removal of exudate and spilled gastric contents from the abdominal cavity, drying and draining it. Suturing an ulcer when it perforates can be performed either openly or using laparoscopic techniques.
How dangerous is the pathological process with a trophic ulcer?
An open TU is always a potential source of pyogenic infection and a kind of “gate” through which pathogenic microorganisms easily penetrate. The risk of developing erysipelas, phlegmon, lymphadenitis, and sepsis increases many times over. If the pathological process is progressive in nature, and if anaerobic flora has been introduced into the affected area, even gas gangrene of the limb may develop. In addition, TU is a source of constant pain and general discomfort, which significantly reduces the patient’s quality of life. If a trophic ulcer does not heal for a long time and (or) an aggressive medicinal substance is used to eliminate it, malignancy of the cells may occur. This is how the patient is diagnosed with skin cancer.
Trophic ulcer - radiofrequency treatment (RFA, RFO)
The radiofrequency treatment method is considered the most modern and safe if you have a trophic ulcer. RFA treatment in Moscow involves heating the walls of the vein with microwaves, it “closes”, and the trophic ulcer gradually shrinks. RFO treatment - and after a few months the problem vein is a connective tissue cord, and the entire load is transferred to neighboring, healthy vessels. This is how the trophic ulcer gradually heals.
Treatment of trophic ulcers with radiofrequency (RFA, RFO) in our center
RFO treatment in Moscow is carried out quite quickly; the patient goes home 10 minutes after the intervention. The radio frequency method provides the following advantages:
- short duration of the procedure - 30-40 minutes;
- exposure parameters are selected automatically and without the participation of a doctor;
- cosmetic effect - the absence of additional trauma promotes the formation of a less rough scar where there was a trophic ulcer. RFA treatment is very positive in this regard.
- the procedure is completely painless and easily tolerated;
- Hospitalization is not required, the patient can lead a normal life, limiting activity only after the procedure.
Diagnostic measures
To diagnose a trophic ulcer, a doctor only needs to conduct a routine visual examination. It is much more important to identify what exactly caused its development.
Laboratory research
1. Submission of general and biochemical blood tests. The results of this analysis reveal an increased number of red blood cells, which makes the blood more viscous and impairs blood circulation. An increased number of leukocytes indicates the presence of an infection.
2. Coagulogram is a comprehensive blood test that allows you to evaluate its coagulation ability, as well as the biochemical systems responsible for the balance of coagulation and fibrinolysis
3. Bacteriological study. A smear from the affected area will help determine whether there are pathogenic bacteria, their type, the level of microbial contamination of the lesion, and the sensitivity of bacteria to antibiotics in order to select appropriate antibacterial therapy.
4. Histological examination. A very important test that allows you to exclude oncological pathology and assess the depth and extent of microscopic changes
5. Rheumatic tests. Especially in young patients and in unclear clinical situations, the analysis determines the autoimmune process due to which the connective tissue is affected. As is known, autoimmune disease also contributes to damage to the bloodstream.
Instrumental research methods
After a conversation with the patient and a routine examination, an ultrasound duplex angioscanning of the veins of the lower extremities is mandatory. At the same time, the patency of deep and subcutaneous venous vessels, the severity and extent of reflux, as well as the condition of the perforating veins of the leg are assessed. Ideally, the ultrasound is performed by the vascular surgeon himself. Thus, the information content and diagnostic value of the technology significantly increases. This is evidenced by personal long-term clinical experience. In parallel, we can always evaluate the patency of the main arteries, which plays an important role in choosing the optimal treatment. Ultrasound is accessible, low cost, simple, and non-invasive.
MSCT angiography. It is a special CT method that will help to study in detail the bloodstream along its entire length. In 3D mode (the so-called “virtual angioscopy”), a detailed study is carried out of the condition of the blood vessels, and any structural change in the arterial and venous walls is revealed. The technique is especially indispensable for high occlusions of the venous bed, lymph circulation disorders, various anomalies in the structure of veins and vascular malformations. It should be noted that MSCT angiography is unsafe for health, since it is associated with a high radiation dose, which limits the frequency of use.
Magnetic resonance imaging (MRI angiography). The modern high-tech method is expensive, but provides more accurate and detailed information. It reveals the condition of the internal organs and soft tissues, as well as the vascular bed, and how they function. It is not associated with ionizing radiation, since it has a completely different physical nature.
Laser Doppler flowmetry. Detects the slightest disturbance in the microcirculation of the wound area. This rather labor-intensive technology has not yet received general clinical application.
Treatment of traumatic stomatitis
The choice of treatment tactics for traumatic stomatitis is largely determined by the nature of the damage that caused the inflammation. Therefore, first of all, the specialists of the Doka-Dent clinic eliminate the traumatic factor:
- Irritating dentures and braces are adjusted or remade;
- if the cause of traumatic stomatitis is a broken tooth, it is treated and restored;
- Tartar deposits are removed with professional cleaning.
Then the dentist proceeds directly to the treatment of traumatic stomatitis. If there are minor injuries, the wounds are washed with antiseptics. More serious lesions are anesthetized and then treated with anti-inflammatory drugs. If the wound is penetrating and deep enough, stitches may be required.
Further treatment of traumatic stomatitis is carried out mainly at home. The doctor prescribes various products for rinsing, applications and other procedures that should ensure the speedy healing of ulcers, erosions and wounds. In addition, the clinic specialist gives the patient the necessary recommendations that will help avoid relapses. Then a date for a follow-up appointment is set, at which the doctor will assess the success of the treatment.
General rules during treatment
1. Conscientiously follow medical prescriptions;
2. If possible, prevent the increase in swelling of the tissues of the lower leg and foot. To remove excess fluid from the body, you need to:
- follow a certain diet, that is, do not eat salty, fatty foods. Maximum salt restriction.
- Make sure that the daily urine output matches the amount of fluid you drink.
- In relatively rare cases, taking diuretics is allowed. Which medicine should be agreed with your doctor. This should only be used as an aid, and not the main method of getting rid of edema (!).
- Use compression garments. The compression class and type of knitwear (stockings, knee socks) depend on the severity of hemodynamic disturbances in the veins of the affected limb. As a rule, in this situation, compression stockings of classes II-III are prescribed. It is allowed to wear a special anti-ulcer kit from well-known manufacturers. ULCER X (Sigvaris, Switzerland) with a working pressure in the lower leg of about 34-46 mm Hg is ideal;
3. Normalizing body weight is a fundamental task that we usually immediately set for a patient with venous TU. It is known that with excess weight there is an increase in the likelihood that a trophic ulcer will appear, and the prognosis for its treatment worsens. With normal weight, there is no overload of the venous bed or disruption of the venous outflow of blood. When reaching optimal weight, a person must make every effort to maintain these indicators;
4. Completely give up bad habits that impair blood circulation. That is, do not smoke, do not drink alcohol, etc.;
5. Do not overcool your feet; buy soft, comfortable shoes. The ideal option is semi-sports shoes with laces (imitation of elastic compression) plus individual orthopedic insoles. It is preferable that it be made from natural materials. All this, in combination with compression hosiery, optimizes the work of the muscle pump of the lower leg and foot;
6. If the localization of the ulcerative defect is the sole of the foot or toes, the patient is recommended to use a special splint or specially selected relief shoes. Thanks to this, the risk of injury and anaerobic infection is reduced. While walking, a person uses a stick or crutches. This reduces the load on the affected area;
7. Carefully observe hygiene measures. A warm, hygienic shower is mandatory for patients with TU. Liquid neutral soap with an antibacterial component is recommended. It is mandatory to regularly clean the affected area and the ulcer itself using modern antiseptics (lavasept, octenisept, meramistin). Thus, wetting the feet is permitted. Otherwise, the likelihood of developing a dried purulent crust increases, which, in turn, is a springboard for pathogenic microorganisms. The product that the patient will use to treat the affected area should be prescribed exclusively by the treating specialist. You should purchase the treatment drug only at specialized pharmacies.
Features of treatment
If a patient has a trophic ulcer, it is necessary, first of all, to identify what is the root cause of the pathology. Before starting treatment, the patient should consult with a dermatologist, endocrinologist and therapist.
As world experience and data from numerous studies have shown, varicose trophic ulcers are difficult to treat without surgical correction of venous hemodynamics in the affected limb. Conservative therapy in itself, although considered the basis of complex treatment, does not guarantee against relapses of TU, and the resulting effect is unstable.
Competent surgical intervention using modern minimally invasive endovascular technologies can in many cases save the patient from severe suffering and achieve spontaneous healing of an ulcer on the lower limb. Endovasal laser coagulation today is the gold standard for surgical treatment of complicated varicose veins of the lower extremities. Performed in the so-called mode. "office surgery" under local anesthesia. Helps quickly eliminate venous reflux, normalize venous blood flow in the saphenous veins and create ideal conditions for self-healing of small ulcerative defects. Larger TUs require additional support (dermatomal autodermoplasty, shave therapy, etc.). Despite more than 20 years of experience in successfully performing classical phlebectomies (“open”, incisional interventions), and technically the most complex ones, I would like to note that we have already completely abandoned their implementation due to the traumatic nature, severe postoperative pain syndrome, long rehabilitation period, and also the risk of wound complications (wound suppuration, lymphorrhea, seroma, etc.). Previously, traditional intervention was performed only after the ulcer had healed and the patient’s general condition had normalized. Currently, it is possible to eliminate venous reflux (using EVLT) under local anesthesia (without hospitalization of the patient in a hospital), even on an “open” trophic ulcer.
For further treatment of a trophic ulcer, the patient is prescribed angioprotectors and disaggregants, as well as a number of wound dressings and ointments that help accelerate tissue regeneration. Topical agents are prescribed strictly taking into account the phase of the wound process, the severity of perifocal inflammation and the condition of the skin. Drug and surgical treatment can be supplemented with various physical procedures.
Trophic ulcer, stages or course options
The size of the trophic ulcer directly depends on the lack of blood supply and the duration of the pathological process. Usually the ulcerative surface occupies no more than 35 cm2. If left untreated, it can cover the entire lower leg and reach 100 cm2. Treatment methods for trophic ulcers must be correct, competent and qualified: no poultices or tinctures!
Stages of appearance of a trophic ulcer
The initial stage (small bleeding ulcer) is complicated by the addition of a bacterial and fungal infection. Purulent contents with an unpleasant odor begin to separate from the ulcer. The longer the process, the deeper the layers are subject to inflammation and rotting. The ulcerative lesion spreads to the calf muscles, involving the ankle joint in the inflammatory process. In advanced cases, the development of pyoderma, phlegmon and sepsis is possible.
It is worth distinguishing between venous and arterial trophic ulcers. The former occur in patients of any age, while arterial ulcers are a disease that occurs exclusively in old age, caused by atherosclerosis of the artery walls.