Every person has had an inflamed gum at least once in their life. This usually occurs due to brushing too aggressively, using a hard toothbrush, putting too much pressure on the soft tissue of the floss, or eating very hard foods. If the causative factor is eliminated, the gums quickly heal and the inflammation goes away. But there are situations when the gums near the crown of the tooth become inflamed, but there were no obvious reasons provoking this condition. In this case, you need the help of a dentist.
general characteristics
The pain is caused by changes in the gums and periodontium, which occur under the influence of local factors: poor oral hygiene, the presence of tartar, functional periodontal insufficiency due to a decrease in chewing load when eating too soft food.
Smoking plays a significant role. Common factors affecting the condition of oral tissues are gastrointestinal diseases, infectious and endocrine pathologies, natural changes in hormone levels, and harmful occupational exposures. The listed reasons entail the formation of an environment favorable for the activity of pathogenic microorganisms, the development of inflammation, disruption of the local blood supply and nutrition of the gums, and changes in its structure. The result is a pain syndrome. Often the periodontium is involved in the pathological process, the disease becomes chronic, leading to gross local changes and tooth loss.
What complications can there be?
In the absence of timely treatment, the disease can lead to complications:
- An abscess is a purulent inflammation of tissue (if there was no pus during inflammation before).
- Phlegmon is an acute purulent inflammation of the subcutaneous tissue and connective tissue.
- Osteomyelitis is a purulent-necrotic process that develops in the bone and surrounding soft tissues.
- Periodontitis is inflammation of the periodontium, i.e. all tissues adjacent to the tooth.
In particularly severe cases, blood poisoning may occur (for example, if an abscess breaks).
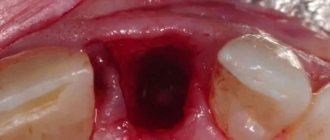
Abscess is one of the possible complications
Why do my gums hurt?
Gingivitis
May be local or widespread. It manifests itself as pain, swelling, redness, increased local temperature, bleeding, and the formation of pinpoint hemorrhages or areas of ulceration. Hypersalivation is observed. The clinical picture varies slightly depending on the type of gingivitis:
- Catarrhal.
The pain is minor and occurs upon contact with food. The main symptoms are pronounced signs of inflammation and gum sensitivity to temperature changes. The general condition is not disturbed. - Ulcerative-necrotic.
Against the background of the formation of areas of necrosis and ulceration, the gums become sharply painful. Eating is difficult. The breath is foul. There is a deterioration in the general condition: weakness, weakness, low-grade or febrile temperature. - Hypertrophic.
It is asymptomatic for a long time and is discovered accidentally during dental examinations. Subsequently, in the absence of treatment, pain in the gums gradually progresses due to touching and eating. Severe discomfort when brushing teeth forces patients to refuse this procedure, which further worsens the condition of the oral cavity. - Desquamative.
It occurs more often in women during menopause and is caused by a decrease in the number of keratin-containing cells and an increase in mucosal permeability. It manifests itself as soreness and bleeding of the gums even with weak influences.
Periodontal disease
The basis of the disease is periodontal atrophy with loosening of the gums, destruction of the periodontal joints, penetration of plaque into them and subsequent tissue damage. As a result, the gums begin to bleed. Pain appears when exposed to any irritant. Against the background of periodontal disease, recurrent inflammatory processes develop. The pathology can be primary, but is more often diagnosed in patients with hypovitaminosis, diseases of the digestive tract, cardiovascular and endocrine systems.
Gum pain
Periodontitis
The cause of periodontal damage is dental plaque, which transforms into tartar. Pain during periodontitis is rarely observed, mainly at the initial stage, with inflammation of the gums (gingivitis). Subsequently, redness, bleeding, swelling, and local hyperthermia predominate. There is an increase in sensitivity to the action of irritants, which some patients interpret as minor pain.
As in the previous case, the disease can develop primarily, but is more often detected against the background of other pathologies. Periodontitis in diabetes mellitus is particularly persistent. The disease develops or progresses rapidly during pregnancy, breastfeeding and menopause, especially if there is a history of gingivitis. It is observed in endemic goiter and Itsenko-Cushing's disease.
Stomatitis
Pain in the gums is most characteristic of Vincent's stomatitis. Soreness and bleeding gums become the first symptoms of the disease. This is explained by the fact that the pathological process begins from the gingival margin, and only then spreads to other areas of the mucosa. Subsequently, erosions and ulcers appear. There is a putrid odor from the mouth and low-grade fever.
With other types of pathology, the presence or absence of pain in the gum area is determined by the affected area. In patients with ulcerative stomatitis, the symptom is observed when the defects are located near the edge of the gums and the inflammatory process spreads to nearby tissues. Manifestations are especially pronounced in the presence of severe somatic diseases and in childhood.
Malocclusion
Pain in the gums due to malocclusion develops against the background of the dental pathologies listed above (periodontal disease, periodontitis, etc.), which are secondary in nature and arise as a result of impaired contact between teeth, improper distribution of the chewing load and chronic trauma. The symptom is observed in some patients with deep and crossbites. Can occur in distal and mesial occlusions.
Mechanical damage
Gum injury can be acute or chronic. Acute injuries are the result of accidents at home (for example, a blow or fall), scratches from hard pieces of food (a fish bone, the edge of a bitten nut) or medical instruments during dental procedures. The pain is local, sometimes accompanied by bleeding or hemorrhage. They disappear after a few days. Chronic injuries are associated with poor fitting dentures. The pain is not intense, persists for a long time, intensifies while eating.
Allergic reactions
Allergy to prosthetic materials is usually a type of stomatitis (allergic contact stomatitis). Along with pain when eating food, it is manifested by dryness, burning and the presence of a metallic taste in the mouth. It can develop many months or even years after the installation of dentures. It is combined with swelling of the mucous membranes of the cheeks, soft palate and tongue, burning sensation in the tongue, and disturbances in taste sensitivity.
What will the dentist do if the gums become inflamed after installing a crown?
First of all, the doctor will order an X-ray to determine the cause of inflammation of the gums under the crown. Treatment by the dentist will also be selected based on this information.
Most often in these cases it is necessary to remove the crown. Additionally, patients are prescribed anti-inflammatory treatment and antibiotics. It is possible to re-prosthetize a tooth after the gums have become inflamed only when the anti-inflammatory treatment has ended. And only then will a new crown be installed.
It is important to understand that folk remedies will not be effective in this case and will not replace seeing a doctor. If you realize that discomfort continues for more than three days, be sure to consult a doctor. Inflammation is a serious process that affects the body as a whole, so it is important to recognize the cause as early as possible and determine effective treatments for inflammation.
Diagnostics
A dentist will determine the cause of pain in the gums. A dental examination involves assessing oral hygiene, studying the condition of soft tissues, identifying signs of inflammation and mucosal defects, determining the presence and severity of periodontal pockets and tooth mobility. As part of the additional examination, the following procedures are prescribed:
- Radiography.
In inflammatory periodontal diseases, osteoporosis is visible in the photographs. Horizontal destruction indicates a chronic course of the pathology, vertical destruction indicates the formation of abscesses. With periodontal disease, osteoporosis is combined with sclerotic changes. Based on the results of radiovisiography or orthopantomography, the type and severity of malocclusion is assessed. - Bacteriological or bacterioscopic examination
. Performed for Vincent's stomatitis and inflammatory periodontal diseases. This type of stomatitis is characterized by a large number of Borrelia Vincent. In other cases, various types of pathogenic bacteria are found, less often fungi. - Other laboratory tests
. The inflammatory process is accompanied by leukocytosis and an increase in ESR in the general blood test. If an allergy is suspected, intradermal, scarification, cutaneous drip, exposure and elimination allergy tests are performed.
Dental examination
Does it make sense to treat wisdom teeth?
An experienced and self-respecting dentist will always fight for every tooth to the last. And wisdom teeth in this case are no exception. After all, no one knows how the patient’s life will turn out in the future. Perhaps in the future he will need prosthetics, and the figure eight will be used as a supporting tooth for installing a prosthesis. Therefore, if the appearance of a third molar does not pose a threat to neighboring teeth and oral health, the dentist will take actions aimed at facilitating the process and preserving the tooth. Well, unless, of course, the patient insists on its removal.
If the current situation is serious, then removal of the wisdom tooth is inevitable. Including in those cases when the figure eight does not hurt much (or does not hurt at all), but is covered with caries and is gradually destroyed. It is more rational and safer to remove such a tooth and forget about the problems.
Treatment
Conservative therapy
Mandatory measures for pathologies accompanied by pain in the gums are professional oral hygiene and treatment of carious teeth. In case of allergies or mechanical injuries due to errors in the installation of prostheses, repeated prosthetics or correction of structures is necessary. Patients with malocclusion undergo orthodontic treatment. Depending on the nature of the disease, therapeutic regimens may include:
- Gingivitis
. Means for improving local immunity are indicated. After eating, it is recommended to rinse your mouth with herbal decoctions and antiseptic solutions. For intense pain, analgesics are prescribed. - Periodontal diseases
. Antibiotics and anti-inflammatory drugs are used for periodontitis. In case of periodontal disease, electrophoresis, hydro- and vacuum therapy are used to improve local blood supply. Movable teeth are fixed with temporary splints. - Vincent's stomatitis
. As part of local treatment, local anesthetics, sorbents, and drugs with proteolytic, antimicrobial and antiprotozoal effects are applied. At the resolution stage, keratoplasties are effective, accelerating tissue restoration. Common medications include antibiotics, NSAIDs, antihistamines, antipyretics, and painkillers.
How to relieve acute gum inflammation?
Each form of the inflammatory process requires separate therapeutic measures. For example, inflamed gums with gingivitis should adhere to the following algorithm:
- Clean teeth from tartar and plaque.
- Take a course of anti-inflammatory drugs: rinsing with a 0.05% chlorhexidine solution or compresses with Cholisal-gel.
- In the future, special toothpastes should be used to clean your teeth: Lakalut or Parodontax. You need to develop the habit of using dental floss to thoroughly clean the space between your teeth.
In addition, inflamed gums can be treated with traditional medicine: for example, herbal decoctions (chamomile, calendula or oak bark). However, it is important to understand that their effect is weaker, and if the gums are already swollen, and purulent discharge appears above or below the tooth, folk remedies for treatment will not be enough.
Content:
- Why does the gum around the wisdom tooth hurt? 1.1. Pain due to wisdom tooth cutting 1.2. Pericoronitis as a cause of pain 1.3. Dental neck caries 1.4. Other reasons
- Signs of inflammation
- What to do at home
- Treatment
- How to avoid inflammation
If your gums near your wisdom tooth hurt, you need to visit a dentist and undergo a prescribed examination. Self-medication for painful symptoms is usually ineffective, since it is not possible to establish the true cause of the disorder. Consequently, all measures taken will be aimed exclusively at relieving the unpleasant symptom.