From this article you will learn:
- what is oral candidiasis,
- what does thrush look like on the tongue in adults,
- effective tablets against thrush,
- causes of thrush in the mouth of a baby.
Thrush in the mouth is a type of fungal infection in which the oral mucosa is affected by yeast-like fungi of the genus Candida (primarily the species Candida albicans). The main symptom of thrush is the appearance on the mucous membrane of a whitish coating in the form of flakes, reminiscent of snow or cottage cheese flakes. Thrush can occur on the mucous membrane of the tongue, cheeks, hard and soft palate, tonsils, palatine arches, and also in the corners of the mouth.
The term “thrush” is only a colloquial expression, and in dentistry, the professional term used to refer to this disease is oral candidiasis. Most often, this disease develops against the background of reduced immunity, and equally in both men and women. Candidiasis in the mouth can also develop in infants, and most often this occurs at 4 weeks from birth (rarely at 1 week, or in children older than 6 months).
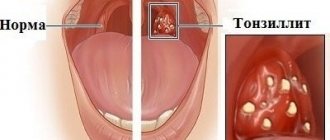
Thrush in the mouth: photo
It is important to understand that thrush in the mouth in adults or infants is not some banal fungal infection of the mucous membrane that can be “caught” somewhere and then easily cured. Fungi of the genus Candida are “opportunistic microorganisms” and cause oral infections only if the “host” has a predisposing condition. Those. yeast-like fungi are part of the normal microflora of the human oral cavity, never showing their pathogenic properties in most cases.
And if oral candidiasis does occur, most often this is a marker of serious (not yet diagnosed) diseases, pathologies of the immune system. If before 1980, thrush in the mouth occurred mainly only in either very young or elderly patients, now due to the widespread prevalence of immunodeficiency conditions (diabetes, leukemia, HIV/AIDS), due to the widespread use of immune-suppressing drugs drugs - candidiasis is typical for any age.
Oral candidiasis: what is it?
A fungus of the genus Candida can settle on the lining of the mouth, which causes a disease called candidiasis, or oral thrush.
With this disease, white plaques appear on the tongue and inner surface of the cheeks. They may cause pain and even slight bleeding when brushing your tongue. Without treatment, candidiasis can spread to other areas of the mouth, such as the back of the throat, tonsils, gums and palate. Although no one is immune to oral thrush, the disease is more common in people with weakened immune systems, denture wearers, patients taking inhaled corticosteroids, and infants. Oral thrush also occurs in people undergoing chemotherapy or radiotherapy, patients with a history of dry mouth syndrome (xerostomia), and smokers.
Symptoms of candidiasis
The disease is widespread. Pathogens of candidiasis have been found in the air, soil, vegetables, fruits, and confectionery products. Yeast-like fungi are found as saprophytes on healthy skin and mucous membranes.
Manifestations of candidiasis, and therefore symptoms and signs, depend on the location of the source of the disease.
Candidiasis of the oral mucosa (oral candidiasis, infantile thrush) most often occurs in children; as a rule, they become infected from the mother through the birth canal. Symptoms:
- the mucous membranes of the cheeks, pharynx, tongue and gums become red,
- swelling appears,
- then pockets of white cheesy plaque appear on the oral mucosa.
With candidiasis of the skin and its appendages, the lesions are most often located in large folds:
- inguinal-femoral,
- intergluteal,
- armpits,
- under the mammary glands.
The skin in the interdigital folds may be affected, more often in children and adults suffering from serious illnesses - on the skin of the palms, feet, smooth skin of the torso and limbs. Lesions in large folds look like small 1-2 mm bubbles, which soon open to form erosions. Erosion increases in size and merges, forming large areas of damage.
Foci of candidiasis have an irregular shape, dark red color, and around the lesion there is a strip of exfoliating epidermis. Outside the folds, the lesions look like red spots with peeling in the center, and occasionally small blisters may appear around the lesion.
Vaginal candidiasis (candidiasis, thrush) is an infectious disease of the vaginal mucosa, which often spreads to the neck of the uterus and vulva. Almost every woman has encountered this disease, and some signs of candidiasis are constantly disturbing. Most often occurs in women of reproductive age, but can occur in girls
Intestinal candidiasis (dysbacteriosis) often accompanies vaginal candidiasis or develops in isolation. Typically, intestinal candidiasis appears after taking antibiotics or previous intestinal infections. Fungi of the genus Candida settle in the small intestine. Symptoms characteristic of this type of candidiasis: white curdled flakes are often found in the stool of a patient suffering from intestinal candidiasis.
Esophageal candidiasis is a disease that is very difficult to identify among all those available in the field of gastroenterology. The disease is characterized by a discrepancy between the severity of the disease, the level of damage and the condition of the patient himself.
Causes of development of oral candidiasis
A number of very specific factors contribute to the occurrence of oral thrush. The causes of the disease can be either a weakening of the immune system (caused by illness or the use of certain drugs), or the use of antibiotics, which changes the natural microbial balance in the human body.
The result of failures in the functioning of natural defense mechanisms can be a significant imbalance in the balance of “beneficial” and “harmful” microbes. Under normal circumstances, the immune system fights viruses and bacteria that are dangerous to humans, but when the immune system is weakened, this fight becomes less effective, which allows the fungus that causes oral candidiasis to multiply.
Vaginal yeast infections, diabetes, most forms of cancer, HIV/AIDS - all of these diseases weaken the body and make it more vulnerable to oral thrush.
Anti-thrush medications –
We have already said above that oral candidiasis is increasingly rarely caused by the subspecies Candida albicans, which responds quite well to antifungal therapy.
Increasingly, patients are being inoculated with the most pathogenic aggressive species of fungi of the genus Candida - such as C.glabrata, C.krusei and C.tropicalis, which not only show resistance to many antifungal drugs, but also more often create microbial associations with other microorganisms (staphylococci, streptococci and etc.). All this complicates the treatment of oral thrush and also contributes to the development of relapses. Therefore, the most important thing to do before treating oral thrush in adults is to conduct a cytological examination. It will not only confirm the diagnosis of “oral candidiasis,” but also determine the sensitivity of Candida fungi isolated from a particular patient to the main antifungal drugs. It is systemic antifungal drugs that will be the basis for the treatment of oral candidiasis - especially severe and moderate forms. Treatment of mild primary forms of the disease can be carried out using topical agents.
Oral candidiasis in adults with weakened immune systems
Oral candidiasis can spread to other organs - the lungs, liver and digestive tract. When an infection enters the intestines, it may disrupt its functioning and further weaken the body.
Depending on the severity of the disease, you may be prescribed antifungal medications, which come in the form of tablets, lozenges, and a mouthwash that you swallow. Amphotericin B, which is often used to treat advanced HIV and antifungal-resistant infections, may also be prescribed.
Because some antifungal medications can damage the liver, your doctor will likely do regular blood tests and monitor the condition of your liver (especially if it is already affected by an infection). The same strategy should also be applied if long-term treatment is expected or if you have liver disease.
Intestinal candidiasis. Therapy
Therapeutic approaches to the treatment of gastrointestinal dysbiosis with overgrowth of Candida fungi include the following:
- A balanced diet excluding sugar and the consumption of complex carbohydrates, foods with prebiotic properties, and probiotic foods.
- Antifungal drugs.
2.1.Polyene antibiotics (nystatin, natamycin, levorin).
- Nystatin is most appropriate to use in the presence of candida in the esophagus, stomach and is practically ineffective when candida is localized in the intestine, which makes it also not effective when administered prophylactically along with antibiotic treatment.
- Pimafucin (natamycin) is the most effective drug for overgrowth of Candida in the intestines. The drug has an antifungal (fungicidal) effect. Interacts with sterols in fungal cell membranes, disrupting their structure and function and causing their death. Active against many pathogenic yeast fungi, especially Candida albicans. No resistance to natamycin was observed. For intestinal candidiasis, 1 tablet is prescribed. 4 times a day after meals for 7-10 days.
2.2. Triazole derivatives (flucanazole, Diflazon, Diflucan, Mikosist, Flucostat, rumicosis, intraconazole, terbizil, etc.), caspofungin derivatives - Cancidas (for administration of the drug), Noxafil (posaconazole) suspension for oral administration.
2.3. MPH (copper derivative of chlorophyll) is a plant antiseptic from brown algae, a natural immunomodulator due to stimulation of phagocytosis and the activity of copper cations, enhanced by the influence of alcohol, has a bactericidal effect against staphylococci, streptococci, pneumococci, fungi, putrefactive bacteria and E. coli and an antiviral effect. MPH protects and stimulates hematopoiesis, the anti-inflammatory effect is due to an excellent complex of microelements. Prescribed by a doctor orally, 1 drop per 5 kg of body weight daily in a small amount of water. The course of treatment is 30 days,
2.4. Citrosept is a herbal antimicrobial agent made from grapefruit seed extract, which has a bactericidal effect, including. and against fungi of the genus Candida and Helicobacteriosis of the stomach, promotes the absorption of vitamin C, contains bioflavonoids that strengthen the vascular wall of capillaries and prevent blood clots and cholesterol plaques, stimulates the body's natural resistance. It is prescribed as drops diluted in water or juice in different dosage regimens depending on the disease.
2.5. Self-eliminating bacillary preparations (B subtilis, L.bulgaricus) - Flonivin-IS, Baktisubtil, Sporobacterin, biosporin, Baktisporin, Gastrofarm, etc.
2.6. Saccharomyces boulardi - Enterol, 1 capsule contains 250 mg Saccharomyces boulardi, suppresses the growth of opportunistic flora and fungi Candida Krusei, Candida pseudotropical
2.7. Probiotics – lactose-containing preparations (Lactobacterin, Gastrofarm, Primadophyllus, Acidophyllus, Narine, etc.)
- Enterosorbents.
- Hepatoprotectors (Heptral, Hofitol, Karsil, milk thistle preparations, Floravit, etc.)
- Immunomodulatory drugs (Kipferon, Polyoxidonium, Dopolan, Marispan, etc.)
Symptoms of oral thrush in children and adults
In some cases, symptoms of oral candidiasis may not appear immediately: sometimes they can appear completely unexpectedly. Here are some telltale signs that you may have oral thrush:
- White, curdled plaques in any part of the mouth
- Unusual pain with normal movements of the tongue and jaw
- Plaques bleed when rubbed
- Cracks and redness in the corners of the lips (more often when wearing dentures)
- Dry mouth
- Marked loss of sense of taste when eating or drinking
Although thrush most often develops in the most easily visible areas of the mouth, lesions can also occur in the esophagus. This makes it difficult to swallow or a feeling that food is stuck in the throat. This occurs in the most severe cases, and if you have any of these symptoms, you should contact your dentist or GP immediately.
While waiting for treatment, you can relieve pain, if any, on your own. Eat unsweetened yogurt or take probiotics containing lactobacillus acidophilus. Neither one nor the other is a medicine in the literal sense of the word, but it can help restore normal microflora. If the infection persists, your doctor will likely prescribe you to take an antifungal or antibiotic.
Symptoms of oral candidiasis in infants and nursing mothers
If you have oral thrush, your baby may have difficulty feeding or become fussier and more irritable than before. The manifestation of thrush will most likely be white plaques in the child’s mouth. Mothers should closely monitor their baby's oral health because candidiasis is transmitted through breastfeeding, and if this happens and the baby recovers, the mother may inadvertently infect him again.
As a breastfeeding mother, look out for the following signs and symptoms:
- Itchy, tender, or unusually red nipples
- Shiny or peeling skin around the alveoli
- Unusual pain during or between feedings
- Severe, stabbing chest pain
If white plaques appear in your or your child's mouth, contact your doctor or dentist immediately. Do not delay a visit to the doctor if symptoms of candidiasis occur in older children or adolescents, since the underlying disease against which thrush developed may be diabetes.
Because there are two people to treat at once, your doctor may use a special strategy, such as prescribing two different antifungal medications to begin with: a cream for your breasts and a different medication for your baby.
If you are breastfeeding, use breastfeeding pads to prevent fungus from getting on your clothes. Do not buy liners with plastic membranes, as they will only encourage the growth of fungus. Reusable pads (and, of course, the bra itself) should be washed in hot water and bleach to help prevent infection from spreading.
If you not only breastfeed your baby, but also bottle-feed him, and also give him a pacifier, wash all items that come into contact with the baby’s mouth every day in a solution of equal parts water and vinegar. After washing, allow items to air dry to prevent fungus from growing. All parts of the breast pump need to be treated in the same way, especially its removable parts.
Important points in the treatment of oral candidiasis -
There are several problems in treating candidiasis of any location. The first problem is that fungi of the genus Candida can be located not only on the surface of epithelial cells of the mucous membrane, but are also capable of germinating inside epithelial cells. In this case, the mucopolysaccharide membrane of the host cell will protect the fungi not only from phagocytes (which must find, absorb and digest infectious agents), but also, to a certain extent, from antifungal drugs. In this case, higher dosages of drugs and longer courses of treatment (including suppressive therapy) may be required.
Another problem may be an insufficient immune response (for example, incomplete phagocytosis of Candida fungi). In the absence of immunocorrection with the help of immunomodulators, this sharply increases the risk of developing chronic candidiasis and subsequent relapses. Among the immunomodulators, we can recommend the prescription drug "Cycloferon" (in the form of intramuscular injections), but it should be used only after the recommendation of a doctor. If a slight correction of the immune status is necessary, you can use Cycloferon tablets.
It is very important to carry out treatment while sanitation of the oral cavity, i.e. it is necessary to cure all carious teeth, foci of chronic inflammation in the oral cavity, and remove dental deposits. If soft microbial plaque and hard dental deposits have not been removed, this means that a new relapse of oral candidiasis will occur very soon. In addition, for patients with removable dentures, it is important to teach them to regularly disinfect dentures, as well as replace them if their service life has expired. It will be futile to treat oral candidiasis in patients whose dentures continue to be a source of infection.
For smokers, it is very important to reduce the frequency of nicotine consumption in this case, or better yet, give it up. If candidiasis occurs during the use of inhaled steroids (in asthmatics), the patient should be told about the need to rinse the mouth with water after spraying the steroid. During treatment, it is also very important to reduce the amount of carbohydrates consumed, and it is advisable to completely give up sweets and sugar-containing drinks. For patients with dry mouth, it is important to start using special medications to keep the oral mucosa hydrated.
Toothpastes containing lactoferrin, lactoperoxidase, lysozyme, and glucose oxidase can be of great help in the treatment and prevention of candidiasis and stomatitis. Such pastes increase local immunity in the oral cavity and reduce the risk of developing stomatitis and candidiasis. For example, such pastes are included in the SPLAT line of toothpastes.
Consultation with a therapist or dentist
If you suspect that you have an oral disease that requires medical supervision, make a list of all the symptoms you have, including those that may seem unrelated to thrush: the doctor will understand whether they are important or not. Include non-medical factors in this list, such as increased stress levels and causes of anxiety. Indicate whether you are around people with weakened immune systems.
You will also need to prepare a list of all medications you take. Also, write down questions you want to ask your doctor. This will help you find out all the details you are interested in and get a comprehensive consultation, regardless of whether you have oral candidiasis or not.
The doctor may ask you clarifying questions that will allow him to narrow down the search for a diagnosis based on the symptoms he has identified and the symptoms you describe. Try to answer as openly and honestly as possible so that the doctor can quickly diagnose the disease and begin treatment without waiting for complications.
If an examination of the oral cavity does not allow the doctor to make an accurate diagnosis, he will definitely take a small sample and either examine it himself or send it to a laboratory for analysis.
If the infection has already affected not only the oral cavity, but also the esophagus, a couple of studies may be required. First, your doctor will take a swab from the back of your throat to determine what bacteria or fungi are causing your symptoms. You may then have an endoscopic examination, in which your doctor uses an endoscope (a flexible tube with a light) to look at your esophagus, stomach, and upper small intestine. This will determine how far the infection has spread.
Lifestyle and Home Remedies for Oral Thrush
At the initial stage of candidiasis, good oral hygiene will help contain the development of the disease - brushing your teeth twice a day and at least daily use of dental floss will contribute to the timely removal of food debris and plaque from the surface of the teeth, from the interdental spaces and along the gum line. Instead of regular mouthwash, use a solution that requires a teaspoon of salt and a glass of warm water. Rinse your mouth with this solution for two minutes; After this, the solution must be spat out.
Oral candidiasis is a contagious disease that can spread to internal organs and cause serious harm to them, making it impossible for you to eat normally (if the esophagus, stomach and intestines are affected). If you suspect you have one or more of the symptoms of oral thrush, contact your dentist immediately for an accurate diagnosis. By identifying candidiasis early, your doctor can relieve symptoms and stop the infection.
How to treat candidiasis in the mouth -
The article is for informational purposes only, and we urge you not to self-medicate, despite the fact that some antifungal drugs are still available over the counter. You need to start with a microbiological study, and also a test for HIV infection.
Microbiological test - before starting to take antifungal drugs, it is very important to perform a microbiological test (culture of material from your oral cavity - identifying the amount of Candida, as well as determining the sensitivity of Candida to the main antifungal drugs). Please note that the analysis must include not only sensitivity to drugs, but also the number of Candida fungi.
The latter will make it possible to distinguish acute or chronic fungal infection from a banal carriage and, thus, confirm the diagnosis. Different laboratories may use different methods to determine antifungal susceptibility. The cheapest and most inaccurate is a Russian-made test that determines sensitivity to 6 antifungal drugs using the disk diffusion method (using disks produced by the Scientific Research Center for Physics, Russia). It is best if sensitivity to drugs is analyzed on a VITEK analyzer, France.
Treatment of oral candidiasis takes an average of 12-15 days (until the symptoms of the disease completely disappear). However, in patients with chronic candidiasis who have already had repeated relapses, maintenance courses of therapy will also be required. In case of a widespread process, treatment of the disease should be carried out by a dentist - in collaboration with doctors of other specialties (general practitioner, gynecologist, mycologist).
1) Local treatment for mild primary form of the disease -
Abroad, there are a large number of drugs for the treatment of mild forms of oral candidiasis, intended for local use in the oral cavity. These are special mucoadhesive tablets with Miconazole 50 mg, which are taken only once a day. These are lozenges with Clotrimazole 10 mg, which dissolve in the mouth in about 20 minutes and should be taken 5 times a day. This is a special oral suspension of Nystatin 100,000 Units/ml, which is taken 5 ml 4 times a day (this suspension is kept in the mouth for several minutes and then swallowed).
But all these drugs are not available in Russia (although some of them will be available to you, for example, if you live in Ukraine). But let's look at what is available to residents of Russia, and we'll start with the simplest.
1) The first option is tablets with Nystatin, 500,000 units, which can be used for resorption - 1 tablet. 4 times a day, i.e. approximately every 6 hours. For children, a single dosage will be 125 thousand units or 250 thousand units, depending on age, and the dosage regimen will be similar. Nystatin is not absorbed through the oral mucosa and into the gastrointestinal tract, but has an unpleasant taste and can occasionally cause nausea, vomiting and diarrhea. Additionally, this is a prescription drug and should only be used as directed by a doctor.
2) Another antifungal drug for topical use in the oral cavity is Amphotericin B, which is sold in 50 mg bottles (for suspension). This drug is a more effective analogue of nystatin. It is usually used for intravenous administration in severe systemic forms of candidiasis. However, there is a large number of studies, as well as clinical practice, when the suspension was used for use in the oral cavity. It must be said that “Amphotericin B” (as well as Nystatin) is practically not absorbed into the gastrointestinal tract or through the oral mucosa. The suspension is used 3 times a day (each time a 50 mg bottle is diluted with 5 ml of solution). Remember that this is also a prescription drug and should only be used as directed by a doctor.
3) Probably the best option is the drug “Diflucan powder”, which contains fluconazole and is intended for preparing a suspension. After dilution, 1 ml of suspension will contain 10 mg of fluconazole. For erythematous (atrophic) form of candidiasis, you need to use 50 mg 1 time per day for 7-14 days, but for pseudomembranous or hyperplastic candidiasis, the dosage is already 100 mg 1 time per day. The suspension should be kept in the mouth for a few minutes (rinse) and then swallowed. One bottle costs from 500 rubles, and is enough for 7 applications of 50 mg each.
Provided that the patient's Candida fungi are equally sensitive to all 3 drugs, a fluconazole suspension will be more effective than nystatin (since the latter has poor adhesion to the oral mucosa), and show the same effectiveness as an Amphotericin suspension. Please note that Diflucan powder for suspension is also only a prescription drug that is not intended for self-medication and should be used only as prescribed by a doctor.
Additional local therapy –
As additional local therapy, solutions for rinsing the oral cavity, as well as antifungal drugs in the form of gels (for application to the affected areas of the oral mucosa) can be used.
- best of all is an antiseptic solution of Chlorhexidine 0.2%,
- Warm soda rinses can also have a weak effect,
- gel with miconazole (for applications to the oral mucosa).
Moreover, the use of the antiseptic Chlorhexidine in addition to therapy with antifungal agents is strongly recommended for the development of candidiasis while wearing removable dentures, as well as against the background of poor oral hygiene.
2) Systemic therapy for moderate and severe oral candidiasis -
The first line of treatment for oral thrush in adults (for moderate to severe oral candidiasis) is fluconazole tablets. It has the advantage that, unlike nystatin and amphoterecin, firstly, it is well absorbed in the intestine, and secondly, it penetrates into saliva in large quantities. Before starting to take the drug or in the first days of taking it, it is very important to consult a dentist and remove all supra- and subgingival dental plaque, which, among other things, is a reservoir of Candida fungi in the oral cavity.
The same applies to patients with removable dentures, who will also need to undergo ultrasonic cleaning of the remaining teeth, as well as professional disinfection of the denture. What else is important to know. We have already said above that fungi of the genus Candida quite often demonstrate resistance to fluconazole (especially in patients with repeated relapses of thrush). For example, while Candida albicans shows good sensitivity to fluconazole, the fungal species C. glabrata and C. krusei show resistance in approximately 35% and 75% of cases, respectively.
Therefore, fluconazole therapy should be started only after a microbiological examination - culture of material from your oral cavity and identification of the sensitivity of the fungal flora to the main antifungal drugs. If the study shows the sensitivity of your Candida fungi to fluconazole, it is taken in a dosage of 150 mg 1 time per day (treatment course is 7-14 days). If we are talking about treating another relapse of oral candidiasis, then suppressive therapy will also be required. This means after completing the main course of treatment, you will have to continue taking fluconazole 100 mg 3 times a week. The duration of the course of suppressive therapy is determined by the doctor.
If Candida is resistant to fluconazole –
In case of insensitivity to fluconazole, Itraconazole capsules are first prescribed (taken only as prescribed by a doctor - usually 200 mg once a day, duration of therapy is usually 28 days). This is a prescription drug that, due to side effects, is not suitable for self-medication and should therefore only be used when prescribed by a doctor. Other drugs that can be used for fluconazole resistance include Voriconazole, Posaconazole, and Isavuconazole.
By the way, the basic dosage of 100 mg per day prescribed in the instructions for Itraconazole is much less effective than a dosage of 200 mg per day. This is confirmed by clinical studies, and this is especially true for patients with weakened immune systems and in the presence of aggressive subspecies of fungi of the genus Candida - such as C.glabrata and C.krusei. The same applies to the duration of use. For example, the instructions for intraconazole only say about 15 days of therapy (and not 28 days), but in case of weakened immunity, or in the presence of aggressive strains of Candida, such a duration of treatment is highly likely to lead to the development of relapses of candidiasis in the near future.
Table 1 - “Resistance of antifungal drugs to different types of fungi of the genus Candida.”