Infectious processes and swelling
Often infection with various infections leads to negative changes on the skin of the penis.
Naturally, we are talking about those diseases that have the ability to be transmitted from person to person through sexual contact.
Among them:
- chlamydia is a common pathology caused by chlamydia
- herpes is a viral disease that leads not only to redness, but also to ulceration of the skin, followed by a rather long healing period
- indurative edema in syphilis is a variant of the body’s reaction to the penetration of Treponema pallidum into it
- candidiasis of the head and foreskin is an infectious disease of fungal origin, infection of which does not necessarily occur after sexual contact, since candida is an opportunistic microorganism that does not always provoke the development of the disease
It is important to understand that infectious processes in most cases are accompanied by additional symptoms.
If the patient can ignore them, it is with great difficulty.
When changes occur in the area of the glans penis, in most cases it is STIs that are diagnosed.
Since patients go to the doctor with them much more often.
Short frenulum of the foreskin
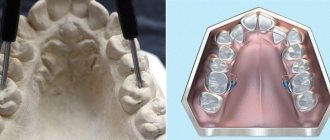
It is possible to identify a short frenulum of the foreskin only starting from adolescence, so young men in puberty need to consult a urologist or andrologist. Diagnosing a short frenulum of the foreskin is not difficult and is based on an analysis of the patient’s complaints and data from an objective examination of the penis. Timely diagnosis of a short frenulum of the foreskin allows one to prevent complications of this pathology.
The only possible treatment option for a short frenulum of the foreskin is surgical, aimed at increasing the length of the frenulum. For this purpose, plastic surgery of the short frenulum of the foreskin (frenulotomy) is performed, and sometimes removal of the frenulum (frenulectomy) is performed using conventional surgery, as well as with a laser or radio wave scalpel. Contraindications to surgery are inflammatory diseases of the external genitalia, including STDs. Frenulotomy is a minimally invasive procedure performed on an outpatient basis, usually under local anesthesia. In the absence of previous ruptures of the short frenulum of the foreskin, a standard transverse-longitudinal frenulotomy is advisable, which consists of a transverse dissection of the frenulum and subsequent suturing of the wound edges in the longitudinal direction.
It is important to carry out the operation in advance, avoiding spontaneous rupture of the frenulum. If it ruptures, it is necessary to stop the bleeding, treat the wound with an antiseptic, apply a sterile bandage and immediately consult a doctor. In order to eliminate the rupture of the short frenulum of the foreskin, it is sutured, antibacterial ointments and local baths with herbal decoctions and antiseptics are prescribed. In the presence of previous ruptures and cicatricial deformation of the short frenulum of the foreskin, a Z-shaped frenulotomy is performed, which allows, due to the zigzag shape of the postoperative scar, to avoid its excessive tension during sexual intercourse. When a short frenulum is combined with phimosis, partial or complete circumcision of the foreskin (circumcision) is also performed.
After frenulotomy, the length of the frenulum increases by 1–1.5 cm, its elasticity and sensitivity are preserved. Complete healing of the wound occurs within 2 weeks. During the postoperative period, the patient is able to work, but must abstain from sexual intercourse.
Prognosis of a short frenulum of the foreskin
In the absence of correction of the short frenulum of the foreskin during sexual intercourse, there is a high risk of permanent ruptures of the frenulum with scar deformation and aggravation of the clinical manifestations of the pathology. Timely treatment of a short frenulum of the foreskin allows you to avoid its trauma in the future and restore the patient’s normal sex life.
Other causes of penis swelling
Often patients are interested in the question of why the head swells after circumcision.
In this case, swelling is a normal temporary reaction of the body.
The body thus reacts to external invasion, responding to surgical intervention with an inflammatory process.
As doctors note, postoperative swelling subsides in patients quite quickly (on average, no more than 4 days are required).
If swelling not only lasts too long, but also severe pain or other changes in well-being appear after surgery, there is a high probability of infection.
In this case, you should see a doctor!
Another reason why the skin around the head may be affected is diabetes.
The fact is that with this endocrine pathology, the composition of urine changes.
It begins to negatively affect the skin around it due to the high glucose content.
It is also worth remembering that altered urine becomes an excellent breeding ground for the proliferation of various pathogenic microorganisms.
This only increases negative symptoms.
Balanoposthitis
Andrey
May 21, 2022 at 10:56 pm
Good afternoon, doctor! I have a strange situation. So I had to look for advice on the Internet. There is inflammation on the head. Nothing else really worries me. Now I will try to explain the situation. About 7 years ago there was a suspicion of candidiasis, they treated it, it seems to have gone away. Last summer there were spots on the head, they didn’t bother me, they didn’t itch, they were just there, there was no smell and no problem either. I went to the dermatologist, but there were still spots on the head (the one on the shoulders