November 30, 2021
One of the main reasons for the spread of rotaviruses is non-compliance with personal hygiene rules, when transmission of infection occurs through hands, which in turn contaminate dishes, toys, and linen
The pathogen is transmitted through dirty hands, that is, the transmission mechanism is fecal-oral, although airborne droplets are also possible. It can affect people at any age, and the causative agent of rotavirus gastroenteritis is a virus from the order Rotavirus, family Reoviridae. Routes of transmission: contact and household (through dirty hands and household items); aqueous (when drinking water infected with viruses, including bottled water); nutritional (most often when consuming milk and dairy products).
The possibility of airborne transmission of rotavirus infection cannot be ruled out. But one of the main reasons for the spread of rotaviruses is non-compliance with personal hygiene rules, when transmission of the infection occurs through hands, which in turn contaminate dishes, toys, and linen.
The carrier of the infection is a sick person or a healthy virus carrier. The virus multiplies in the cells of the mucous membrane of the gastrointestinal tract and is excreted in the feces for up to 3 weeks (usually 7-8 days from the first symptoms of the disease). Damage to the mucous membrane of the digestive tract disrupts the digestion of food and leads to the development of severe diarrhea and dehydration. The main mechanism of transmission of rotavirus infection is through food. Infection occurs through the fecal-oral route.
The main risk factors for the development of candidiasis include:
- improper oral hygiene;
- wearing orthopedic structures or removable dentures;
- long-term inhalation therapy;
- decreased salivation due to certain pathologies;
- hypothermia;
- stress;
- taking antibiotics;
- changes in hormonal levels;
- decreased immunity, including due to chronic diseases;
- endocrine pathologies, including obesity, diabetes;
- smoking;
- carrying out chemotherapy or radiation therapy.
Oral candidiasis occurs much more often in children than in adults. Newborns can become infected even in utero if the mother has thrush - infection occurs during natural childbirth. After birth, the infection can be transmitted to the child through the skin of the mother's nipples and hands, and from her oral mucosa. The source of infection is unsterile pacifiers and oilcloths, and medical personnel who do not follow the rules of asepsis and antisepsis during invasive procedures. In an older child, oral candidiasis is often caused by a weakened immune system or improper dental care.
NON-ODONTOGENIC AND SPECIFIC INFECTION
NECROTIC STOMATITIS (VINCINS ULCER-NECROTIC GINGIVOSTOMATITIS)
Main pathogens
Fusobacterium is concentrated in the gingival sulcus
, pigmented
Bacteroides
, anaerobic spirochetes. With necrotizing stomatitis, there is a tendency for infection to quickly spread into surrounding tissues.
The causative agents are F. nucleatum, T. vinsentii, P. melaninogenica, P. gingivalis and P. intermedia
.
In patients with AIDS, C. rectus
.
Choice of antimicrobials
Drugs of choice:
phenoxymethylpenicillin, penicillin.
Alternative drugs:
macrolide + metronidazole.
Duration of therapy:
depending on the severity of the current.
ACTINOMYCOSIS
Main pathogens
The main causative agent of actinomycosis is A.israelii
, association with gram-negative bacteria
A. actinomycetemcomitans
and
H. aphrophilus
, which are resistant to penicillin but sensitive to tetracyclines, is also possible.
Choice of antimicrobials
Drugs of choice
: penicillin at a dose of 18-24 million units/day, with positive dynamics - transition to step-down therapy (phenoxymethylpenicillin 2 g/day or amoxicillin 3-4 g/day).
Alternative drugs
: doxycycline 0.2 g/day, oral drugs - tetracycline 3 g/day, erythromycin 2 g/day.
Duration of therapy
: penicillin 3-6 weeks IV, drugs for oral administration - 6-12 months.
Oral candidiasis is divided into 3 types:
- Pseudomembranous. This is a classic thrush in the form of a superficial white film or white spots. Accompanied by a feeling of slight discomfort. In mild forms of the disease there may be only a few such plaques, and they can be easily removed. In severe cases, many large spots appear, they merge and gradually affect the entire mucous membrane, and can penetrate lower, affecting first the throat, and then the esophagus, up to the gastrointestinal tract. The spots may thicken, making them difficult to remove. Most often, ordinary acute candidiasis occurs in adults who have taken antibiotics, immunosuppressants or corticosteroids, as well as in infants.
- Atrophic. It can be acute or chronic. In the first case, there may be no plaque, but the mucous membrane becomes inflamed - it becomes bright red, the patient complains of a strong burning sensation in the mouth, increased dryness, and sometimes an unpleasant taste with a hint of bitterness or metal. Most often, acute candidiasis is a consequence of drug therapy. The chronic form usually occurs due to wearing orthodontic structures or dentures. The symptoms of the disease are more subtle.
- Hyperplastic. Candidiasis in the mouth affects the lips, corners of the mouth, cheeks, soft palate, and back of the tongue. White spots are usually large, merge with each other, and may acquire a yellow tint. Gradually they become rough and cannot be scraped off. The disease is chronic and is diagnosed only in adults.
Treatment of candidiasis in the mouth
There are several types of candidiasis of the oral mucosa, but treatment tactics do not differ significantly.
The most commonly used drugs for oral candidiasis are local antimycotics in the form of aerosols, solutions, gels, for example, fenticonazole, miconazole or amphotericin B.
Additionally, antiseptics with antifungal activity are used in the form of solutions for rinsing or lubricating lesions. For rinsing, preparations based on hexetidine and chlorhexidine are often used. A good medicine for candidiasis in the mouth is Lugol's solution, it is used to lubricate plaques.
To strengthen the immune system, it is recommended to take vitamins, especially C, P and group B.
Oral and even infusional antifungal antibiotics for oral candidiasis (sertaconazole, miconazole, isoconazole) are required for severe or chronic disease.
It is important that during the therapy period patients follow a diet that excludes fast carbohydrates (all types of sweets), since they are an excellent breeding ground for candida. Patients should refrain from eating sour and spicy foods.
When treating oral candidiasis in children, it is recommended to carry out “alkalinization” - treating pacifiers, bottles and toys that the baby may put in the mouth with a baking soda solution.
Currently, the problem of mycotic diseases is acquiring important social significance. The increase in the incidence of mycoses is associated with many factors, primarily with the active use of antibacterial drugs in medical practice, which undoubtedly increases not only the incidence of candidiasis, but also mycoses caused by filamentous fungi. This is also facilitated by the use of cytostatics, corticosteroids and other drugs with immunosuppressive properties. The development of mycosis is promoted by a combination of many reasons associated with the urbanization of modern life of the population [1–4].
The wide distribution of fungi in nature, their constant presence both in the environment and in the body, makes contact and infection of humans inevitable. Particularly alarming is the increase in the number of patients with deep mycoses, which include some mycoses of the ENT organs.
Currently, approximately 100,000 species of microscopic fungi have been identified, of which more than 400 species are capable of causing infections in humans, but about 100 species are of real importance in clinical practice [5].
An analysis of clinical and laboratory studies conducted at the Moscow Scientific and Practical Center of Otorhinolaryngology showed the increasing importance of fungal pathology among general ENT morbidity. So, in 2010-2011. among patients with chronic inflammatory pathology of the ENT organs who applied to the mycology room of the Center’s advisory department, fungal infection was detected in 23% [6].
In this regard, the problem of mycoses of the ENT organs remains relevant, which determined the purpose of this work: to familiarize otorhinolaryngologists with modern principles of diagnosis and treatment of mycoses of the upper respiratory tract and ear, varying in localization and nature of clinical manifestations.
Nosological forms of fungal diseases of the ENT organs are otomycosis, pharyngomycosis, laryngomycosis, fungal infection of the nasal cavity and paranasal sinuses. There are superficial mycoses, which affect the skin, mucous membrane, external auditory canal, pharyngeal cavity, and deep mycoses affecting, for example, the SNP, the postoperative cavity of the middle ear, accompanied by invasion of the fungus not only into the epithelium, but also into surrounding tissues.
According to our data, in recent years, the frequency of detection of pharyngomycosis is 45%, otomycosis - 42%, mycosis of the nasal cavity and SNP - 8%, laryngomycosis -5% among all patients with mycosis of the ENT organs [3, 7].
The proportion of otomycosis among otitis of other etiologies reaches 25.3%, pharyngomycosis in chronic pharyngitis and tonsillitis - 26%. Fungal infection of the larynx in chronic laryngitis reaches 15%; in chronic inflammation of the nose and SNP, the share of the fungal process is 7%.
External fungal otitis, fungal otitis media and fungal infection of the postoperative middle ear cavity occur in 69, 18 and 13% of cases of otomycosis, respectively. The main causative agents of external fungal otitis are molds of the genus Aspergillus
(65%),
Penicillium
(5%), with mycosis of the postoperative cavity the proportion of mold fungi reaches 95%, while with fungal otitis media, yeast-like fungi of the genus
Candida
(79%).
In some cases, fungal diseases of the ears can be caused by fungi of the genera Mucor, Alternaria
, etc. In 17% of cases, we noted a combined infection with
Aspergillus
spp.
and Candida
spp.
in combination with representatives of Staph.
spp and
Pseudomonas
spp.
Infection with two or more species of fungi Aspergillus
spp.
+ Candida
spp.,
Aspergillus
spp.
+ Candida
spp.
+ Alternaria alternata
occurs in 1% of observations.
Candida are the leading pathogens
(97-99% of observations).
In mycosis of the nasal cavity and SNP, mold fungi account for up to 78% of the lesions. The main pathogen is a fungus of the genus Aspergillus
, species -
fumigatus
and
niger
, in some cases, in immunocompromised patients, fungal diseases of SNP can be caused by fungi of the genera
Mucor, Alternaria, Rhizopus, Rhizomucor
, etc.
Basically, all these types of fungi belong to the group of opportunistic fungi and cause disease only under certain conditions that predispose to the development and reproduction of fungi, ensuring their transition from saprophyte to the realization of pathogenic properties.
Among the risk factors for the development of mycoses of the ENT organs, the leading positions are occupied by iatrogenic immunodeficiency states that develop as a result of massive antibiotic therapy, long-term use of glucocorticoid and immunosuppressive drugs for oncological and autoimmune diseases. Mycoses of the ENT organs often accompany severe somatic pathologies, such as HIV infection and AIDS, diabetes mellitus, thyroid dysfunction, agranulocytosis, anemia, bronchial asthma, etc.
The pathogenesis of mycosis consists of adhesion (attachment of the fungus to the surface of the mucous membrane or to the skin), colonization of fungi and their invasive growth. In severe forms of ENT mycosis, the next stage is the generalization of the process: the penetration of fungi into the blood with dissemination and the appearance of secondary foci of mycosis in various organs and tissues. This is especially true for fungi of the genus Aspergillus
spp., the pathogenicity factor of which is their ability to grow at 37 °C, the presence of enzymes (protease, phospholipase), toxins (aflatoxin, fumagillin, etc.), pronounced angioinvasiveness and the ability to evade immune surveillance due to the production of inhibitors of the phagocytic function of macrophages and neutrophils, for example gliotoxin [1, 5].
A factor contributing to the development of otomycosis is, first of all, trauma. When the skin and mucous membrane are damaged, paths are opened for the fungus to penetrate deep into the tissues, and protective reactions at the site of damage are weakened. In addition, the secreted secretion of the injured integumentary epithelium is a good nutrient medium for the proliferation of fungi. Thus, a paradoxical phenomenon has been noted: fungal diseases of the outer ear more often occur in extremely careful people who intensively use cotton swabs and other objects to clean their ears, injuring the skin of the external auditory canal and often causing traumatic invasion of the pathogen. Speaking about the need for proper, gentle removal of excess sulfur, it should be remembered that its presence in a small amount in the ear canal is necessary, since it not only mechanically protects the skin, but also carries out bactericidal and fungicidal functions.
The occurrence of a fungal infection of the outer ear is often preceded by water entering the ear during bathing or removing wax plugs by washing. Long-term local use of glucocorticoid drugs, antibiotics, and antiseptics for otorrhea, which accompanies a purulent-inflammatory process in the middle ear, leads to the development of otomycosis in 20% of cases.
Surgical sanitation of the middle ear in the absence of a positive effect from previous courses of antibacterial therapy, local and physiotherapeutic conservative treatment often entails the development of fungal infection of the postoperative cavity. Perhaps in such cases there is undiagnosed fungal otitis media. Surgical treatment in this case can be performed only after negative repeated mycological studies.
Otomycosis can also develop when working in dusty conditions and in pressure complexes with high pressure and humidity.
Fungal infection of the pharynx and larynx often develops in patients after massive high-dose antibacterial therapy, long-term systemic use at a dose exceeding 0.3 mg/kg/day (in terms of prednisolone) for more than 3 weeks, and local use of inhaled forms of corticosteroids for hormone-dependent bronchial asthma. A stay in the intensive care unit for more than 10 days, accompanied by laryngeal intubation for more than 5 days, significantly increases the risk of developing mycoses. Smoking, the use of removable dentures and their improper treatment contribute to the development of mycosis of the pharynx and larynx.
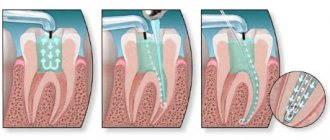
Mycosis of the nasal cavity as an independent disease is extremely rare, usually due to trauma to the nasal mucosa in HIV-infected people. More often, the fungal process affects the maxillary sinuses after foreign bodies enter them (filling material when filling the canals of the 4th-7th teeth of the upper jaw).
Complaints and clinical manifestations of mycosis of the ENT organs
are determined by the characteristics of vegetation and parasitism of certain types of fungi and are largely determined by the localization of the pathological process.
In all forms of mycotic diseases of the upper respiratory tract and ear, there is a specific discharge in the form of crusts, plaques, thick caseous or liquid secretions, the color, quantity and consistency of which depend on the type of fungus and the phase of its development. The clinical picture, despite the diversity of pathogens, has a number of specific features. Main complaints with mycotic otitis media
- discharge from the ear, formation of “plugs” in the external auditory canal, itching, pain, ear congestion.
Thus, with otomycosis caused by dermatophytes, the skin of the auricle, postauricular area and external auditory canal is mainly affected. Patients are concerned about itching and peeling of the skin of the affected area. In the external auditory canal there is dry discharge in the form of plaque and films. Inflammatory phenomena are not expressed. Accelerated formation of sulfur plugs was noted.
For otomycosis caused by mold fungi ( Aspergillus, Penicillium, Mucor
etc.), the skin of the external auditory canal, the postoperative cavity, and less often the middle ear cavity and the skin of the auricle are affected. The patient experiences severe pain, severe hearing loss, and dizziness. The discharge looks like “wet newspaper.” The symptoms of inflammation are significantly pronounced. After removal of the pathological discharge, granulations are visualized, the skin is damaged and bleeds easily. The disease can occur as necrotizing external otitis with damage to the bones of the skull.
With candidal otomycosis, the middle ear cavity and the skin of the external auditory canal are affected. Upon examination, maceration and infiltration, reminiscent of weeping eczema, are determined. The process often spreads to the skin of the auricle and the area behind the ear. Pain and itching are moderate. Some patients in the acute stage may have complaints of increased body temperature, headache, increased sensitivity of the auricle and postauricular area.
Mycotic otitis media and mycosis of the postoperative cavity are characterized by the following clinical manifestations: hearing loss, noise in the ear, pain, discharge from the ear, periodic itching, congestion and dizziness.
Otomycosis, like other types of specific inflammation, has a chronic course with a subtle onset of the disease, its gradual development and significant duration. The development of a fungal disease is possible at any age; frequent exacerbations and relapses of the disease during treatment are typical.
For fungal infections of the pharynx
patients complain of discomfort in the throat, burning sensation, dryness, rawness, and soreness, which may be more pronounced than with bacterial pharyngitis. Painful symptoms are moderate; when swallowing and eating irritating foods, the pain intensifies. Sometimes patients note irradiation of pain in the submandibular region, on the anterior surface of the neck and in the ear. Depending on the degree of damage, pseudomembranous, hyperplastic, granulomatous and erosive-ulcerative clinical forms of pharyngomycosis are distinguished. Specific signs of the clinical picture of pharyngomycosis are the presence of plaque, swelling of the mucous membrane and pronounced general symptoms of intoxication; frequent (up to 10 times a year) exacerbations are also characteristic.
For fungal infection of the larynx
patients are worried about pain in the throat and on the front surface of the neck, a feeling of “rolling a lump” in the throat and neck, not associated with swallowing, constant hoarseness, rapid fatigue of the voice, and an unproductive cough. On examination, congestive hyperemia of the mucous membrane of the larynx, swelling of the mucous membrane of the vocal folds, and fibrin deposits are characteristic, when removed, the eroded surface is exposed. Often the fungal process is one-sided, which must be differentiated from cancer and tuberculosis.
Fungal infection of the nose and SNP
divided into invasive and non-invasive forms. Invasive forms include acute (fulminant) and chronic forms. Non-invasive ones include fungal body and allergic fungal sinusitis.
Invasive forms of fungal infection of the SNP are extremely unfavorable in predicting the outcome of the disease. The fulminant form of SNP damage is most often caused by fungi belonging to the class Zygomycetes. This form of the disease occurs in patients with severe immunodeficiency, decompensated diabetic ketoacidosis, neutropenia, and burn disease. Zygomycosis is characterized by an extremely severe course and, without active antifungal therapy and early surgical treatment, usually ends in death.
The chronic form occurs as chronic sinusitis with reactive phenomena from surrounding tissues. Accompanied by copious purulent nasal discharge in the morning, severe pain in the projection of the affected SNP.
The fungal body is quite often a “diagnostic finding” when performing a CT scan of the ED and in some patients is asymptomatic.
With allergic fungal sinusitis, in addition to polyps in the nasal cavity and SNP, a thick, viscous secretion is detected in the lumen of the latter.
Lack of awareness among otorhinolaryngologists regarding the diagnosis of fungal infection of the ENT organs is often the reason for their late and/or incorrect diagnosis. This creates difficulties in treatment and leads to a chronic course of the disease.
Diagnosis of fungal disease of ENT organs
, like any infectious disease, is established only on the basis of complex laboratory mycological research methods. A pronounced clinical picture of a disease similar to a fungal infection, no matter how characteristic it may be, is not the basis for making a final diagnosis of mycosis.
Diagnosis of mycosis is carried out in the following areas:
1. Microscopy of pathological discharge.
2. Inoculation of pathological discharge on various elective nutrient media to isolate fungal cultures and their generic and species identification.
3. Determination of the sensitivity of isolated fungi to antifungal drugs.
4. Radiation diagnostics in cases of damage to the nose and special organs.
Sampling of biological material from the ear is carried out using an attic probe or a Volkmann spoon. Pathological discharge from the deep parts of the external auditory canal is placed between two fat-free sterile slides and microscoped at 100, 200 and 400 times magnification.
In the active stage of aspergillosis and mucorosis with abundant formation of mycotic masses with aerial mycelium, we recommend using an operating otorhinolaryngological microscope (otomicroscopic method of express diagnostics) for diagnosis.
If a fungal infection of the pharynx and larynx is suspected, microscopy of scrapings from the mucous membrane of the oral cavity, pharynx, tonsils, taken with a swab to detect elements of the fungus, and seeding of material from the affected areas of the mucous membranes are performed.
The main method for diagnosing mycosis of SNP is culture of aspirate or rinsing water (puncture using a Kulikovsky needle according to the usual method) with mandatory identification of the pathogen. A histological examination of the biopsy material is also carried out.
In addition to microscopy of native material, microscopic examination of preparations stained using the Romanowsky-Giemsa method is performed. The most informative method that reliably identifies the causative agent of the disease is staining the preparation with solutions of calcofluor white, followed by fluorescent microscopy. For mycological diagnosis, pathological material is inoculated on elective media (Saburo, Chapek, wort agar, etc.). Types of yeast-like fungi of the genus Candida
determined by morphological characteristics and the nature of fermentation of sugars. Inoculation of the material is carried out using the standard method [1, 2, 5]. To clarify the diagnosis, in some cases it is necessary to carry out serological, allergological and histological studies [2, 5].
Treatment
You should always start with eliminating the pathogen. Correction of general and local predisposing factors is carried out in parallel or in the second stage.
When treating a patient with mycosis of the ENT organs, it is necessary to take into account all possible conditions under which this disease arose specifically in this patient with a view to their possible elimination. It is necessary to identify and treat diabetes mellitus, blood diseases, gastrointestinal tract, and immune deficiency. The role of allergies in the pathogenesis of the disease should be taken into account, since mushrooms have pronounced allergenic properties, and hyposensitizing therapy should be carried out in parallel with etiotropic therapy.
Selection of rational antifungal therapy for mycosis of ENT organs
presents certain difficulties. On the one hand, a large number of antimycotic drugs expands the possibilities of treating fungal infections that differ in both localization and type of pathogen. On the other hand, it requires the clinician to have increased awareness of the spectrum and characteristics of their action (fungicidal or fungistatic), pharmacokinetics, compatibility with antibacterial drugs, side effects, etc. The ideal treatment is with an antimycotic that has the least toxic and greatest therapeutic effect, which is not always possible, especially in acute forms of fungal disease, when the choice of drug is made empirically, since the pathogenic fungus is not immediately identified and tests can take a long time. Determining the choice of drug are the results of laboratory mycological studies of the sensitivity of fungi isolated from a particular patient to known antifungal drugs.
Fungal disease of the oropharynx - pharyngomycosis is caused mainly by yeast-like fungi of the genus Candida
, which largely determines treatment tactics. Limited acute candidiasis of the tonsils, which developed as a result of antibacterial therapy, usually heals quickly after stopping the administration of antibiotics and performing only local antifungal treatment. However, widespread lesions of the mucous membrane of the oropharynx, with a tendency to chronicity and recurrence, require a long course of treatment using local and general antimycotic therapy. For systemic therapy, a drug from the azole group, fluconazole (mycoflucan), is used orally at a dose of 100-200 mg once a day. Treatment should be continued for another 14 days after clinical improvement. If such treatment is ineffective, itraconazole (200 mg per day orally) or amphotericin B (1 ml 4 times a day orally, or >0.3 mg/kg per day intravenously) is used [1, 8-10].
In the systemic treatment of pharyngomycosis caused by molds, it is advisable to use itraconazole and amphotericin B, which have a fungicidal effect not only on yeast-like fungi, but also on mold fungi of the genera Aspergillus, Mucor, Penicillium
[12].
In addition to systemic treatment, local treatment is also recommended. During treatment, the pharynx after meals should be lubricated with a solution of clotrimazole at a rate of 10 mg 5 times a day, or nystatin tablets should be dissolved/chewed after meals at a dose of 250-500 thousand units 4-5 times a day. For chronic tonsillitis of fungal etiology, courses of washing the lacunae of the tonsils every other day or 1-2 times a week at least 10 times with solutions of antiseptics with antifungal action (miramistin, quinozol, clotrimazole solution) [10, 11].
Drug therapy for mycosis of SNP always accompanies and/or precedes surgical treatment. In the treatment of fungal infections of the nose and SNP, both general and local measures are provided. For invasive forms of fungal infection of the maxillary sinuses, the most effective is a combination of drug antifungal and surgical treatment. To eliminate the Aspergillus infection at this location, surgical treatment is almost always necessary. Surgical intervention consists of performing radical surgery on the affected sinus using the extranasal method with complete removal of all pathologically altered tissues. In the postoperative period, daily rinsing with antiseptics and antimycotics (amphotericin B, miramistin, pimafucin suspension, clotrimazole) is carried out.
In acute toxic forms of invasive aspergillosis of SNP, antifungal therapy is mandatory. Voriconazole or lipid amphotericin B is used [1, 13]. It is possible to use caspofungin and amphotericin B. After stabilization of the process, treatment with itraconazole. The duration of use of antimycotics depends on the clinical picture of the disease and its course, but should continue for at least 14 days after clinical and laboratory cure [1, 2, 9].
For candidiasis of the nose and SNP, it is necessary to combine the use of systemic antifungals with local antifungal drugs. The drug of choice is fluconazole (mycoflucan), which is prescribed once a day at a dose of 50-200 mg. The course of therapy cannot be less than 14 days. If treatment with standard doses of fluconazole is ineffective, it is possible to increase the dosage to 400 mg/day, or prescribe itraconazole 200 mg/day [10].
Patients with allergic fungal sinusitis are advised to undergo surgery to completely remove the polypous mucous membrane and the viscous “rubber-like” contents of the sinus [1, 13]. In the early postoperative period, it is necessary to wash the SNP twice with an aqueous solution of amphotericin B. It is advisable to prescribe topical nasal corticosteroids to prevent relapse no earlier than 20 days after surgery.
Only in case of resistance to other antimycotics, amphotericin B is used for the treatment of candidal lesions of the nose and SNP (intravenous 0.3 mg/kg per day for 3-7 days). Treatment is carried out under the supervision of biochemical studies of liver and kidney function, since amphotericin B has a pronounced nephro- and hepatotoxic effect.
The specificity of the treatment of fungal infection of the larynx is the widespread use of the inhalation method for administering drugs. The effectiveness of the aerosol method for inflammatory diseases of the larynx is determined by the direct effect of the drug on the site of the disease and the higher concentration of the drug at the site of the lesion. With this method of administration, inhalations with the water-soluble sodium salt of nystatin or levorin are effective, especially for candidiasis. Treatment is carried out for 15-20 minutes 1-2 times a day. The initial course of treatment is 12-15 procedures. In case of resistance to other antimycotics, 12-15-day courses of aerosol therapy with amphotericin B are carried out. All patients with laryngomycosis, in addition to inhalation therapy, must undergo systemic therapy with antimycotics. The drug of choice is fluconazole (mycoflucan) once a day at a dose of 100-200 mg, in severe cases - 300 mg/day) [11]. For patients whose fungal disease in the larynx is accompanied by the formation of a large amount of viscous secretion, it is advisable to carry out inhalations with proteolytic enzymes that selectively break down necrotic masses and dilute the viscous exudate for their better removal. For this, inhalations with chemopsin and chemotrypsin (150 mg in 5 ml of saline) can be recommended.
When treating otomycosis, local and systemic drugs are used. For local treatment of mold lesions in the ear, the most effective are naftifine, nitrofungin, terbinafine (exifin), and for candidiasis - clotrimazole, terbinafine (exifin), naftifine. An indispensable condition for local therapy is preliminary thorough cleaning of the ear using endoscopic equipment or an operating microscope. Ear toileting is performed only by a doctor using an attic probe and a padded cotton pad moistened with an antimycotic drug. Thorough toileting of the ear is given special importance, since even a small amount of mycotic masses significantly lengthens the course of treatment until complete recovery.
In case of external fungal otitis, it is necessary to thoroughly clean the anterior inferior part of the external auditory canal. In case of fungal otitis media, mycotic masses are completely removed from the area of perforation of the eardrum. The postoperative cavity of the middle ear is cleaned in the same way - the entire cavity is thoroughly cleaned, especially in the posterior section, behind the spur. Before treatment, if polyps and granulations are present, they are removed or extinguished with a 20% solution of silver nitrate.
Local treatment with antifungal drugs must be carried out for at least 3-4 weeks under mandatory laboratory control (cultures before, during and after the end of the course of treatment). Local treatment is carried out by placing cotton wool moistened with a fungicidal preparation into the ear, which is left for 5-10 minutes 2-4 times a day, depending on the activity of the fungal process.
For systemic therapy of candidal lesions, the most effective is fluconazole (mycoflucan) - 50-200 mg per day for 14 days. For mold mycoses - itraconazole 200 mg/day for 14 days, terbinafine (exifin) - 250 mg/day for 16 days. If necessary, the course of treatment is repeated after 7 days.
The criterion for the effectiveness of treatment is complete clinical cure within a month, confirmed by both the clinical picture and negative results of mycological research [1, 9].
Quite often, with otitis externa, only a local effect on the mycotic focus of infection is carried out, while with fungal otitis media and mycosis of the postoperative cavity, systemic therapy is mandatory.
Since fungal diseases of the upper respiratory tract and ear are prone to recurrence, dynamic follow-up of the patient is necessary for timely implementation of preventive courses of antifungal treatment. Analysis of our own results of treating patients with ENT mycoses using the above drugs allows us to conclude that they are highly effective, accompanied by the elimination of fungi that cause the disease and normalization of the clinical picture [7, 8, 10].
In general, with proper treatment of mycoses of the ENT organs, therapy is quite effective. Unsatisfactory results are largely explained by the lack of awareness of doctors about the clinical manifestations of mycoses, incorrect diagnostic tactics, as a result of which adequate etiotropic treatment is delayed and carried out at a later stage, when the disease has already spread and become chronic.
Prevention
To prevent the development of the disease, you should carefully monitor the condition of the oral cavity. Every person is recommended to undergo a preventive examination at the dentist once a year and have their teeth treated on time. People who wear dentures should do so more often. Smoking is also one of the causes of thrush, so it is advisable to give up this bad habit.
During the period of antibiotic therapy, it is necessary to take eubiotics to correct the intestinal microflora.
How do probiotics work?
Dysbacteriosis and inflammatory processes in the oral cavity very often cause not only local discomfort, but also discomfort in the gastrointestinal tract and bad breath. Antibiotics, along with pathogenic microorganisms, begin to destroy the beneficial bacteria necessary for humans.
Probiotics are live strains of “friendly” bacteria and bring invaluable benefits to the body:
- help destroy pathogenic microorganisms;
- promote the regeneration of damaged tissues;
- activate the immune system;
- normalize cell metabolism;
- prevent cells from degenerating into malignant formations;
- restore the balance of fluid and beneficial microorganisms;
- prevent allergies;
- removes unpleasant odors from the mouth;
- eliminate toxins produced by pathogenic microorganisms.
Popular questions about candidiasis
How to determine candidiasis?
The disease has a specific symptom - white plaque in different parts of the oral cavity.
Which doctor treats oral candidiasis?
Dentist-therapist.
How is candidiasis treated?
Doctors usually prescribe the following medications to treat oral thrush: chlorhexidine or hexetidine solution, as well as nystatin, amphotericin B, or miconazole. They are available in different dosage forms (in the form of a gel, solution, aerosol), everyone will choose the one that is convenient for themselves.