Introduction
How often, having a preschooler child, we get tired of the seemingly endless runny nose, daily noticing small changes in the amount, thickness and color of “snot”: sometimes liquid and colorless, sometimes thick, green and plentiful. It is not for nothing that popular rumor, with its inherent irony and worldly wisdom, assigned its caustic stamp to preschool age, long before the emergence of the institution of preschool education: the capacious and simple-minded “brat.” And it becomes completely alarming when, despite careful treatment, an obsessive dry cough at night, snoring during sleep, and significant difficulty in nasal breathing do not go away. Rare and such short “bright” intervals of health, and again a runny nose, cough, and sometimes congestion and pain in the ears. And the natural question arises: “Who is to blame? So what should I do? And of course, a trip to the doctor, and maybe more than one, to make a diagnosis: chronic adenoiditis, adenoid hypertrophy . And again persistent treatment and the thought: “Can I remove them already and forget about the problem?” What choice to make: Delete or save? So is it worth fighting and how to do it in modern conditions of medical development? And what is the effectiveness of this fight? We will talk about all this in this article. But let's start with the very basics:
Chronic adenoiditis is a chronic inflammation of adenoid vegetations (accumulations of lymphoid tissue) located in the nasopharynx, accompanied by their mucus (which is manifested by a runny nose, cough, mucus flowing down the back wall of the pharynx), swelling and/or hypertrophy (enlargement) (which is manifested by difficulty in nasal breathing up to to complete absence of breathing through the nose, sometimes snoring during sleep). All or some of these manifestations can occur periodically up to 4-6 times a year or more, or be present constantly for several months.
What are adenoids?
Adenoids are three of the six lymphoid formations (tonsils) of the so-called lymphoid “Pirogov’s ring”: two tubal tonsils (located around the mouths of the auditory tubes) and the nasopharyngeal tonsil (located in the center of the nasopharynx vault. In addition to these three tonsils, the “Pirogov’s ring” includes two palatine tonsils tonsils (tonsillar) and one lingual (located at the root of the tongue in front of the epiglottis). The function of the “Pirogov ring” is very important. This is the main “guard” of the body at the “entrance gate” from possible infection. Everything that enters our body from the outside: air for breathing, food and water, everything undergoes careful control by the lymphatic formations of the nasopharynx and oropharynx (“Pirogov’s rings”). And inflammation is nothing more than the body’s response to an infectious agent (virus, bacteria or fungi), with the aim block the infection, prevent it from entering the body, destroy and remove it.
Age-related features of adenoids (age of adenoid hypertrophy)
It is noteworthy that adenoid lymphoid formations reach their maximum development in preschool age from 1.5-2 to 5-6 years, when the child begins to actively contact the outside world, attend preschool institutions, clubs, sections, and visit places large crowds of people: shops, public transport, cinema, theater, circus, etc. In this case, an exchange of microflora inevitably occurs with surrounding people, including pathogenic ones; in response to this, the adenoids react with inflammation, and as a result, their enlargement. Thus, there is a tireless “training” of the immune response to the action of the infectious agent. That is why in preschool age the adenoids in their physiological norm will be of the 2nd degree of hypertrophy (they occupy ½ of the lumen of the nasopharynx). As a rule, up to 1.5-2 years of age, adenoids are less than grade 1, they are still underdeveloped and do not cause any problems. But at this age a child has much less contacts, and they are limited to family members. If the family does not have many children, then before the child starts attending kindergarten, he either does not get sick at all, or no more than 1-2 times a year. After 8-10 years, adenoids undergo involution (reduction in size); by 12-14 years, most children will not have adenoids when examined. But the lymphoid cells will move to the back wall of the pharynx and will retain their protective role all their lives. This is why it is so important to preserve the immune organ and avoid removal during the “adenoid” (preschool) age.
How to recognize?
The first thing a baby will complain about with chronic tonsillitis is a sore throat and painful swallowing. However, if the child is under 3 years old, he cannot always explain what is bothering him. Therefore, it is important for parents to pay attention to the accompanying symptoms:
- The appearance of bad breath;
- Nervous system disorders: frequent whims and crying, anxiety, rapid fatigue and poor sleep.
- These are the first symptoms, the manifestation of which can be missed. After them, as a rule, the child develops:
- Low temperature (up to 37.5 degrees);
- Nasal congestion and enlarged lymph nodes;
- The tonsils increase in size and purulent plugs appear on them;
- Possible simultaneous occurrence of otitis media or sinusitis.
Degrees of hypertrophy (enlargement) of adenoids
I degree - when adenoid vegetations during endoscopic examination cover less than 1/3 of the lumen of the choana (the outlet from each half of the nose into the nasopharynx)
II degree - when adenoid vegetations during endoscopic examination cover 1/2 of the lumen of the choana (the outlet from each half of the nose into the nasopharynx)
III degree - when adenoid vegetations during endoscopic examination cover the entire lumen of the choana (the outlet from each half of the nose into the nasopharynx)
Often, ENT doctors assign grade II-III - in the case when more than ½ of the lumen of the choanae is closed, but the lumen for breathing still remains, and is not completely closed.
Contraindications to adenotomy
The operation is not performed on children under 2 years of age, except in emergency situations. General contraindications to adenotomy are:
- ARVI, influenza and other acute infections;
- exacerbation of allergies;
- blood clotting disorder;
- cleft lip and palate;
- malignant tumors of any location;
- intolerance to drugs for pain relief or anesthesia;
- concomitant pathologies (heart malformations) in specialized centers;
- anomalies of nasopharyngeal vessels.
A temporary ban may be the recent performance of other surgical interventions. Preventive vaccinations are also a reason to postpone surgery. It is recommended to wait at least 1-2 months after vaccination.
Symptoms of chronic adenoiditis and adenoid hypertrophy
- Frequent lingering runny nose
- Nasal congestion, up to complete absence of nasal breathing
- As a result of the previous symptom, the child often breathes with his mouth open during the day or during sleep
- Cough, including dry cough at night (due to mucus draining down the back of the throat)
- Snoring while sleeping
- Decreased attention and fatigue due to lack of oxygen through nasal breathing
Is it possible to “give up” on these symptoms?
Even the uncomplicated form of chronic adenoiditis cannot be ignored; oxygen starvation, which develops against the background of difficulty in nasal breathing or breathing through the mouth, is manifested by a decrease in memory, perseverance, attention, and learning ability. The child becomes irritable, capricious, and gets tired quickly. The immune system is under constant stress of chronic inflammation, as a result of which a symptom of natural immunodeficiency appears, due to the depletion of the cellular elements of the immune system, and the child becomes weakened and often ill. With a large degree of hypertrophy, the facial skeleton may change, the so-called “adenoid” type of face is formed with an elongated lower part of the skeleton, a change in the bite, and a slightly open mouth.
In addition, we are afraid of the formation of complications
Complications of chronic adenoiditis and adenoid hypertrophy:
- Acute otitis media
- Exudative otitis (so-called “silent” otitis, when in the absence of pain hearing loss occurs due to the accumulation of fluid behind the eardrum)
- Persistent conductive hearing loss
- Frequent sore throats
- Tracheitis, bronchitis
- Sinusitis, ethmoiditis, sinusitis
Indications for surgery
The operation to remove adenoids in children is called adenotomy. For children under 3–4 years old it is indicated in the following cases:
- holding your breath during sleep (sleep apnea);
- severe swelling of the nasopharynx, which prevents the child from eating and sleeping;
- lack of effect from drug therapy.
For children aged 5 years and older, surgery is performed if stage II or III pathology is diagnosed, when the nasopharyngeal canal is blocked by overgrown lymphatic tissue up to 60% or more. At such stages of the disease, there are clear signs of a negative effect on the body, which include:
- often recurrent otitis media;
- constant headache;
- decreased hearing acuity due to fluid accumulation in the ears, behind the eardrums;
- various sleep disorders: snoring, apnea, snoring;
- delay and improper development of speech skills;
- deformation and malformations of the osseous-facial structure;
- constant difficulty breathing;
- nasal voice.
Hypertrophied adenoids affect not only physical health. Pathological proliferation of lymphatic tissue can provoke nervous tics, convulsions, enuresis, and increased excitability. With a long course of the disease, the child’s face takes on a characteristic adenoid type: the mouth is half-open, the chin is displaced.
Traditional diagnostic methods (examination by an ENT doctor or pediatrician)
In a regular clinic, to diagnose chronic adenoiditis and adenoid hypertrophy, an examination of the nose, throat and ears is used using metal instruments for examining ENT organs: nasal and ear mirrors and a spatula illuminated with reflected light, using a conventional head reflector (head mirror) or a head lamp in the form flashlight. In this case, the ENT doctor (or pediatrician) only sees the area of the nasal vestibule and the surrounding parts of the nose. The nasopharynx, the anatomical location of the adenoids, is not visible. The examination is contact (when examining the nose, the wings of the nose in the vestibule area are expanded with a nasal speculum; when examining the ear, an ear speculum is inserted into the ear canal)
In addition, it will be possible to perform a digital examination of the nasopharynx for a subjective assessment of the size of the adenoids (the doctor feels the nasopharynx and the surface of the adenoids through the mouth, trying to determine their size). This method is not reliable, is unpleasant for a small patient and is traumatic for adenoid vegetations.
Modern diagnostic methods (endoscopic examination of the ear, nose and throat by an ENT doctor)
The gold standard for diagnosis (and the only correct one) is an endoscopic examination of the nasopharynx by an ENT doctor with good skills and experience working with children from birth. An endoscopic examination is an examination using a video camera, with additional powerful lighting and magnification and display on a television screen, on which both the doctor and the child’s parents will clearly see not only all the structures of the nose, but also the nasopharynx with the mouths of the auditory tubes and adenoid vegetations. In this case, the doctor will evaluate the degree of their increase, inflammation of the mucous membrane, the nature of the discharge, the presence and size of the respiratory lumen. The examination is carried out with a special children's nozzle - a tube less than 3 millimeters in diameter, the examination is non-contact, absolutely painless, does not require special preparation (the ENT doctor only drips vasoconstrictor drops in an age-appropriate dosage before the examination) and has no contraindications and is used in children from birth.
Of course, with such a diagnosis, digital examination is not required.
It is very important that during an endoscopic examination of the ears, such a significant complication as exudative otitis (accumulation of fluid behind a healthy, non-inflamed eardrum) will not be missed. Thanks to good lighting and magnification, the eardrum is transparent during endoscopic examination, so the liquid and air bubbles behind it are clearly visible. Whereas when examined in the usual way, the eardrum, if it is not inflamed, reflects the light of a flashlight and looks gray and opaque, the liquid behind it cannot be seen.
Comparative characteristics of traditional examination of ENT organs and endoscopic examination of ENT organs
| Criteria | Traditional ENT examination | Endoscopic examination of ENT organs |
| Price | Low inspection costs due to the use of tools and a reflector | High cost due to the use of expensive equipment |
| Painless | The contact method can be unpleasant due to the instrumental expansion of the entrance to the nose for examination; the use of an ear mirror is also contact. Digital examination is traumatic and can be painful | The method is non-contact, painless, as nozzles of less than 3 mm are used. in diameter |
| Diagnostic reliability | The examination is superficial, the structures of the nose are examined only in the anterior sections, the nasopharynx is inaccessible for inspection, the adenoids and the mouths of the auditory tubes are not visible, it is impossible to assess the condition of the middle ear behind a healthy eardrum | The reliability of diagnosis of adenoiditis, adenoid hypertrophy, and complications in ENT organs is 100%. All structures of the nose, nasopharynx, ear and throat are examined on a screen with additional magnification and lighting. A diagnostic error has been ruled out. |
| Accuracy of the diagnosis | The diagnosis is presumptive | Reliable diagnosis with assessment of possible risks and complications |
| Purpose of treatment | Overdiagnosis, high probability of prescribing antibacterial therapy “just in case” | Prescribing adequate therapy |
| Assessment of dynamics during treatment | Assessment of only external signs and symptoms (presence of runny nose, cough, etc.) | Assessment of both the dynamics of symptoms and mucus and size of the adenoids, development or relief of complications. |
| Recommendations for adenoid removal | It is possible to prescribe removal of adenoids if they can be preserved and monitored. | Appointment of adenoid removal only if there are indications for removal and an objective assessment of the lack of effect of treatment. |
| Who can carry out diagnostics | Pediatrician, ENT doctor with any experience and qualifications | ENT doctor with practical skills and experience in endoscopic examination of ENT organs in children from birth. |
Laboratory diagnostic methods (the goal is to clarify the cause of chronic adenoiditis and/or adenoid hypertrophy)
To establish the cause of enlarged adenoids, as a rule, a detailed blood test is prescribed, a nasal smear for cytology (cellular composition of nasal discharge), blood for total immunoglobulin E (to exclude an allergic nature or allergic background), feces for worm eggs and scraping for enterobiasis ( adenoids often enlarge due to helminthic lesions), a PCR test for the Epstein bar virus is possible (if mononucleosis is suspected)
Diagnosis of enlarged adenoids
Hypertrophied tissues of the nasopharyngeal tonsils cannot be seen with the naked eye, so special techniques are used to confirm the diagnosis:
- radiography;
- endoscopy of the nasopharynx;
- tympanometry – assessment of the condition of the eardrum and middle ear;
- examination by an ENT doctor using special instruments.
Particular attention is paid to children with frequent relapses of adenoiditis. Based on the clinical manifestations of the disease and data obtained during the examination, the doctor decides on the need for surgical intervention.
Treatment of chronic adenoiditis and/or adenoid hypertrophy
Conservative methods:
- Drug treatment (includes the prescription of vasoconstrictor drops in a short course, local anti-inflammatory treatment, general anti-inflammatory or antiallergic treatment, expectorants, antibacterial drugs for bacterial infections, as well as treatment of complications if they occur) IMPORTANT: Treatment methods, as well as drug therapy only prescribed by a specialist doctor. Ideally, an ENT doctor under the supervision of an endoscopic examination of the adenoids and laboratory parameters
- Hardware, manipulation and physiotherapy (includes both mechanical sanitation of adenoid vegetations, for example, washing the adenoids using an electric suction, and numerous options for physiotherapy, both in the form of monotherapy and combining different methods: USOL therapy of the nasopharynx; laser therapy with red, violet, infrared laser; magnetic therapy; treatment with the Intralor device; photochromotherapy with orange color, etc.) The method of exposure is selected by the ENT doctor depending on the clinical picture and individual characteristics of the patient. These methods allow, in most cases, to avoid the unnecessary prescription of antibiotic therapy, significantly reduce the prognosis of the course of the disease, avoid the development of complications, speed up recovery or significantly prolong the remission of the disease, and avoid long-term residual effects.
Surgical treatment of chronic adenoiditis and adenoid hypertrophy:
This treatment method is used only if there are absolute indications for adenoid removal (including the threat of developing persistent hearing loss), and if there is no effect from conservative therapy (including hardware and physical therapy). As practice shows, conservative treatment is effective in more than 99% of children with chronic adenoiditis and adenoid hypertrophy. Any surgical intervention is an “act of desperation” when everything possible has been done, but the effect is not obtained and the threat of serious complications remains.
If there is no effect from conservative therapy and there are absolute indications for adenotomy, we recommend choosing a modern endoscopic method of adenotomy, which is performed endoscopically under visual control, which means it is less traumatic and more effective. The traditional method of removal with an adenotomy is a blind method, does not always achieve full effect and is more traumatic.
“Disadvantages” of adenotomy:
- The operation is performed under general injection anesthesia, therefore it carries the risks of using narcotic drugs like any surgical intervention;
- If there are unforeseen anatomical features of the skeleton of the nasopharyngeal vault (absence, underdevelopment or thinning of bone in the nasopharyngeal vault), there may be a risk of damage to the brain stem;
- the process of scar-adhesive changes in the nasopharynx cannot be excluded, which, in the presence of these changes in the area of the mouths of the auditory tubes, can disrupt the anatomy and cause a deterioration in the patency of the auditory tubes;
- But probably the most important thing is the removal of the immune organ (three lymph nodes: two tubar and one nasopharyngeal), which plays a protective role as an independent organ, and disrupts the functioning of the entire immune system during a very crucial period of its formation. For example, the formation of the most persistent prostaglandin form of bronchial asthma has been proven during adenotomy in children with a certain allergic background. It is impossible to even predict all the consequences of such interference in the immune system.
Of course, all these complications are very rare, but adenotomy should be treated as an operation that carries all possible operational risks.
How is adenoid surgery performed on children?
Adenotomy is performed under general anesthesia, 1 hour including anesthesia. hours depending on the degree of pathology and individual characteristics of the development of the nasopharynx in the child.
What is included in preoperative preparation
The preparation plan before adenotomy includes:
- examination by a pediatrician;
- sanitation of the oral cavity by a dentist;
- consultation with an anesthesiologist;
- examination by a cardiologist.
The following tests will be required:
- UAC;
- test for blood clotting, group and Rh factor;
- blood biochemistry;
- ECG;
- OAM;
- X-ray of the lungs;
- hospital group.
7–10 days before surgery, you should avoid taking medications that affect the rate of blood clotting. For a week, it is advisable to limit children’s contacts with strangers, stay in crowded places, and exclude foods that can cause an allergic reaction from the diet. Measures are necessary to ensure that the operation is as effective and safe as possible for the baby.
How is surgery to remove adenoids performed in children?
There are two options for performing the operation:
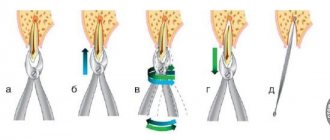
- classic adenotomy, in which the doctor inserts a special instrument (adenotome) through the mouth and cuts off the enlarged tissue;
- endoscopic adenotomy, which is performed using an endoscope and special equipment - a ring knife, a microdebrider shaver (an instrument that simultaneously sucks out the cut-off lymphoid tissue).
Endoscopic adenotomy is considered the standard, in which the operation to remove adenoids in children is carried out under the control of video equipment. In parallel with the removal of nasopharyngeal tonsils, in some cases a vasotomy is performed, which significantly reduces nasal swelling, and tonsillectomy, which involves resection of the palatine tonsils. A combined operation is performed only if there are strict indications and it is impossible to solve the problem by other methods.
Both laser and endoscopic removal of adenoids in children occur according to a specific algorithm:
- the child is given general anesthesia;
- An endoscope and the necessary instruments are inserted into the nasopharynx;
- Using a laser, microdebrider or adenotom, excess tissue is cut off:
- assess the condition of the mucous membranes and blood vessels, the degree of opening of the lumen of the nasopharyngeal canal;
- carefully remove the equipment.
To provide a better view, in some cases doctors use a laryngeal speculum, which is inserted through the mouth. The risk of bleeding is minimal and nasal packing is usually not required.
Possible complications
The only dangerous complication after surgery is bleeding. It occurs in extremely rare cases. After the operation, the child is in the hospital. Sometimes after removal of the adenoids, a child may experience:
- dizziness;
- slight increase in temperature;
- short headache;
- slight nausea.
A slight nasal voice, nasal congestion and a slight runny nose may persist for 4–10 days. In most cases, these phenomena go away on their own and do not require medical attention.
Modern diagnostic and treatment methods offered at ENT Clinic No. 1
Diagnostics:
ENT clinic number 1, Moscow, is a specialized otolaryngology clinic. The clinic’s ENT doctors are fluent in the method of endoscopic diagnosis of ENT organs and have sufficient experience in working with children from birth. An endoscopic examination of the nasopharynx, ears and throat will make it possible to assess the degree of enlargement of the adenoids and the presence of inflammation, as well as to determine the presence or absence of complications.
To clarify the cause of adenoid hypertrophy in the clinic, on the first day of admission, it is possible to take the necessary laboratory tests.
If complications are suspected, on the day of admission tympanometry (diagnosis of middle ear pathology) or ultrasound of the paranasal sinuses if sinusitis or sinusitis is suspected.
Treatment:
Based on the ENT diagnosis, the doctor will prescribe medication, manipulation and physical treatment. ENT clinic number 1 presents the maximum variety of hardware treatment for adenoiditis:
- rinsing the nose with an electric suction;
- laser therapy with red, infrared and violet lasers;
- USOL therapy of adenoids (nasopharynx);
- photochromotherapy with orange color;
- magnetic therapy;
- nasal rinsing using the Intralor device;
- galacamera (salt cave).
These types of physiotherapeutic effects have a wide evidence base in the effectiveness of anti-inflammatory, immunomodulatory, antiseptic, anti-edematous effects on adenoid tissue and absolute safety of use in children of any age. Each method can be used as an independent treatment or in combination with another method. At the same time, different methods of physical therapy act as synergists (increasing each other’s effectiveness and facilitating the penetration of topically applied drugs into the mucous membrane.)
As a consequence of all of the above effects, the prescribed combination treatment gives a very good result in relieving inflammation and reducing adenoid vegetations to physiological norms. This allows you to preserve the adenoids and subsequently monitor their condition over time.
This in no way means that one course of therapy will be enough to prevent exacerbations of chronic adenoiditis. A child who is in contact with other people, especially if he attends a kindergarten, if he is re-infected, will go through an exacerbation of adenoiditis again and, of course, it would be right to come for a consultation with an ENT doctor and choose a new course of treatment. But against the background of professional treatment, firstly, the size of the adenoids will return to their normal age, the symptoms will be completely relieved, the child will breathe well through the nose in the intervals between diseases, the auditory tubes will function, and hearing will be preserved. The number and duration of courses of drug therapy will be reduced, including the number of antibiotics taken by the child. Taking into account the immunomodulating and preventive effect of physical therapy, the child will get sick much less often and the intervals of health will increase significantly. This means that complications will not form and surgery will be avoided.
Prevention of exacerbations of chronic adenoiditis and adenoid hypertrophy:
Many of the physiotherapeutic treatment methods (laser therapy with red and infrared lasers; orange photochromotherapy; magnetic therapy; halo-chamber) are used against the background of complete health without exacerbation, for the prevention of chronic adenoiditis and adenoid hypertrophy. They have extensive experience in using it with a proven effect of reducing morbidity in frequently ill children. Wherein:
- adenoid vegetations decrease in size;
- antibacterial, antiviral and antifungal effect allows you to maintain the normal microflora of the nasopharynx, suppressing the growth of pathogenic microflora;
- immunomodulating effect (stimulates the production of interferon, immunoglobulins, antibodies) increases the protective function of the mucous membrane;
- anti-inflammatory effect, relieves the manifestations of chronic inflammation;
- Magnetic therapy also affects the hypothalamus region, regulating and normalizing the functioning of the endocrine and nervous systems (balances the production of hormones, which is disturbed in frequently ill children)
A preventive course of therapy is prescribed by an ENT doctor and is carried out during the remission stage or against the background of full health at least 2 times a year. Preventive courses of treatment are recommended not only for children with an established diagnosis of Chronic adenoiditis and adenoid hypertrophy, but also for children at risk: first of all, these are children of preschool and early school age attending preschool and school educational institutions; sections and circles; crowded places (cinema, theater, circus, shopping and entertainment complexes).